Human chorionic gonadotropin
Human chorionic gonadotropin (hCG) is a hormone produced by cells that are surrounding a growing embryo (syncitiotrophoblast initially) , which eventually forms the placenta after implantation.[1][2] The presence of hCG is detected in some pregnancy tests (HCG pregnancy strip tests). Some cancerous tumors produce this hormone; therefore, elevated levels measured when the patient is not pregnant may lead to a cancer diagnosis and, if high enough, paraneoplastic syndromes, however, it is not known whether this production is a contributing cause, or an effect of carcinogenesis. The pituitary analog of hCG, known as luteinizing hormone (LH), is produced in the pituitary gland of males and females of all ages.[1][3]
| Chorionic gonadotropin, alpha polypeptide | |
|---|---|
 | |
| Identifiers | |
| Symbol | CGA |
| Alt. symbols | FSHA, GPHa, GPHA1, HCG, LHA, TSHA |
| NCBI gene | 1081 |
| HGNC | 1885 |
| OMIM | 118850 |
| RefSeq | NM_000735 |
| UniProt | P01215 |
| Other data | |
| Locus | Chr. 6 q14-q21 |
| chorionic gonadotropin, beta polypeptide | |
|---|---|
| Identifiers | |
| Symbol | CGB |
| Alt. symbols | CGB3 |
| NCBI gene | 1082 |
| HGNC | 1886 |
| OMIM | 118860 |
| RefSeq | NM_000737 |
| UniProt | P01233 |
| Other data | |
| Locus | Chr. 19 q13.3 |
Regarding endogenous forms of hCG, there are various ways to categorize and measure them, including total hCG, C-terminal peptide total hCG, intact hCG, free β-subunit hCG, β-core fragment hCG, hyperglycosylated hCG, nicked hCG, alpha hCG, and pituitary hCG. Regarding pharmaceutical preparations of hCG from animal or synthetic sources, there are many gonadotropin preparations, some of which are medically justified and others of which are of a quack nature. As of December 6, 2011, the United States Food and Drug Administration has prohibited the sale of "homeopathic" and over-the-counter hCG diet products and declared them fraudulent and illegal.[4][5][6]
B hcg is initially secreted by syncitiotrophoblast.
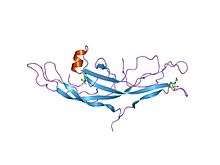
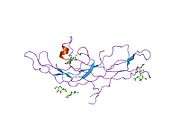
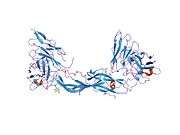
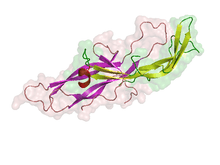
Structure
Human chorionic gonadotropin is a glycoprotein composed of 237 amino acids with a molecular mass of 36.7 kDa, approximately 14.5 αhCG and 22.2kDa βhCG.[7]
It is heterodimeric, with an α (alpha) subunit identical to that of luteinizing hormone (LH), follicle-stimulating hormone (FSH), thyroid-stimulating hormone (TSH), and β (beta) subunit that is unique to hCG.
- The α (alpha) subunit is 92 amino acids long.[8]
- The β-subunit of hCG gonadotropin (beta-hCG) contains 145 amino acids, encoded by six highly homologous genes that are arranged in tandem and inverted pairs on chromosome 19q13.3 - CGB (1, 2, 3, 5, 7, 8). It is known that CGB7 has a sequence slightly different from that of the others.[9]
The two subunits create a small hydrophobic core surrounded by a high surface area-to-volume ratio: 2.8 times that of a sphere. The vast majority of the outer amino acids are hydrophilic.[10]
beta-hCG is mostly similar to beta-LH, with the exception of a Carboxy Terminus Peptide (beta-CTP) containing four glycosylated serine residues that is responsible for hCG's longer half-life.[11]
Function
Human chorionic gonadotropin interacts with the LHCG receptor of the ovary and promotes the maintenance of the corpus luteum during the beginning of pregnancy. This allows the corpus luteum to secrete the hormone progesterone during the first trimester. Progesterone enriches the uterus with a thick lining of blood vessels and capillaries so that it can sustain the growing fetus.
