Biological functions of nitric oxide
Nitric oxide (nitrogen monoxide) is a molecule and chemical compound with chemical formula of NO. In mammals including humans, nitric oxide is a signaling molecule involved in many physiological and pathological processes.[1] It is a powerful vasodilator with a half-life of a few seconds in the blood. Standard pharmaceuticals such as nitroglycerine and amyl nitrite are precursors to nitric oxide. Low levels of nitric oxide production are typically due to ischemic damage in the liver.
As a consequence of its importance in neuroscience, physiology, and immunology, nitric oxide was proclaimed "Molecule of the Year" in 1992.[2] Research into its function led to the 1998 Nobel Prize for elucidating the role of nitric oxide as a cardiovascular signalling molecule.
Sources of nitric oxide
Nitric oxide biosynthesis
Platelet-derived factors, shear stress, acetylcholine, and cytokines stimulate the production of NO by endothelial nitric oxide synthase (eNOS). eNOS synthesizes NO from the terminal guanidine-nitrogen of L-arginine and oxygen and yields citrulline as a byproduct. NO production by eNOS is dependent on calcium-calmodulin and other cofactors.
Nitric oxide synthases (NOSs) synthesize the metastable free radical nitric oxide (NO). Three isoforms are known for the NOS enzyme: endothelial (eNOS), neuronal (nNOS), and inducible (iNOS) - each with separate functions. The neuronal enzyme (NOS-1) and the endothelial isoform (NOS-3) are calcium-dependent and produce low levels of this gas as a cell signaling molecule. The inducible isoform (NOS-2) is calcium-independent and produces large amounts of gas that can be cytotoxic.
NOS oxidizes the guanidine group of L-arginine in a process that consumes five electrons and results in the formation of NO with stoichiometric formation of L-citrulline. The process involves the oxidation of NADPH and the reduction of molecular oxygen. The transformation occurs at a catalytic site adjacent to a specific binding site of L-arginine.[3] NO is an important regulator and mediator of numerous processes in the nervous, immune, and cardiovascular systems. These include vascular smooth muscle relaxation, resulting in arterial vasodilation and increasing blood flow.[4] NO is also a neurotransmitter and has been associated with neuronal activity and various functions such as avoidance learning. NO also partially mediates macrophage cytotoxicity against microbes and tumor cells. Besides mediating normal functions, NO is implicated in pathophysiologic states as diverse as septic shock, hypertension, stroke, and neurodegenerative diseases.[5]

Exogenous NO (NO-delivery drugs)
Exogenous NO sources constitute a powerful way to supplement NO when the body cannot generate enough for normal biological functions.[7] Certain endogenous compounds can act as NO-donors or elicit NO-like reactions in vivo. Nitroglycerin and amyl nitrite serve as vasodilators because they are converted to nitric oxide in the body. The vasodilating antihypertensive drug minoxidil contains an ·NO moiety and may act as an NO agonist. Likewise, Sildenafil citrate, popularly known by the trade name Viagra, stimulates erections primarily by enhancing signaling through the nitric oxide pathway. Prominent examples are S-nitrosothiols, certain organic nitrates, nitrosylated metal complexes, dinitrosyl iron complexes (DNIC), and even nitrite anions (NO2− ) under hypoxic conditions [8][9]
A high salt intake attenuates NO production in patients with essential hypertension, although bioavailability remains unregulated.[10]
Other, including dietary
Dietary nitrate is also an important source of nitric oxide in mammals. Green, leafy vegetables and some root vegetables (such as beetroot) have high concentrations of nitrate.[11] When eaten and absorbed into the bloodstream, nitrate is concentrated in saliva (about 10-fold) and is reduced to nitrite on the surface of the tongue by a biofilm of commensal facultative anaerobic bacteria.[12] This nitrite is swallowed and reacts with acid and reducing substances in the stomach (such as ascorbate) to produce high concentrations of nitric oxide. The purpose of this mechanism to create NO is thought to be both sterilization of swallowed food (to prevent food poisoning) and to maintain gastric mucosal blood flow.[13]
The nitrate-nitrite-nitric oxide pathway elevates nitric oxide through the sequential reduction of dietary nitrate derived from plant-based foods.[14] Nitrate-rich vegetables, in particular leafy greens, such as spinach and arugula, and beetroot, have been shown to increase cardioprotective levels of nitric oxide with a corresponding reduction in blood pressure in pre-hypertensive persons.[15][16] For the body to generate nitric oxide through the nitrate-nitrite-nitric oxide pathway, the reduction of nitrate to nitrite (by nitrate reductase, a bacterial enzyme) occurs in the mouth, by commensal bacteria, an obligatory and necessary step.[17] Monitoring nitric oxide status by saliva testing detects the bioconversion of plant-derived nitrate into nitric oxide. A rise in salivary levels is indicative of diets rich in leafy vegetables which are often abundant in anti-hypertensive diets such as the DASH diet.[18]
A related mechanism is thought to protect the skin from fungal infections, where nitrate in sweat is reduced to nitrite by skin commensal organisms and then to NO on the slightly acidic skin surface. In alternative fashion, nitrite anions on sun-exposed skin may be photolyzed to free nitric oxide radicals by UVA in sunlight.[19] This mechanism may elicit significant changes to the systemic blood circulation in humans and be exploited for therapeutic purposes.[20]
Nasal breathing also produces nitric oxide within the body.[21][22][23][24]
Immune response
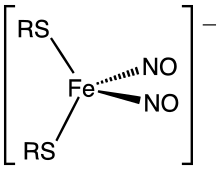
Nitric oxide is generated by phagocytes (monocytes, macrophages, and neutrophils) as part of the human immune response.[26] Phagocytes are armed with inducible nitric oxide synthase (iNOS), which is activated by interferon-gamma (IFN-γ) as a single signal or by tumor necrosis factor (TNF) along with a second signal.[27][28][29] On the other hand, transforming growth factor-beta (TGF-β) provides a strong inhibitory signal to iNOS, whereas interleukin-4 (IL-4) and IL-10 provide weak inhibitory signals. In this way, the immune system may regulate the armamentarium of phagocytes that play a role in inflammation and immune responses.[30] Nitric oxide is secreted as free radicals in an immune response and is toxic to bacteria and intracellular parasites, including Leishmania[31] and malaria;[32][33][34] the mechanism for this includes DNA damage[35][36][37] and degradation of iron sulfur centers into iron ions and iron-nitrosyl compounds.[38]
The inducible pathway (iNOS) of nitrogen oxide synthesis in phagocytes can generate large amounts of NO that trigger apoptosis and kill other cells. In vitro studies indicate that phagocyte-dependent generation of NO at concentrations greater than 400-500 nM triggers apoptosis in nearby cells and that this effect may act in a manner similar to Specialized pro-resolving mediators to dampen and reverse inflammatory responses by neutralizing and then speeding the clearance of pro-inflammatory cells from inflamed tissues.[39] However, the role of ·NO in inflammation is complex with model studies involving viral infection suggesting that this gaseous mediator can also promote inflammation.[40]
In response, many bacterial pathogens have evolved mechanisms for nitric oxide resistance.[41] Because nitric oxide might serve as an inflammometer (meter of inflammation) in conditions like asthma, interest has increased in the use of exhaled nitric oxide as a breath test in diseases with airway inflammation. Reduced levels of exhaled NO have been associated with exposure to air pollution in cyclists and smokers, but, in general, increased levels of exhaled nitric oxide are associated with exposure to air pollution.[42]
Molecular effects of NO on biological systems
In cells, two broad classes of reactions of nitric oxide involve the S-nitrosation of thiols and the nitrosylation of some metalloenzymes.
