Pulmonary aspiration
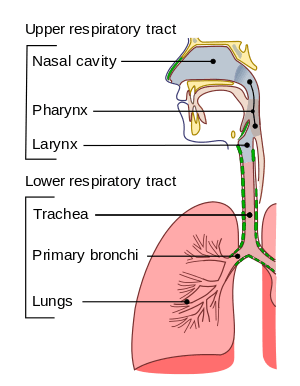
Pulmonary aspiration is the entry of material such as pharyngeal secretions, food or drink, or stomach contents from the oropharynx or gastrointestinal tract, into the larynx (voice box) and lower respiratory tract, the portions of the respiratory system from the trachea (windpipe) to the lungs. A person may inhale the material, or it may be delivered into the tracheobronchial tree during positive pressure ventilation. When pulmonary aspiration occurs during eating and drinking, the aspirated material is often colloquially referred to as "going down the wrong pipe."
| Pulmonary aspiration | |
|---|---|
 | |
| Upper gastrointestinal series at the level of the esophagus, showing pulmonary aspiration of the radiocontrast agent | |
| Specialty | Pulmonology |
Consequences of pulmonary aspiration range from no injury at all, to chemical pneumonitis or pneumonia, to death within minutes from asphyxiation. These consequences depend on the volume, chemical composition, particle size, and presence of infectious agents in the aspirated material, and on the underlying health status of the person.
In healthy people, aspiration of small quantities of material is common and rarely results in disease or injury. People with significant underlying disease or injury are at greater risk for developing respiratory complications following pulmonary aspiration, especially hospitalized patients, because of certain factors such as depressed level of consciousness and impaired airway defenses (gag reflex and respiratory tract antimicrobial defense system). The lumen of the right main bronchus is more vertical and slightly wider than that of the left, so aspirated material is more likely to end up in this bronchus or one of its subsequent bifurcations.
About 3.6 million cases of pulmonary aspiration or foreign body in the airway occurred in 2013.[1]
Presentation
Consequences

Particle-related
Pulmonary aspiration of particulate matter may result in acute airway obstruction which may rapidly lead to death from arterial hypoxemia.[2]
Acid-related
Pulmonary aspiration of acidic material (such as stomach acid) may produce an immediate primary injury caused by the chemical reaction of acid with lung parenchyma, and a later secondary injury as a result of the subsequent inflammatory response.[2]
Bacterial
Pulmonary aspiration may be followed by bacterial pneumonia. Community-acquired aspiration pneumonia is usually caused by anaerobic bacteria, whereas hospital-acquired aspiration pneumonia is more often caused by mixed flora, including both aerobic and anaerobic bacteria.[2]
Death
Pulmonary aspiration resulting in pneumonia, in some patients, particularly those with physical limitations, can be fatal.
Risk factors
Risk factors for pulmonary aspiration include conditions which depress the level of consciousness (such as traumatic brain injury, alcohol intoxication, drug overdose, and general anesthesia).[3] A decreased gag reflex, upper esophageal sphincter and lower esophageal sphincter tone, gastroesophageal reflux, full stomach, as well as obesity, stroke, and pregnancy can all increase the risk of aspiration in the semiconscious. Tracheal intubation or presence of a gastric tube (for example, a feeding tube) may also increase the risk.[4]
Prevention
The lungs are normally protected against aspiration by a series of protective reflexes such as coughing and swallowing. Significant aspiration can only occur if the protective reflexes are absent or severely diminished (in neurological disease, coma, drug overdose, sedation or general anesthesia). In intensive care, sitting patients up reduces the risk of pulmonary aspiration and ventilator-associated pneumonia.
Measures to prevent aspiration depend on the situation and the patient. In patients at imminent risk of aspiration, tracheal intubation by a trained health professional provides the best protection. A simpler intervention that can be implemented is to lay the patient on their side in the recovery position (as taught in first aid and CPR classes), so that any vomitus produced by the patient will drain out their mouth instead of back down their pharynx. Some anesthetists will use sodium citrate to neutralize the stomach's low pH and metoclopramide or domperidone (pro-kinetic agents) to empty the stomach.