Due to its highly negative charge, hCG may repel the immune cells of the mother, protecting the fetus during the first trimester. It has also been hypothesized that hCG may be a placental link for the development of local maternal immunotolerance. For example, hCG-treated endometrial cells induce an increase in T cell apoptosis (dissolution of T cells). These results suggest that hCG may be a link in the development of peritrophoblastic immune tolerance, and may facilitate the trophoblast invasion, which is known to expedite fetal development in the endometrium.[12] It has also been suggested that hCG levels are linked to the severity of morning sickness or Hyperemesis gravidarum in pregnant women.[13]
Because of its similarity to LH, hCG can also be used clinically to induce ovulation in the ovaries as well as testosterone production in the testes. As the most abundant biological source in women who are presently pregnant, some organizations collect urine from pregnant women to extract hCG for use in fertility treatment.
Human chorionic gonadotropin also plays a role in cellular differentiation/proliferation and may activate apoptosis.
Production
Naturally, it is produced in the human placenta by the syncytiotrophoblast.
Like any other gonadotropins, it can be extracted from the urine of pregnant women or produced from cultures of genetically modified cells using recombinant DNA technology.
In Pubergen, Pregnyl, Follutein, Profasi, Choragon and Novarel, it is extracted from the urine of pregnant women. In Ovidrel, it is produced with recombinant DNA technology.[14]
hCG forms
Regarding endogenous forms of hCG, there are various ways to categorize and measure them, including total hCG, C-terminal peptide total hCG, intact hCG, free β-subunit hCG, β-core fragment hCG, hyperglycosylated hCG, nicked hCG, alpha hCG, and pituitary hCG.
Regular hCG is the main form of hCG associated with the majority of pregnancy and in non-invasive molar pregnancies. This is produced in the trophoblast cells of the placental tissue. Hyperglycosylated hCG is the main form of hCG during the implantation phase of pregnancy, with invasive molar pregnancies, and with choriocarcinoma.
Regarding pharmaceutical preparations of hCG from animal or synthetic sources, there are many gonadotropin preparations, some of which are medically justified and others of which are of a quack nature.
Testing
Blood or urine tests measure hCG. These can be pregnancy tests. hCG-positive indicates an implanted blastocyst and mammalian embryogenesis. These can be done to diagnose and monitor germ cell tumors and gestational trophoblastic diseases.
Concentrations are commonly reported in thousandth international units per milliliter (mIU/ml). The international unit of hCG was originally established in 1938 and has been redefined in 1964 and in 1980.[15] At the present time, 1 international unit is equal to approximately 2.35×10−12 moles,[16] or about 6×10−8 grams.[17]
Methodology
Most tests employ a monoclonal antibody, which is specific to the β-subunit of hCG (β-hCG). This procedure is employed to ensure that tests do not make false positives by confusing hCG with LH and FSH. (The latter two are always present at varying levels in the body, whereas the presence of hCG almost always indicates pregnancy.)
Many hCG immunoassays are based on the sandwich principle, which uses antibodies to hCG labeled with an enzyme or a conventional or luminescent dye. Pregnancy urine dipstick tests are based on the lateral flow technique.
- The urine test may be a chromatographic immunoassay or any of several other test formats, home-, physician's office-, or laboratory-based.[18] Published detection thresholds range from 20 to 100 mIU/ml, depending on the brand of test.[19] Early in pregnancy, more accurate results may be obtained by using the first urine of the morning (when urine is most concentrated). When the urine is dilute (specific gravity less than 1.015), the hCG concentration may not be representative of the blood concentration, and the test may be falsely negative.
- The serum test, using 2-4 mL of venous blood, is typically a chemiluminescent or fluorimetric immunoassay[18] that can detect βhCG levels as low as 5 mIU/ml and allows quantification of the βhCG concentration.