S-nitrosation of thiols
S-nitrosation involves the (reversible) conversion of thiol groups, including cysteine residues in proteins, to form S-nitrosothiols (RSNOs). S-Nitrosation is a mechanism for dynamic, post-translational regulation of most or all major classes of protein.[43]
Nitrosylation of metal centers, especially iron
Nitric oxide to a transition metal ion like iron or copper, forming metal nitrosyl complexes. Typical cases involve the nitrosylation of heme proteins like cytochromes, thereby disabling the normal enzymatic activity of the enzyme. Nitrosylated ferrous iron is particularly stable. Hemoglobin is a prominent example of a heme protein that may be modified by NO by both direct attack by NO and, independently, via attack by S-nitrosothiols, involving NO transfer from S to Fe.[44]
The iron-containing proteins ribonucleotide reductase and aconitase are deactivated by NO.[45] NO has been demonstrated to activate NF-κB in peripheral blood mononuclear cells, a transcription factor in iNOS gene expression in response to inflammation.[46]
Guanylate cyclase
Although NO affects many metalloproteins, it does so by deactivating them.
Guanylate cyclase is a key component of the famous smooth-muscle relaxing properties of NO. It is a heme-containing enzyme that is acted on by NO, which binds to the heme.[47] Cyclic-GMP activates protein kinase G, which causes reuptake of Ca2+ and the opening of calcium-activated potassium channels. The fall in concentration of Ca2+ ensures that the myosin light-chain kinase (MLCK) can no longer phosphorylate the myosin molecule, thereby stopping the crossbridge cycle and leading to relaxation of the smooth muscle cell.[48]
Smooth muscles
Vasodilation
Nitric oxide dilates blood vessels, raising blood supply and lowering blood pressure.[49] Conversely, it helps protect tissues from damage due to low blood supply.[49] Also a neurotransmitter, nitric oxide acts in the nitrergic neurons active on smooth muscle, abundant in the gastrointestinal tract and erectile tissue.[50] Sildenafil (Viagra) works to inhibit the enzyme phosphodiesterase PDE5, which increases the cGMP concentration by inhibiting the conversion to GMP.
Nitric oxide (NO) contributes to vessel homeostasis by inhibiting vascular smooth muscle contraction and growth, platelet aggregation, and leukocyte adhesion to the endothelium. Humans with atherosclerosis, diabetes, or hypertension often show impaired NO pathways.[51]
Nitric oxide (NO) is a mediator of vasodilation in blood vessels. It is induced by several factors, and once synthesized by eNOS it results in phosphorylation of several proteins that cause smooth muscle relaxation.[4] The vasodilatory actions of nitric oxide play a key role in renal control of extracellular fluid homeostasis and is essential for the regulation of blood flow and blood pressure.[52] NO also plays a role in erection of the penis and clitoris.[53]
Cardiac effects
Nitric oxide also acts on cardiac muscle to decrease contractility and heart rate. NO contributes to the regulation of cardiac contractility. Emerging evidence suggests that coronary artery disease (CAD) is related to defects in generation or action of NO.[54] Reduced levels of exhaled NO have been associated with exposure to traffic related air pollution.[42]
Effects on plants
In plants, nitric oxide can be produced by any of four routes: (i) L-arginine-dependent nitric oxide synthase,[55][56][57] (although the existence of animal NOS homologs in plants is debated),[58] (ii) plasma membrane-bound nitrate reductase, (iii) mitochondrial electron transport chain, or (iv) non-enzymatic reactions. It is a signaling molecule, acts mainly against oxidative stress and also plays a role in plant pathogen interactions. Treating cut flowers and other plants with nitric oxide has been shown to lengthen the time before wilting.[59][60]
In plants, NO also regulates some plant-pathogen interaction, promotion of the plant hypersensitive response, symbiosis (for example, with organisms in nitrogen-fixing root nodules), development of lateral and adventitious roots and root hairs, and control of stomatal opening. Nitric oxide is known to be produced by cellular organelles, including mitochondria, peroxisomes, and chloroplasts. It plays a role in antioxidant and reactive oxygen species responses.[61]
Nitric oxide sensing in plants is mediated by the N-end rule of proteolysis[62][63] and controls abiotic stress responses such as flooding-induced hypoxia,[64] salt and drought stress.[65]
Nitric oxide interactions have been found within signaling pathways of plant hormones such as auxin,[66] ethylene,[64][67][68] Abscisic acid [62] and cytokinin.[69]
Atmospheric nitric oxide can enter the stomates of most vascular species, and can have effects ranging from leaf blemishing, to stunting of growth, to necrosis.[70]
Effects in insects
Blood-sucking insects exploit vasodilation induced by NO to ensure their blood meal. These insects include Cimex lectularius (bed bug) and Rhodnius proxlixus (kissing bug). These insects deliver NO from its carrier nitrophorin carrier, which is in their saliva.[6]
Effects in bacteria
While nitric oxide is typically known to halt bacterial growth as part of an immune response, in one case NO protects a bacterium. The bacterium Deinococcus radiodurans can withstand extreme levels of radioactivity and other stresses. In 2009 it was reported that nitric oxide plays an important role in this bacteria's recovery from radiation exposure: The gas is required for division and proliferation after DNA damage has been repaired. A gene that increases nitric oxide production after UV radiation was described, and in the absence of this gene the bacteria were still able to repair DNA damage, but would not grow.[71]
Medical uses
| Clinical data | |
|---|---|
| Trade names | Inomax, Noxivent, Genosyl |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Pregnancy category | |
| Routes of administration | Inhalation |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | NO |
| Molar mass | 30.006 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
In the European Union nitric oxide in conjunction with ventilatory support and other appropriate active substances, is indicated:[73]
- for the treatment of newborn infants ≥34 weeks gestation with hypoxic respiratory failure associated with clinical or echocardiographic evidence of pulmonary hypertension, in order to improve oxygenation and to reduce the need for extracorporeal membrane oxygenation;[73]