People with chronic neurological disorders, for example, after a stroke, are less likely to aspirate thickened fluids on an instrumental swallowing assessment. However, this does not necessarily translate into reduced risk of pneumonia in real life eating and drinking.[5] Also, pharyngeal residue is more common with very thickened fluids: this may subsequently be aspirated and lead to a more severe pneumonia.[6]
The location of abscesses caused by aspiration depends on the position one is in. If one is sitting or standing up, the aspirate ends up in the posterior basal segment of the right lower lobe. If one is on one's back, it goes to the superior segment of the right lower lobe. If one is lying on the right side, it goes to the posterior segment of the right upper lobe, or the posterior basal segment of the right upper lobe. If one is lying on the left, it goes to the lingula.
References
- Vos, Theo; Barber, Ryan M; Bell, Brad; Bertozzi-Villa, Amelia; Biryukov, Stan; Bolliger, Ian; Charlson, Fiona; Davis, Adrian; Degenhardt, Louisa; Dicker, Daniel; Duan, Leilei; Erskine, Holly; Feigin, Valery L; Ferrari, Alize J; Fitzmaurice, Christina; Fleming, Thomas; Graetz, Nicholas; Guinovart, Caterina; Haagsma, Juanita; Hansen, Gillian M; Hanson, Sarah Wulf; Heuton, Kyle R; Higashi, Hideki; Kassebaum, Nicholas; Kyu, Hmwe; Laurie, Evan; Liang, Xiofeng; Lofgren, Katherine; Lozano, Rafael; et al. (2015). "Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013". The Lancet. 386 (9995): 743–800. doi:10.1016/s0140-6736(15)60692-4. PMC 4561509. PMID 26063472.
- Engelhardt, T.; Webster, N. R. (1999). "Pulmonary aspiration of gastric contents in anaesthesia". British Journal of Anaesthesia. 83 (3): 453–60. doi:10.1093/bja/83.3.453. PMID 10655918.
- Huxley, Eliot J.; Viroslav, Jose; Gray, William R.; Pierce, Alan K. (1978). "Pharyngeal aspiration in normal adults and patients with depressed consciousness". The American Journal of Medicine. 64 (4): 564–8. doi:10.1016/0002-9343(78)90574-0. PMID 645722.
- Gomes, Guilherme F.; Pisani, Julio C.; MacEdo, Evaldo D.; Campos, Antonio C. (2003). "The nasogastric feeding tube as a risk factor for aspiration and aspiration pneumonia". Current Opinion in Clinical Nutrition and Metabolic Care. 6 (3): 327–33. doi:10.1097/01.mco.0000068970.34812.8b. PMID 12690267.
- O'Keeffe ST. (July 2018). Use of modified diets to prevent aspiration in oropharyngeal dysphagia: is current practice justified? BMC Geriatrics. 2018;18:167 https://doi.org/10.1186/s12877-018-0839-7
- Robbins J, Gensler G, Hind J, Logemann JA, Lindblad AS, Brandt D, et al. Comparison of 2 interventions for fluid aspiration on pneumonia incidence: a randomised trial. Ann Intern Med. 2008;148:509–18.
Further reading
- Levy, D M (2006). "Pre-operative fasting—60 years on from Mendelson". Continuing Education in Anaesthesia, Critical Care & Pain. 6 (6): 215–8. doi:10.1093/bjaceaccp/mkl048.
- Mendelson, C. L. (1946). "The aspiration of stomach contents into the lungs during obstetric anesthesia". American Journal of Obstetrics and Gynecology. 52 (2): 191–205. doi:10.1016/S0002-9378(16)39829-5. PMID 20993766.
External links
| Classification |
|---|