Reference levels in normal pregnancy
The following is a list of serum hCG levels. (LMP is the last menstrual period dated from the first day of the last menstrual period.) The levels grow exponentially after conception and implantation.[20]
| weeks since LMP | mIU/mL |
|---|---|
| 3 | 5 – 50 |
| 4 | 5 – 428 |
| 5 | 18 – 7,340 |
| 6 | 1,080 – 56,500 |
| 7 – 8 | 7,650 – 229,000 |
| 9 – 12 | 25,700 – 288,000 |
| 13 – 16 | 13,300 – 254,000 |
| 17 – 24 | 4,060 – 165,400 |
| 25 – 40 | 3,640 – 117,000 |
| Non-pregnant females | <5.0 |
| Postmenopausal females | <9.5 |
Interpretation
The ability to quantitate the βhCG level is useful in the monitoring germ cell and trophoblastic tumors, follow-up care after miscarriage, and diagnosis of and follow-up care after treatment of ectopic pregnancy. The lack of a visible fetus on vaginal ultrasound after the βhCG levels have reached 1500 mIU/ml is strongly indicative of an ectopic pregnancy.[21] Still, even an hCG over 2000 IU/l does not necessarily exclude the presence of a viable intrauterine pregnancy in such cases.[22]
As pregnancy tests, quantitative blood tests and the most sensitive urine tests usually detect hCG between 6 and 12 days after ovulation.[23] It must be taken into account, however, that total hCG levels may vary in a very wide range within the first 4 weeks of gestation, leading to false results during this period.[24] A rise of 35% over 48 hours is proposed as the minimal rise consistent with a viable intrauterine pregnancy.[22]
Gestational trophoblastic disease like hydatidiform moles ("molar pregnancy") or choriocarcinoma may produce high levels of βhCG (due to the presence of syncytiotrophoblasts - part of the villi that make up the placenta) despite the absence of an embryo. This, as well as several other conditions, can lead to elevated hCG readings in the absence of pregnancy.
hCG levels are also a component of the triple test, a screening test for certain fetal chromosomal abnormalities/birth defects.
A study of 32 normal pregnancies came to the result a gestational sac of 1–3 mm was detected at a mean hCG level of 1150 IU/l (range 800-1500), a yolk sac was detected at a mean level of 6000 IU/l (range 4500-7500) and fetal heartbeat was visible at a mean hCG level of 10,000 IU/l (range 8650–12,200).[25]
Uses
Tumor marker
Human chorionic gonadotropin can be used as a tumor marker,[26] as its β subunit is secreted by some cancers including seminoma, choriocarcinoma, germ cell tumors, hydatidiform mole, teratoma with elements of choriocarcinoma, and islet cell tumor. For this reason, a positive result in males can be a test for testicular cancer. The normal range for men is between 0-5 mIU/mL. Combined with alpha-fetoprotein, β-HCG is an excellent tumor marker for the monitoring of germ cell tumors.
Fertility
| Clinical data | |
|---|---|
| Trade names | Novarel, Pregnyl |
| AHFS/Drugs.com | Monograph |
| ATC code | |
| Identifiers | |
| CAS Number | |
| DrugBank | |
| ChemSpider |
|
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.029.679 |
| Chemical and physical data | |
| Formula | C1105H1770N318O336S26 |
| Molar mass | 25719.70 g·mol−1 |
| | |
Human chorionic gonadotropin injection is extensively used for final maturation induction in lieu of luteinizing hormone. In the presence of one or more mature ovarian follicles, ovulation can be triggered by the administration of HCG. As ovulation will happen between 38 and 40 hours after a single HCG injection,[27] procedures can be scheduled to take advantage of this time sequence,[28] such as intrauterine insemination or sexual intercourse. Also, patients that undergo IVF, in general, receive HCG to trigger the ovulation process, but have an oocyte retrieval performed at about 34 to 36 hours after injection by, a few hours before the eggs actually would be released from the ovary.
As HCG supports the corpus luteum, administration of HCG is used in certain circumstances to enhance the production of progesterone.
In the male, HCG injections are used to stimulate the Leydig cells to synthesize testosterone. The intratesticular testosterone is necessary for spermatogenesis from the sertoli cells. Typical uses for HCG in men include hypogonadism and fertility treatment, including during testosterone replacement therapy to restore or maintain fertility and prevent testicular atrophy.