- as part of the treatment of peri- and post-operative pulmonary hypertension in adults and newborn infants, infants and toddlers, children and adolescents, ages 0–17 years in conjunction to heart surgery, in order to selectively decrease pulmonary arterial pressure and improve right ventricular function and oxygenation.[73]
In the United States it is indicated to improve oxygenation and reduce the need for extracorporeal membrane oxygenation in term and near-term (>34 weeks gestation) neonates with hypoxic respiratory failure associated with clinical or echocardiographic evidence of pulmonary hypertension in conjunction with ventilatory support and other appropriate agents.[74]
The most common side effects include thrombocytopenia (low blood platelet counts), hypokalaemia (low blood potassium levels), hypotension (low blood pressure), atelectasis (collapse of the whole, or part of a, lung), and hyperbilirubinaemia (high blood levels of bilirubin).[73]
Nitric oxide was approved for medical use in the United States in December 1999 and for medical use in the European Union in 2001.[75][73][74]
Associated problems
There are some associated complaints with utilization of nitric oxide in neonatal patients. Some of them include dose errors associated with the delivery system, headaches associated with environmental exposure of nitric oxide in hospital staff, hypotension associated with acute withdrawal of the drug, hypoxemia associated with acute withdrawal of the drug, and pulmonary edema in patients with CREST syndrome.
Contraindications
Inhaled nitric oxide is contraindicated in the treatment of neonates known to be dependent on right-to-left shunting of blood. This is as the nitric oxide decreases the pulmonary circulation's resistance by dilating pulmonary blood vessels. The increased pulmonary return increases pressure in the left atrium, causing closure of the foramen ovale and reducing the blood flow through the ductus arteriosus. Closing these shunts can kill neonates with heart malformations that rely on the right-to-left shunting of blood.
Dosage and strength
In the United States, nitric oxide is a gas available in concentrations of only 100 ppm and 800 ppm. Overdosage with inhaled nitric oxide will be seen by elevations in methemoglobin and pulmonary toxicities associated with inspired ·NO. Elevated NO may cause acute lung injury.
Fatty liver disease
Nitric oxide production is associated with nonalcoholic fatty liver disease (NAFLD) and is essential for hepatic lipid metabolism under starvation.[76]
Lung infection
Nitric oxide is a potential therapeutic intervention in acute and chronic lung infections.[77][78]
Mechanism of action
Nitric oxide is a compound produced by many cells of the body. It relaxes vascular smooth muscle by binding to the heme moiety of cytosolic guanylate cyclase, activating guanylate cyclase and increasing intracellular levels of cyclic-guanosine 3',5'-monophosphate, which then leads to vasodilation. When inhaled, nitric oxide dilates the pulmonary vasculature and, because of efficient scavenging by hemoglobin, has minimal effect on the vasculature of the entire body.[79]
Inhaled nitric oxide appears to increase the partial pressure of arterial oxygen (PaO2) by dilating pulmonary vessels in better-ventilated areas of the lung, moving pulmonary blood flow away from lung segments with low ventilation/perfusion (V/Q) ratios toward segments with normal or better ratios.[80]
Neonatal use
Nitric oxide/oxygen blends are used in critical care to promote capillary and pulmonary dilation to treat primary pulmonary hypertension in neonatal patients[81][82] and post-meconium aspiration related to birth defects. These are often a last-resort gas mixture before the use of extracorporeal membrane oxygenation (ECMO). Nitric oxide therapy has the potential to significantly increase the quality of life and, in some cases, save the lives of infants at risk for pulmonary vascular disease.[83]
Pathology
People with diabetes usually have lower levels of nitric oxide than patients without diabetes.[84] Diminished supply of nitric oxide can lead to vascular damage, such as endothelial dysfunction and vascular inflammation. Vascular damage can lead to decreased blood flow to the extremities, causing the diabetic patient to be more likely to develop neuropathy and non-healing ulcers, and to be at a greater risk for lower limb amputation.
Pediatric and adult use
The primary use is in the form of nitroglycerin, either pill or liquid spray forms, which, as a prodrug, is denitrated and releases the active metabolite nitric oxide (NO). As with all supplements of nitric oxide, the response is short-lived because, as a normally produced internal physiologic control mechanism, increased concentrations lead to increased rates of clearance, which is the reason that the effectiveness of sustained use of nitroglycerin for vasodilation fades to none after hours to days. In the United States, ongoing direct use of nitric oxide use is only approved for neonates. In the adult ICU setting, inhaled ·NO can improve hypoxemia in acute lung injury, acute respiratory distress syndrome, and severe pulmonary hypertension, although the effects are short-lived and there are no studies demonstrating improved clinical outcomes. It is used on an individualized basis in ICUs as an adjunct to other definitive therapies for reversible causes of hypoxemic respiratory distress.[85]
Pharmacokinetics
Nitric oxide is absorbed systemically after inhalation. Most of it moves across the pulmonary capillary bed where it combines with hemoglobin that is 60% to 100% oxygen-saturated.
Nitrate has been identified as the predominant nitric oxide metabolite excreted in the urine, accounting for >70% of the nitric oxide dose inhaled. Nitrate is cleared from the plasma by the kidney at rates approaching the rate of glomerular filtration.
Pharmacology
Nitric oxide is considered an antianginal drug: It causes vasodilation, which can help with ischemic pain, known as angina, by decreasing the cardiac workload. By dilating (expanding) the arteries, nitric oxide drugs lower arterial pressure and left ventricular filling pressure.[86] Nitric oxide can contribute to reperfusion injury when an excessive amount produced during reperfusion (following a period of ischemia) reacts with superoxide to produce the damaging oxidant peroxynitrite. In contrast, inhaled nitric oxide has been shown to help survival and recovery from paraquat poisoning, which produces lung tissue-damaging superoxide and hinders NOS metabolism.
