Calcium pyrophosphate dihydrate crystal deposition disease
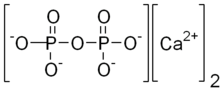
Calcium pyrophosphate dihydrate (CPPD) crystal deposition disease, also known as pseudogout and pyrophosphate arthropathy, is a rheumatologic disease which is thought to be secondary to abnormal accumulation of calcium pyrophosphate dihydrate crystals within joint soft tissues.[1] The knee joint is most commonly affected.[2]
| Calcium pyrophosphate dihydrate disease | |
|---|---|
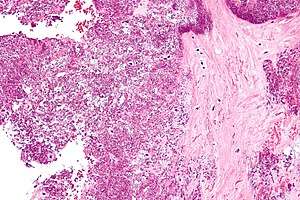 | |
| Micrograph showing crystal deposition in an intervertebral disc. H&E stain |
Signs and symptoms
When symptomatic, the disease classically begins with symptoms which are similar to a gout attack (thus the monicker "pseudogout"). These include:
- severe pain
- warmth
- swelling of one or more joints
The symptoms can be monoarticular (involving a single joint) or polyarticular (involving several joints).[1] Symptoms usually last for days to weeks, and often recur. Although any joint may be affected, the knees, wrists, and hips are most common.[3]
X-ray, CT, or other imaging usually shows accumulation of calcium within the joint cartilage, known as chondrocalcinosis. There can also be findings of osteoarthritis.[4][3] The white blood cell count is often raised.[3]
In many instances, patients may also have signs of carpal tunnel syndrome.[3] This condition can also be associated with Milwaukee shoulder syndrome.
Cause
The cause of CPPD disease is unknown. Increased breakdown of adenosine triphosphate (ATP; the molecule used as energy currency in all living things), which results in increased pyrophosphate levels in joints, is thought to be one reason why crystals may develop.[3]
Familial forms are rare.[5] One genetic study found an association between CPPD and a region of chromosome 8q.[6]
The gene ANKH is involved in crystal-related inflammatory reactions and inorganic phosphate transport.[4][3]
Diagnosis
The disease is defined by presence of joint inflammation and the presence of CPPD crystals within the joint. The crystals are usually detected by imaging and/or joint fluid analysis.

Medical imaging, consisting of x-ray, CT, MRI, or ultrasound may detect chondrocalcinosis within the affected joint, indicating a substantial amount of calcium crystal deposition within the cartilage or ligaments.[2] Ultrasound is a reliable method to diagnose CPPD.[7] Using ultrasound, chondrocalcinosis may be depicted as echogenic foci with no acoustic shadow within the hyaline cartilage[8] or fibrocartilage.[7] By x-ray, CPPD can appear similar to other diseases such as ankylosing spondylitis and gout.[2][3]

Arthrocentesis, or removing synovial fluid from the affected joint, is performed to test the synovial fluid for the calcium pyrophosphate crystals that are present in CPPD. When stained with H&E stain, calcium pyrophosphate crystals appears deeply blue ("basophilic").[9][10] However, CPP crystals are much better known for their rhomboid shape and weak positive Birefringence on polarized light microscopy, and this method remains the most reliable method of identifying the crystals under the microscope.[11] However, even this method suffers from poor sensitivity, specificity, and inter-operator agreement.[11]
These two modalities currently define CPPD disease, but lack diagnostic accuracy.[12] Thus, the diagnosis of CPPD disease is potentially epiphenomenological.