Several vaccines against human chorionic gonadotropin (hCG) for the prevention of pregnancy are currently in clinical trials.[29]
HCG Pubergen, Pregnyl warnings
In the case of female patients who want to be treated with HCG Pubergen, Pregnyl:[30] a) Since infertile female patients who undergo medically assisted reproduction (especially those who need in vitro fertilization), are known to often be suffering from tubal abnormalities, after a treatment with this drug they might experience many more ectopic pregnancies. This is why early ultrasound confirmation at the beginning of a pregnancy (to see whether the pregnancy is intrauterine or not) is crucial. Pregnancies that have occurred after a treatment with this medicine are submitted to a higher risk of multiplets. Female patients who have thrombosis, severe obesity, or thrombophilia should not be prescribed this medicine as they have a higher risk of arterial or venous thromboembolic events after or during a treatment with HCG Pubergen, Pregnyl. b)Female patients who have been treated with this medicine are usually more prone to pregnancy losses.
In the case of male patients: A prolonged treatment with HCG Pubergen, Pregnyl is known to regularly lead to increased production of androgen. Therefore: Patients who are suffering from overt or latent cardiac failure, hypertension, renal dysfunction, migraines, or epilepsy might not be allowed to start using this medicine or may require a lower dose of HCG Pubergen, Pregnyl. Also this medicine should be used with extreme caution in the treatment of prepubescent teenagers in order to reduce the risk of precocious sexual development or premature epiphyseal closure. This type of patients' skeletal maturation should be closely and regularly monitored.
Both male and female patients who have the following medical conditions must not start a treatment with HCG Pubergen, Pregnyl: (1) Hypersensitivity to this medicine or to any of its main ingredients. (2) Known or possible androgen-dependent tumors for example male breast carcinoma or prostatic carcinoma.
Anabolic steroid adjunct
In the world of performance-enhancing drugs, HCG is increasingly used in combination with various anabolic-androgenic steroid (AAS) cycles. [31] As a result, HCG is included in some sports' illegal drug lists.
When exogenous AAS are put into the male body, natural negative-feedback loops cause the body to shut down its own production of testosterone via shutdown of the hypothalamic-pituitary-gonadal axis (HPGA). This causes testicular atrophy, among other things. HCG is commonly used during and after steroid cycles to maintain and restore testicular size as well as normal testosterone production.[32]
High levels of AASs, that mimic the body's natural testosterone, trigger the hypothalamus to shut down its production of gonadotropin-releasing hormone (GnRH) from the hypothalamus. Without GnRH, the pituitary gland stops releasing luteinizing hormone (LH). LH normally travels from the pituitary via the blood stream to the testes, where it triggers the production and release of testosterone. Without LH, the testes shut down their production of testosterone.[33] In males, HCG helps restore and maintain testosterone production in the testes by mimicking LH and triggering the production and release of testosterone.
If HCG is used for too long and in too high a dose, the resulting rise in natural testosterone and estrogen would eventually inhibit endogenous production of luteinizing hormone via negative feedback on the hypothalamus and pituitary gland.
Professional athletes who have tested positive for HCG have been temporarily banned from their sport, including a 50-game ban from MLB for Manny Ramirez in 2009[34] and a 4-game ban from the NFL for Brian Cushing for a positive urine test for HCG.[35] Mixed Martial Arts fighter Dennis Siver was fined $19,800 and suspended 9 months for being tested positive after his bout at UFC 168.[36]
HCG diet
British endocrinologist Albert T. W. Simeons proposed HCG as an adjunct to an ultra-low-calorie weight-loss diet (fewer than 500 calories).[37] Simeons, while studying pregnant women in India on a calorie-deficient diet, and "fat boys" with pituitary problems (Frölich's syndrome) treated with low-dose HCG, observed that both lost fat rather than lean (muscle) tissue.[37] He reasoned that HCG must be programming the hypothalamus to do this in the former cases in order to protect the developing fetus by promoting mobilization and consumption of abnormal, excessive adipose deposits. Simeons in 1954 published a book entitled Pounds and Inches, designed to combat obesity. Simeons, practicing at Salvator Mundi International Hospital in Rome, Italy, recommended low-dose daily HCG injections (125 IU) in combination with a customized ultra-low-calorie (500 cal/day, high-protein, low-carbohydrate/fat) diet, which was supposed to result in a loss of adipose tissue without loss of lean tissue.[37]
Other researchers did not find the same results when attempting experiments to confirm Simeons' conclusions, and in 1976 in response to complaints the FDA required Simeons and others to include the following disclaimer on all advertisements:[38]
These weight reduction treatments include the injection of HCG, a drug which has not been approved by the Food and Drug Administration as safe and effective in the treatment of obesity or weight control. There is no substantial evidence that HCG increases weight loss beyond that resulting from caloric restriction, that it causes a more attractive or "normal" distribution of fat, or that it decreases the hunger and discomfort associated with calorie-restrictive diets.