This vasodilation does not decrease the volume of blood the heart pumps, but rather it decreases the force the heart muscle must exert to pump the same volume of blood. Nitroglycerin pills, taken sublingually (under the tongue), are used to prevent or treat acute chest pain. The nitroglycerin reacts with a sulfhydryl group (–SH) to produce nitric oxide, which eases the pain by causing vasodilation. There is a potential role for the use of nitric oxide in alleviating bladder contractile dysfunctions,[87][88] and recent evidence suggests that nitrates may be beneficial for treatment of angina due to reduced myocardial oxygen consumption both by decreasing preload and afterload and by some direct vasodilation of coronary vessels.[86]
Pulmonary embolism
Nitric oxide is also administered as salvage therapy in patients with acute right ventricular failure secondary to pulmonary embolism.[89]
Research
COVID‑19
As of April 2020, studies and trials are underway that examine the possible benefits of nitric oxide in the treatment of COVID‑19.[90][91][92][93] This research is based on the fact that nitric oxide was investigated as an experimental therapy for SARS.[94] Brian Strickland, MD, a fellow in Wilderness Medicine at Massachusetts General Hospital who studies "acute respiratory distress" in high altitudes, is applying this research towards COVID‑19.[95][96] He is involved in clinical trials which apply the use of inhaled nitric oxide as a treatment for COVID‑19.[97] This approach was inspired by the work of Associate Professor of Emergency Medicine at the Harvard Medical School N. Stuart Harris, who has been studying the effects of altitude sickness on mountain climbers, such as those who climb Mount Everest. Harris noticed that the consequences of high level altitude sickness on the human body mirrored COVID‑19's dysfunctional impact on the lungs. His focus on nitric oxide comes from its role in being able to breathe in high altitudes.[95][98] According to WCVB-TV, similar trials are being conducted at Tufts Medical Center.[99] Other studies speculate that replacing mouth breathing (which decimates NO) with nasal breathing (which increases NO)[21][22][23][24] is a "lifestyle change" that "may also help to reduce SARS-CoV-2 viral load and symptoms of COVID‑19 pneumonia by promoting more efficient antiviral defense mechanisms in the respiratory tract."[100]
References
- Hou, YC; Janczuk, A; Wang, PG (1999). "Current trends in the development of nitric oxide donors". Current Pharmaceutical Design. 5 (6): 417–41. PMID 10390607.
- Culotta, Elizabeth; Koshland, Daniel E. Jr (1992). "NO news is good news". Science. 258 (5090): 1862–1864. Bibcode:1992Sci...258.1862C. doi:10.1126/science.1361684. PMID 1361684.
- Ignarro L.J. (1990): Nitric Oxide. A Novel Signal Transduction Mechanism For Transcellular Communication; Hypertension; 16(5): 477-483.
- Weller, Richard, Could the sun be good for your heart? TedxGlasgow March 2012, posted January 2013
- Davies, S.A., Stewart, E.J., Huesmaan, G.R and Skaer, N. J. (1997): Neuropeptide stimulation of the nitric oxide signalling pathway in Drosophila melanogaster Malpighian tubules. Am. J. Physiol..; 273, R823-827.
- Walker, F. A. (2005). "Nitric Oxide Interaction with Insect Nitrophorins and Thoughts on the Electron Configuration of the FeNO6 complex". J. Inorg. Biochem. 99 (1): 216–236. doi:10.1016/j.jinorgbio.2004.10.009. PMID 15598503.
- Hou, Y.C.; Janczuk, A.; Wang, P.G. (1999). "Current trends in the development of nitric oxide donors". Curr. Pharm. Des. 5 (6): 417–471. PMID 10390607.
- Radicals for life: The various forms of nitric oxide. E. van Faassen and A. Vanin, eds. Elsevier, Amsterdam 2007. ISBN 978-0-444-52236-8.
- Nitrite as regulator of hypoxic signaling in mammalian physiology. Med Res Rev 29, 2009, 683 - 741
- Osanai, T; Fujiwara, N; Saitoh, M; Sasaki, S; Tomita, H; Nakamura, M; Osawa, H; Yamabe, H; Okumura, K (2002). "Relationship between salt intake, nitric oxide, and asymmetric dimethylarginine and its relevance to patients with end-stage renal disease". Blood Purification. 20 (5): 466–8. doi:10.1159/000063555. PMID 12207094. S2CID 46833231.
- Liu, A.H.; et al. (2013). "Effects of a nitrate-rich meal on arterial stiffness and blood pressure in healthy volunteers". Nitric Oxide : Biology and Chemistry. 35: 123–30. doi:10.1016/j.niox.2013.10.001. PMID 24120618.
- Lundberg, JO; Eddie Weitzberg, E; Gladwin, MT (2008). "The nitrate–nitrite–nitric oxide pathway in physiology and therapeutics". Nature Reviews Drug Discovery. 7 (2): 156–167. doi:10.1038/nrd2466. PMID 18167491. S2CID 5141850.
- Green, SJ (1995). "Nitric oxide in mucosal immunity". Nature Medicine. 1 (6): 515–517. doi:10.1038/nm0695-515. PMID 7585111. S2CID 36184793.
- "Plant-based Diets | Plant-based Foods | Beetroot Juice | Nitric Oxide Vegetables". Berkeley Test. Archived from the original on 2013-10-04. Retrieved 2013-10-04.
- Ghosh, S. M.; Kapil, V.; Fuentes-Calvo, I.; Bubb, K. J.; Pearl, V.; Milsom, A. B.; Khambata, R.; Maleki-Toyserkani, S.; Yousuf, M.; Benjamin, N.; Webb, A. J.; Caulfield, M. J.; Hobbs, A. J.; Ahluwalia, A. (2013). "Enhanced Vasodilator Activity of Nitrite in Hypertension: Critical Role for Erythrocytic Xanthine Oxidoreductase and Translational Potential". Hypertension. 61 (5): 1091–102. doi:10.1161/HYPERTENSIONAHA.111.00933. PMID 23589565.
- Webb, A. J.; Patel, N.; Loukogeorgakis, S.; Okorie, M.; Aboud, Z.; Misra, S.; Rashid, R.; Miall, P.; Deanfield, J.; Benjamin, N.; MacAllister, R.; Hobbs, A. J.; Ahluwalia, A. (2008). "Acute Blood Pressure Lowering, Vasoprotective, and Antiplatelet Properties of Dietary Nitrate via Bioconversion to Nitrite". Hypertension. 51 (3): 784–90. doi:10.1161/HYPERTENSIONAHA.107.103523. PMC 2839282. PMID 18250365.