Treatment
Because any medication that could reduce the inflammation of CPPD bears a risk of causing organ damage, treatment is not advised if the condition is not causing pain.[3] For acute pseudogout, treatments include intra-articular corticosteroid injection, systemic corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs), or, on occasion, high-dose colchicine.[3] In general, NSAIDs are administered in low doses to help prevent CPPD. However, if an acute attack is already occurring, higher doses are administered.[3] If nothing else works, hydroxychloroquine or methotrexate may provide relief.[13] Research into surgical removal of calcifications is underway, however this still remains an experimental procedure.[3]
Epidemiology
The condition is more common in older adults.[4]
CPPD is estimated to affect 4% to 7% of the adult populations of Europe and the United States.[14] Previous studies have overestimated the prevalence by simply estimating the prevalence of chondrocalcinosis, which is found in many other conditions as well.[14]
It may cause considerable pain, but it is never fatal.[3] Women are at a slightly higher risk than men, with an estimated ratio of occurrence of 1.4:1.[3]
History
CPPD crystal deposition disease was originally described over 50 years ago.[12]
Terminology
Calcium pyrophosphate dihydrate crystals are associated with a range of clinical syndromes, which have been given various names, based upon which clinical symptoms or radiographic findings are most prominent.[12] A task force of the European League Against Rheumatism (EULAR) made recommendations on preferred terminology.[5] Accordingly, calcium pyrophosphate deposition (CPPD) is an umbrella term for the various clinical subsets, whose naming reflects an emphasis on particular features. For example, pseudogout refers to the acute symptoms of joint inflammation or synovitis: red, tender, and swollen joints that may resemble gouty arthritis (a similar condition in which monosodium urate crystals are deposited within the joints). Chondrocalcinosis,[2][3] on the other hand, refers to the radiographic evidence of calcification in hyaline and/or fibrocartilage. "Osteoarthritis (OA) with CPPD" reflects a situation where osteoarthritis features are the most apparent. Pyrophosphate arthropathy refers to several of these situations.[15]
References
- Wright GD, Doherty M (1997). "Calcium pyrophosphate crystal deposition is not always 'wear and tear' or aging". Ann. Rheum. Dis. 56 (10): 586–8. doi:10.1136/ard.56.10.586. PMC 1752269. PMID 9389218.
- Rothschild, Bruce M Calcium Pyrophosphate Deposition Disease (radiology)
- Rothschild, Bruce M Calcium Pyrophosphate Deposition Disease (rheumatology) at eMedicine
- Tsui FW (Apr 2012). "Genetics and mechanisms of crystal deposition in calcium pyrophosphate deposition disease". Curr Rheumatol Rep. 14 (2): 155–60. doi:10.1007/s11926-011-0230-6. PMID 22198832.
- Zhang W, Doherty M, Bardin T, Barskova V, Guerne PA, Jansen TL, Leeb BF, Perez-Ruiz F, Pimentao J, Punzi L, Richette P, Sivera F, Uhlig T, Watt I, Pascual E. European League Against Rheumatism recommendations for calcium pyrophosphate deposition. Part I: terminology and diagnosis. Ann Rheum Dis. 2011;70(4):563.
- Baldwin CT, Farrer LA, Adair R, Dharmavaram R, Jimenez S, Anderson L (March 1995). "Linkage of early-onset osteoarthritis and chondrocalcinosis to human chromosome 8q". Am. J. Hum. Genet. 56 (3): 692–7. PMC 1801178. PMID 7887424.
- Filippou, G.; Adinolfi, A.; Iagnocco, A.; Filippucci, E.; Cimmino, M.A.; Bertoldi, I.; Di Sabatino, V.; Picerno, V.; Delle Sedie, A.; Sconfienza, L.M.; Frediani, B. (June 2016). "Ultrasound in the diagnosis of calcium pyrophosphate dihydrate deposition disease. A systematic literature review and a meta-analysis". Osteoarthritis and Cartilage. 24 (6): 973–981. doi:10.1016/j.joca.2016.01.136.
- Arend CF. Ultrasound of the Shoulder. Master Medical Books, 2013. Free chapter on acromioclavicular chondrocalcinosis is available at ShoulderUS.com
- Hosler, Greg. "calcinosis_cutis_2_060122". Derm Atlas. Archived from the original on 5 February 2007. Retrieved 13 March 2012.
- "Calcium Pyrophosphate Dihydrate Deposition Disease: Synovial Biopsy, Wrist". Rheumatology Image Bank. American College of Rheumatology. Retrieved 13 March 2012.
- Dieppe, P.; Swan, A. (1 May 1999). "Identification of crystals in synovial fluid". Annals of the Rheumatic Diseases. 58 (5): 261–3. doi:10.1136/ard.58.5.261. PMC 1752883. PMID 10225806.
- Rosenthal, AK; Ryan, LM (May 2011). "Crystal arthritis: Calcium pyrophosphate deposition—nothing 'pseudo' about it!". Nat Rev Rheumatol. 7 (5): 257–8. doi:10.1038/nrrheum.2011.50. PMID 21532639.
- Emkey GR, Reginato AM (2009). "All about gout and pseudogout". Journal of Musculoskeletal Medicine. 26 (10).
- Ann K. Rosenthal. "Clinical manifestations and diagnosis of calcium pyrophosphate crystal deposition (CPPD) disease". UpToDate. This topic last updated: Jul 24, 2018.
- Longmore, Murray; Ian Wilkinson; Tom Turmezei; Chee Kay Cheung (2007). Oxford Handbook of Clinical Medicine. Oxford. p. 841. ISBN 978-0-19-856837-7.
External links
| Classification | |
|---|---|
| External resources |