— 1976 FDA-mandated disclaimer for HCG diet advertisements
There was a resurgence of interest in the "HCG diet" following promotion by Kevin Trudeau, who was banned from making HCG diet weight-loss claims by the U.S. Federal Trade Commission in 2008, and eventually jailed over such claims.[39]
A 1976 study in the American Journal of Clinical Nutrition[40] concluded that HCG is not more effective as a weight-loss aid than dietary restriction alone.[41]
A 1995 meta analysis found that studies supporting HCG for weight loss were of poor methodological quality and concluded that "there is no scientific evidence that HCG is effective in the treatment of obesity; it does not bring about weight-loss or fat-redistribution, nor does it reduce hunger or induce a feeling of well-being".[42]
On November 15, 2016, the American Medical Association (AMA) passed policy that "The use of human chorionic gonadotropin (HCG) for weight loss is inappropriate."[43]
There is no scientific evidence that HCG is effective in the treatment of obesity. The meta-analysis found insufficient evidence supporting the claims that HCG is effective in altering fat-distribution, hunger reduction, or in inducing a feeling of well-being. The authors stated “…the use of HCG should be regarded as an inappropriate therapy for weight reduction…” In the authors opinion, “Pharmacists and physicians should be alert on the use of HCG for Simeons therapy. The results of this meta-analysis support a firm standpoint against this improper indication. Restraints on physicians practicing this therapy can be based on our findings.”
According to the American Society of Bariatric Physicians, no new clinical trials have been published since the definitive 1995 meta-analysis.[44]
The scientific consensus is that any weight loss reported by individuals on an "HCG diet" may be attributed entirely to the fact that such diets prescribe calorie intake of between 500 and 1,000 calories per day, substantially below recommended levels for an adult, to the point that this may risk health effects associated with malnutrition.[45]
Homeopathic HCG for weight control
Controversy about, and shortages[46] of, injected HCG for weight loss have led to substantial Internet promotion of "homeopathic HCG" for weight control. The ingredients in these products are often obscure, but if prepared from true HCG via homeopathic dilution, they contain either no HCG at all or only trace amounts. Moreover, it is highly unlikely that oral HCG is bioavailable due to the fact that digestive protease enzymes and hepatic metabolism renders peptide-based molecules (such as insulin and human growth hormone) biologically inert. HCG can likely only enter the bloodstream through injection.
The United States Food and Drug Administration has stated that over-the-counter products containing HCG are fraudulent and ineffective for weight loss. They are also not protected as homeopathic drugs and have been deemed illegal substances.[47] HCG is classified as a prescription drug in the United States and it has not been approved for over-the-counter sales by the FDA as a weight loss product or for any other purposes, and therefore neither HCG in its pure form nor any preparations containing HCG may be sold legally in the country except by prescription.[4] In December 2011, FDA and FTC started to take actions to pull unapproved HCG products from the market.[4] In the aftermath, some suppliers started to switch to "hormone-free" versions of their weight loss products, where the hormone is replaced with an unproven mixture of free amino acids[48] or where radionics is used to transfer the "energy" to the final product.