- Hezel, MP; Weitzberg, E (2013). "The oral microbiome and nitric oxide homoeostasis". Oral Diseases. 21 (1): 7–16. doi:10.1111/odi.12157. PMID 23837897.
- Green, Shawn J. (2013-07-25). "Turning DASH Strategy into Reality for Improved Cardio Wellness Outcomes: Part II". Real World Health Care. Retrieved 2013-10-04.
- Suschek, C.; Opländer, C. (2010). "Nonenzymatic NO production in human skin: Effect of UVA on cutaneous NO stores". Nitric Oxide. 22 (2): 120–135. doi:10.1016/j.niox.2009.10.006. PMID 19879370.
- Opländer, C.; et al. (2012). "Dermal application of nitric oxide in vivo: Kinetics, biological responses and therapeutic potential in humans". Clin Pharmacol Ther. 91 (6): 1074–1082. doi:10.1038/clpt.2011.366. PMID 22549282.
- Glazier, M.D., Eve (2019-11-04). "'Nose breathing has more benefits than mouth breathing". The Times and Democrat. Retrieved 2020-07-09.
- Dahl, Melissa (2011-01-11). "'Mouth-breathing' gross, harmful to your health". NBC News. Retrieved 2020-06-28.
- Berman, Joe (2019-01-29). "Could nasal breathing improve athletic performance?". Washington Post. Retrieved 2020-05-31.
- Vinopal, Lauren (2019-07-19). "Undiagnosed Mouth Breathing Creates Unhealthy Kids". Fatherly. Retrieved 2020-05-31.
- Jessica Fitzpatrick; Eunsuk Kim (2015). "Synthetic Modeling Chemistry of Iron–Sulfur Clusters in Nitric Oxide Signaling". Acc. Chem. Res. 48 (8): 2453–2461. doi:10.1021/acs.accounts.5b00246. PMID 26197209.
- Green, SJ; Mellouk, S; Hoffman, SL; Meltzer, MS; Nacy, CA (1990). "Cellular mechanisms of nonspecific immunity to intracellular infection: Cytokine-induced synthesis of toxic nitrogen oxides from L-arginine by macrophages and hepatocytes". Immunology Letters. 25 (1–3): 15–9. doi:10.1016/0165-2478(90)90083-3. PMID 2126524.
- Gorczyniski and Stanely, Clinical Immunology. Landes Bioscience; Austin, TX. ISBN 1-57059-625-5
- Green, SJ; Nacy, CA; Schreiber, RD; Granger, DL; Crawford, RM; Meltzer, MS; Fortier, AH (1993). "Neutralization of gamma interferon and tumor necrosis factor alpha blocks in vivo synthesis of nitrogen oxides from L-arginine and protection against Francisella tularensis infection in Mycobacterium bovis BCG-treated mice". Infection and Immunity. 61 (2): 689–98. doi:10.1128/IAI.61.2.689-698.1993. PMC 302781. PMID 8423095.
- Kamijo, R; Gerecitano, J; Shapiro, D; Green, SJ; Aguet, M; Le, J; Vilcek, J (1995). "Generation of nitric oxide and clearance of interferon-gamma after BCG infection are impaired in mice that lack the interferon-gamma receptor". Journal of Inflammation. 46 (1): 23–31. PMID 8832969.
- Green, SJ; Scheller, LF; Marletta, MA; Seguin, MC; Klotz, FW; Slayter, M; Nelson, BJ; Nacy, CA (1994). "Nitric oxide: Cytokine-regulation of nitric oxide in host resistance to intracellular pathogens" (PDF). Immunology Letters. 43 (1–2): 87–94. doi:10.1016/0165-2478(94)00158-8. hdl:2027.42/31140. PMID 7537721.
- Green, SJ; Crawford, RM; Hockmeyer, JT; Meltzer, MS; Nacy, CA (1990). "Leishmania major amastigotes initiate the L-arginine-dependent killing mechanism in IFN-gamma-stimulated macrophages by induction of tumor necrosis factor-alpha". Journal of Immunology. 145 (12): 4290–7. PMID 2124240.
- Seguin, M. C.; Klotz, FW; Schneider, I; Weir, JP; Goodbary, M; Slayter, M; Raney, JJ; Aniagolu, JU; Green, SJ (1994). "Induction of nitric oxide synthase protects against malaria in mice exposed to irradiated Plasmodium berghei infected mosquitoes: Involvement of interferon gamma and CD8+ T cells". Journal of Experimental Medicine. 180 (1): 353–8. doi:10.1084/jem.180.1.353. PMC 2191552. PMID 7516412.
- Mellouk, S; Green, SJ; Nacy, CA; Hoffman, SL (1991). "IFN-gamma inhibits development of Plasmodium berghei exoerythrocytic stages in hepatocytes by an L-arginine-dependent effector mechanism". Journal of Immunology. 146 (11): 3971–6. PMID 1903415.
- Klotz, FW; Scheller, LF; Seguin, MC; Kumar, N; Marletta, MA; Green, SJ; Azad, AF (1995). "Co-localization of inducible-nitric oxide synthase and Plasmodium berghei in hepatocytes from rats immunized with irradiated sporozoites". Journal of Immunology. 154 (7): 3391–5. PMID 7534796.
- Wink, D.; Kasprzak, K.; Maragos, C.; Elespuru, R.; Misra, M; Dunams, T.; Cebula, T.; Koch, W.; Andrews, A.; Allen, J.; Et, al. (1991). "DNA deaminating ability and genotoxicity of nitric oxide and its progenitors". Science. 254 (5034): 1001–3. Bibcode:1991Sci...254.1001W. doi:10.1126/science.1948068. PMID 1948068.
- Nguyen, T.; Brunson, D.; Crespi, C. L.; Penman, B. W.; Wishnok, J. S.; Tannenbaum, S. R. (1992). "DNA Damage and Mutation in Human Cells Exposed to Nitric Oxide in vitro". Proceedings of the National Academy of Sciences. 89 (7): 3030–3034. Bibcode:1992PNAS...89.3030N. doi:10.1073/pnas.89.7.3030. PMC 48797. PMID 1557408. Free text.
- Li, Chun-Qi; Pang, Bo; Kiziltepe, Tanyel; Trudel, Laura J.; Engelward, Bevin P.; Dedon, Peter C.; Wogan, Gerald N. (2006). "Threshold Effects of Nitric Oxide-Induced Toxicity and Cellular Responses in Wild-Type and p53-Null Human Lymphoblastoid Cells". Chemical Research in Toxicology. 19 (3): 399–406. doi:10.1021/tx050283e. PMC 2570754. PMID 16544944. free text
- Hibbs, John B.; Taintor, Read R.; Vavrin, Zdenek; Rachlin, Elliot M. (1988). "Nitric oxide: A cytotoxic activated macrophage effector molecule". Biochemical and Biophysical Research Communications. 157 (1): 87–94. doi:10.1016/S0006-291X(88)80015-9. PMID 3196352.
- Wallace JL, Ianaro A, Flannigan KL, Cirino G (2015). "Gaseous mediators in resolution of inflammation". Seminars in Immunology. 27 (3): 227–33. doi:10.1016/j.smim.2015.05.004. PMID 26095908.
- Uehara EU, Shida Bde S, de Brito CA (2015). "Role of nitric oxide in immune responses against viruses: beyond microbicidal activity". Inflammation Research. 64 (11): 845–52. doi:10.1007/s00011-015-0857-2. PMID 26208702. S2CID 14587150.
- Janeway, C. A.; et al. (2005). Immunobiology: the immune system in health and disease (6th ed.). New York: Garland Science. ISBN 978-0-8153-4101-7.
- Jacobs, L; Nawrot, Tim S; De Geus, Bas; Meeusen, Romain; Degraeuwe, Bart; Bernard, Alfred; Sughis, Muhammad; Nemery, Benoit; Panis, Luc (Oct 2010). "Subclinical responses in healthy cyclists briefly exposed to traffic-related air pollution". Environmental Health. 9 (64): 64. doi:10.1186/1476-069X-9-64. PMC 2984475. PMID 20973949.
- van Faassen, E. and Vanin, A. (eds.) (2007) Radicals for life: The various forms of nitric oxide. Elsevier, Amsterdam, ISBN 978-0-444-52236-8
- van Faassen, E. and Vanin, A. (2004) "Nitric Oxide", in Encyclopedia of Analytical Science, 2nd ed., Elsevier, ISBN 0127641009.
- Shami, PJ; Moore, JO; Gockerman, JP; Hathorn, JW; Misukonis, MA; Weinberg, JB (1995). "Nitric oxide modulation of the growth and differentiation of freshly isolated acute non-lymphocytic leukemia cells". Leukemia Research. 19 (8): 527–33. doi:10.1016/0145-2126(95)00013-E. PMID 7658698.
- Kaibori M.; Sakitani K.; Oda M.; Kamiyama Y.; Masu Y.; Okumura T. (1999). "Immunosuppressant FK506 inhibits inducible nitric oxide synthase gene expression at a step of NF-κB activation in rat hepatocytes". J. Hepatol. 30 (6): 1138–1145. doi:10.1016/S0168-8278(99)80270-0. PMID 10406194.
- Derbyshire ER, Marletta MA (2009). Biochemistry of soluble guanylate cyclase. Handb. Exp. Pharmacol. Handbook of Experimental Pharmacology. 191. pp. 17–31. doi:10.1007/978-3-540-68964-5_2. ISBN 978-3-540-68960-7. PMID 19089323.
- Rhoades, RA; Tanner, GA (2003). Medical physiology 2nd edition.
- van Faassen, EE; Bahrami, S; Feelisch, M; Hogg, N; Kelm, M; et al. (Sep 2009). "Nitrite as regulator of hypoxic signaling in mammalian physiology". Med Res Rev. 29 (5): 683–741. doi:10.1002/med.20151. PMC 2725214. PMID 19219851.
- Toda, N; Ayajiki, K; Okamura, T (May 2005). "Nitric oxide and penile erectile function". Pharmacol Ther. 106 (2): 233–66. doi:10.1016/j.pharmthera.2004.11.011. PMID 15866322.
- Dessy, C.; Ferron, O. (2004). "Pathophysiological Roles of Nitric Oxide: In the Heart and the Coronary Vasculature". Current Medicinal Chemistry - Anti-Inflammatory & Anti-Allergy Agents. 3 (3): 207–216. doi:10.2174/1568014043355348.
- Yoon, Y.; Song, U.; Hong, S.H.; Kim, J.Q. (2000). "Plasma nitric oxide concentration and nitric oxide synthase gene polymorphism in coronary artery disease". Clin. Chem. 46 (10): 1626–1630. doi:10.1093/clinchem/46.10.1626.
- Gragasin, S.; Michelakis, D.; Hogan, A.; Moudgil, R.; Hashimoto, K.; Wu, X.; Bonnet, S.; Haromy, A.; Archer, L. (Sep 2004). "The neurovascular mechanism of clitoral erection: nitric oxide and cGMP-stimulated activation of BKCa channels". The FASEB Journal. 18 (12): 1382–1391. doi:10.1096/fj.04-1978com. ISSN 0892-6638. PMID 15333581.
- Navin, K.T.; Toshio, H.A.; Daigo, S.I.; Hatsuyo, K.; Hisako, M.; Taku, T.S.; Akihisa, A. (2002). "Anti-Atherosclerotic Effect of -Blocker with Nitric Oxide–Releasing Action on the Severe Atherosclerosis". J. Cardiovascular Pharmacology. 39 (2): 298–309. doi:10.1097/00005344-200202000-00017. PMID 11791016.
- Corpas, F. J.; Barroso, JB; Carreras, A; Quirós, M; León, AM; Romero-Puertas, MC; Esteban, FJ; Valderrama, R; Palma, JM; Sandalio, LM; Gómez, M; Del Río, LA (2004). "Cellular and subcellular localization of endogenous nitric oxide in young and senescent pea plants". Plant Physiology. 136 (1): 2722–33. doi:10.1104/pp.104.042812. PMC 523336. PMID 15347796.
- Corpas, F. J.; Barroso, Juan B.; Carreras, Alfonso; Valderrama, Raquel; Palma, José M.; León, Ana M.; Sandalio, Luisa M.; Del Río, Luis A (2006). "Constitutive arginine-dependent nitric oxide synthase activity in different organs of pea seedlings during plant development". Planta. 224 (2): 246–54. doi:10.1007/s00425-005-0205-9. PMID 16397797. S2CID 23329722.
- Valderrama, R.; Corpas, Francisco J.; Carreras, Alfonso; Fernández-Ocaña, Ana; Chaki, Mounira; Luque, Francisco; Gómez-Rodríguez, María V.; Colmenero-Varea, Pilar; Del Río, Luis A.; Barroso, Juan B. (2007). "Nitrosative stress in plants". FEBS Lett. 581 (3): 453–61. doi:10.1016/j.febslet.2007.01.006. PMID 17240373.
- Corpas, F. J.; Barroso, Juan B.; Del Rio, Luis A. (2004). "Enzymatic sources of nitric oxide in plant cells – beyond one protein–one function". New Phytologist. 162 (2): 246–7. doi:10.1111/j.1469-8137.2004.01058.x.
- Siegel-Itzkovich, J. (1999). "Viagra makes flowers stand up straight". BMJ. 319 (7205): 274. doi:10.1136/bmj.319.7205.274a. PMC 1126920. PMID 10426722.
- Mur, L. A.; Mandon, J.; Persijn, S.; Cristescu, S. M.; Moshkov, I. E.; Novikova, G. V.; Gupta, K. J. (2013). "Nitric oxide in plants: an assessment of the current state of knowledge". AoB PLANTS. 5: pls052. doi:10.1093/aobpla/pls052. PMC 3560241. PMID 23372921.
- Verma, K., Mehta, S. K., & Shekhawat, G. S. (2013). Nitric oxide (NO) counteracts cadmium induced cytotoxic processes mediated by reactive oxygen species (ROS) in Brassica juncea: cross-talk between ROS, NO and antioxidant responses. BioMetals: an international journal on the role of metal ions in biology, biochemistry, and medicine.
- Gibbs, DJ; Md Isa, N; Movahedi, M; Lozano-Juste, J; Mendiondo, GM; Berckhan, S; Marín-de la Rosa, N; Vicente Conde, J; Sousa Correia, C; Pearce, SP; Bassel, GW; Hamali, B; Talloji, P; Tomé, DF; Coego, A; Beynon, J; Alabadí, D; Bachmair, A; León, J; Gray, JE; Theodoulou, FL; Holdsworth, MJ (6 February 2014). "Nitric oxide sensing in plants is mediated by proteolytic control of group VII ERF transcription factors". Molecular Cell. 53 (3): 369–79. doi:10.1016/j.molcel.2013.12.020. PMC 3969242. PMID 24462115.
- León, J; Costa-Broseta, Á; Castillo, MC (13 February 2020). "RAP2.3 negatively regulates nitric oxide biosynthesis and related responses through a rheostat-like mechanism in Arabidopsis". Journal of Experimental Botany. 71 (10): 3157–3171. doi:10.1093/jxb/eraa069. PMID 32052059.
- Hartman, S; Liu, Z; van Veen, H; Vicente, J; Reinen, E; Martopawiro, S; Zhang, H; van Dongen, N; Bosman, F; Bassel, GW; Visser, EJW; Bailey-Serres, J; Theodoulou, FL; Hebelstrup, KH; Gibbs, DJ; Holdsworth, MJ; Sasidharan, R; Voesenek, LACJ (5 September 2019). "Ethylene-mediated nitric oxide depletion pre-adapts plants to hypoxia stress". Nature Communications. 10 (1): 4020. Bibcode:2019NatCo..10.4020H. doi:10.1038/s41467-019-12045-4. PMC 6728379. PMID 31488841.
- Vicente, J; Mendiondo, GM; Movahedi, M; Peirats-Llobet, M; Juan, YT; Shen, YY; Dambire, C; Smart, K; Rodriguez, PL; Charng, YY; Gray, JE; Holdsworth, MJ (23 October 2017). "The Cys-Arg/N-End Rule Pathway Is a General Sensor of Abiotic Stress in Flowering Plants". Current Biology. 27 (20): 3183–3190.e4. doi:10.1016/j.cub.2017.09.006. PMC 5668231. PMID 29033328.
- Terrile, M. C., París, R., Calderón‐Villalobos, L. I., Iglesias, M. J., Lamattina, L., Estelle, M., & Casalongué, C. A. (2012). Nitric oxide influences auxin signaling through S‐nitrosylation of the Arabidopsis TRANSPORT INHIBITOR RESPONSE 1 auxin receptor. The Plant Journal.
- Melo, NK; Bianchetti, RE; Lira, BS; Oliveira, PM; Zuccarelli, R; Dias, DL; Demarco, D; Peres, LE; Rossi, M; Freschi, L (April 2016). "Nitric Oxide, Ethylene, and Auxin Cross Talk Mediates Greening and Plastid Development in Deetiolating Tomato Seedlings". Plant Physiology. 170 (4): 2278–94. doi:10.1104/pp.16.00023. PMC 4825133. PMID 26829981.
- Zhang, L; Li, G; Wang, M; Di, D; Sun, L; Kronzucker, HJ; Shi, W (July 2018). "Excess iron stress reduces root tip zone growth through nitric oxide-mediated repression of potassium homeostasis in Arabidopsis". The New Phytologist. 219 (1): 259–274. doi:10.1111/nph.15157. PMID 29658100.
- Liu, W. Z.; Kong, D. D.; Gu, X. X.; Gao, H. B.; Wang, J. Z.; Xia, M.; He, Y. K. (2013). "Cytokinins can act as suppressors of nitric oxide in Arabidopsis". Proceedings of the National Academy of Sciences. 110 (4): 1548–1553. Bibcode:2013PNAS..110.1548L. doi:10.1073/pnas.1213235110. PMC 3557067. PMID 23319631.
- C.Michael Hogan. 2010. "Abiotic factor" Archived June 8, 2013, at the Wayback Machine. Encyclopedia of Earth. eds Emily Monosson and C. Cleveland. National Council for Science and the Environment. Washington DC
- Bhumit A. Patel; Magali Moreau; Joanne Widom; Huan Chen; Longfei Yin; Yuejin Hua; Brian R. Crane (2009). "Endogenous nitric oxide regulates the recovery of the radiation-resistant bacterium Deinococcus radiodurans from exposure to UV light". PNAS. 106 (43): 18183–18188. Bibcode:2009PNAS..10618183P. doi:10.1073/pnas.0907262106. PMC 2775278. PMID 19841256.
- "Nitric oxide Use During Pregnancy". Drugs.com. 21 November 2019. Retrieved 29 May 2020.
- "Inomax EPAR". European Medicines Agency (EMA). Retrieved 29 May 2020. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- "Inomax- nitric oxide gas". DailyMed. 25 February 2019. Retrieved 29 May 2020.
- "Drug Approval Package: Inomax (Nitric Oxide) NDA# 20-845". U.S. Food and Drug Administration (FDA). 31 March 2001. Retrieved 29 May 2020.
- Gu, Qilin; Yang, Xiaojie; Lin, Li; Li, Shaoyang; Li, Qing; Zhong, Shan; Peng, Jinrong; Cui, Zongbin (December 2014). "Genetic ablation of solute carrier family 7a3a leads to hepatic steatosis in zebrafish during fasting". Hepatology. 60 (6): 1929–1941. doi:10.1002/hep.27356. PMID 25130427.
- Fang, FC (October 2004). "Antimicrobial reactive oxygen and nitrogen species: concepts and controversies". Nature Reviews. Microbiology. 2 (10): 820–32. doi:10.1038/nrmicro1004. PMID 15378046. S2CID 11063073.
- Goldfarb, RD; Cinel, I (January 2007). "Inhaled nitric oxide therapy for sepsis: more than just lung". Critical Care Medicine. 35 (1): 290–2. doi:10.1097/01.CCM.0000251290.41866.2B. PMID 17197767.
- Kinsella JP, Cutter GR, Walsh WF, Gerstmann DR, Bose CL, Hart C, et al. (2006). "Early inhaled nitric oxide therapy in premature newborns with respiratory failure". N Engl J Med. 355 (4): 354–64. CiteSeerX 10.1.1.319.6088. doi:10.1056/NEJMoa060442. PMID 16870914.
- Ballard RA, Truog WE, Cnaan A, Martin RJ, Ballard PL, Merrill JD, et al. (2006). "Inhaled nitric oxide in preterm infants undergoing mechanical ventilation". N Engl J Med. 355 (4): 343–53. doi:10.1056/NEJMoa061088. PMID 16870913.
- Barrington, Keith J.; Finer, Neil; Pennaforte, Thomas; Altit, Gabriel (2017). "Nitric oxide for respiratory failure in infants born at or near term". The Cochrane Database of Systematic Reviews. 1: CD000399. doi:10.1002/14651858.CD000399.pub3. ISSN 1469-493X. PMC 6464941. PMID 28056166.
- Chotigeat U, Khorana M, Kanjanapattanakul W (2007). "Inhaled nitric oxide in newborns with severe hypoxic respiratory failure". J Med Assoc Thai. 90 (2): 266–71. PMID 17375630.
- Hayward, CS; Kelly, RP; MacDonald, PS (1999). "Inhaled nitric oxide in cardiology practice". Cardiovascular Research. 43 (3): 628–38. doi:10.1016/S0008-6363(99)00114-5. PMID 10690334.
- nfb University Studies - Nitric Oxide Holds Promise for Diabetes
- Mark J.D. Griffiths, M.R.C.P.; Timothy W. Evans, M.D. (December 22, 2005). "Inhaled Nitric Oxide Therapy in Adults". N Engl J Med. 353 (25): 2683–2695. doi:10.1056/NEJMra051884. PMID 16371634. S2CID 28911682.
- Abrams, J (1996). "Beneficial actions of nitrates in cardiovascular disease". The American Journal of Cardiology. 77 (13): 31C–7C. doi:10.1016/S0002-9149(96)00186-5. PMID 8638524.
- Moro, C; Leeds, C; Chess-Williams, R (January 2012). "Contractile activity of the bladder urothelium/lamina propria and its regulation by nitric oxide". Eur J Pharmacol. 674 (2–3): 445–449. doi:10.1016/j.ejphar.2011.11.020. PMID 22119378.
- Andersson, M.C; Tobin, G; Giglio, D (February 2008). "Cholinergic nitric oxide release from the urinary bladder mucosa in cyclophosphamide-induced cystitis of the anaesthetized rat". Br J Pharmacol. 153 (7): 1438–44. doi:10.1038/bjp.2008.6. PMC 2437908. PMID 18246091.
- Summerfield DT, Desai H, Levitov A, Grooms DA, Marik PE (2011). "Inhaled Nitric Oxide as Salvage Therapy in Massive Pulmonaryembolism: A Case Series". Respir Care. 57 (3): 444–8. doi:10.4187/respcare.01373. PMID 22005573.
- Katsnelson, Alla (2020-05-20). "Multiple clinical trials test whether NO gas can treat and prevent COVID-19". Chemical & Engineering News. Retrieved 2020-07-14.
- Cohan, Alexi (2020-07-26). "Nitric oxide, a 'miracle molecule,' could treat or even prevent coronavirus, top doctors say". Boston Herald. Retrieved 2020-07-27.
- Gander, Kashmira (2020-04-07). "What Is Nitric Oxide? How the Gas That Gave Us Viagra Could Help Treat Coronavirus Patients". Newsweek. Retrieved 2020-06-25.
- "Nitric Oxide Investigated as COVID-19 Treatment". WebMD. Retrieved 10 April 2020.
- Åkerström, Sara; Mousavi-Jazi, Mehrdad; Klingström, Jonas; Leijon, Mikael; Lundkvist, Åke; Mirazimi, Ali (1 February 2005). "Nitric Oxide Inhibits the Replication Cycle of Severe Acute Respiratory Syndrome Coronavirus". Journal of Virology. 79 (3): 1966–1969. doi:10.1128/JVI.79.3.1966-1969.2005. PMC 544093. PMID 15650225.
- Powell, Alvin (2020-05-06). "Applying wisdom from the Himalayas to the ER's COVID battle". The Harvard Gazette. Retrieved 2020-06-25.
- "Lessons from the Backcountry in Finding a Potential COVID-19 Treatment". Massachusetts General Hospital. 2020-06-24. Retrieved 2020-06-25.
- "Inhaled Nitric Oxide Therapy for Emergency Room COVID-19 Patients". Massachusetts General Hospital. 2020-06-24. Retrieved 2020-06-25.
- Meredith, Sam (2020-05-01). "How the gas that gave the world Viagra could help treat coronavirus patients". CNBC. Retrieved 2020-07-05.
- Riemer, Emily (2020-06-23). "Tufts researchers test inhaled nitric oxide as COVID-19 treatment". WCVB-TV. Retrieved 2020-07-05.
- Martel, Jan; Ko, Yun-Fei; Young, John D.; Ojcius, David (2020-05-06). "Could nasal nitric oxide help to mitigate the severity of COVID-19?". Microbes and Infection. doi:10.1016/j.micinf.2020.05.002. Retrieved 2020-05-06.
External links
- "Nitric oxide". Drug Information Portal. U.S. National Library of Medicine.