Tetanus vaccine conspiracy theory
Catholic Bishops in Kenya[49] are among those who have spread a conspiracy theory[50] asserting that HCG forms part of a covert sterilization program, forcing denials from the Kenyan government.[49]
In order to induce a stronger immune response, some versions of human chorionic gonadotropin-based anti-fertility vaccines were designed as conjugates of the β subunit of HCG covalently linked to tetanus toxoid.[29][51] It has been alleged that a non-conjugated tetanus vaccine used in developing countries is laced with a human chorionic gonadotropin based anti-fertility drug and is distributed as a means of mass sterilization.[52] This charge has been vigorously denied by the World Health Organization (WHO) and UNICEF.[53] Others have argued that a hCG laced vaccine could not be used for sterilization since the effects of the anti-fertility vaccines are reversible (requiring booster doses to maintain immunity) and a non-conjugated vaccine is likely to be ineffective.[54] Finally, independent testing of the tetanus vaccine by Kenya's health authorities has revealed no traces of the human chorionic gonadotropin hormone.[55]
See also
- Equine chorionic gonadotropin
- Gonadotropin preparations
- Human placental lactogen
- Triple test - a screening test in pregnancy
- The Weight-Loss Cure "They" Don't Want You to Know About - Kevin Trudeau's book
References
- Cole LA (2009). "New discoveries on the biology and detection of human chorionic gonadotropin". Reprod. Biol. Endocrinol. 7: 8. doi:10.1186/1477-7827-7-8. PMC 2649930. PMID 19171054.
- Gregory JJ, Finlay JL (April 1999). "Alpha-fetoprotein and beta-human chorionic gonadotropin: their clinical significance as tumour markers". Drugs. 57 (4): 463–7. doi:10.2165/00003495-199957040-00001. PMID 10235686.
- Hoermann R, Spoettl G, Moncayo R, Mann K (July 1990). "Evidence for the presence of human chorionic gonadotropin (hCG) and free beta-subunit of hCG in the human pituitary". J. Clin. Endocrinol. Metab. 71 (1): 179–86. doi:10.1210/jcem-71-1-179. PMID 1695224.
- Gever J (December 6, 2011). "FDA Yanks HCG Weight Loss Agents from Market". MedPage Today. Retrieved December 7, 2011.
- "HCG Diet Products Are Illegal". FDA. December 6, 2011.
- "FDA, FTC act to remove 'homeopathic' HCG weight loss products from the market" (Press release). FDA. December 6, 2011. Retrieved December 7, 2011.
- Canfield RE, O'Connor JF, Birken S, Krichevsky A, Wilcox AJ (October 1987). "Development of an assay for a biomarker of pregnancy and early fetal loss". Environmental Health Perspectives. 74: 57–66. doi:10.1289/ehp.877457. PMC 1474496. PMID 3319556.
- "Glycoprotein hormones alpha chain precursor - Homo sapiens (Human)". UniProt accession number P01215. UniProt Consortium.
P01215[25-116]
- "Choriogonadotropin subunit beta 3 - Homo sapiens (Human)". UniProt accession number P01233. UniProt Consortium.
P0DN86[21-165]; Two specific hCGb proteins that differ by three amino acids in positions 2,4 and 117 have been described: type 1 (CGB7) and type 2 (CGB3, CGB5, CGB8).
- PDB: 1HRP; Lapthorn AJ, Harris DC, Littlejohn A, Lustbader JW, Canfield RE, Machin KJ, Morgan FJ, Isaacs NW (June 1994). "Crystal structure of human chorionic gonadotropin". Nature. 369 (6480): 455–61. Bibcode:1994Natur.369..455L. doi:10.1038/369455a0. PMID 8202136.
- Furuhashi M, Shikone T, Fares FA, Sugahara T, Hsueh AJ, Boime I (January 1995). "Fusing the carboxy-terminal peptide of the chorionic gonadotropin (CG) beta-subunit to the common alpha-subunit: retention of O-linked glycosylation and enhanced in vivo bioactivity of chimeric human CG". Molecular Endocrinology. 9 (1): 54–63. doi:10.1210/mend.9.1.7539107. PMID 7539107.
- Kayisli U, Selam B, Guzeloglu-Kayisli O, Demir R, Arici A (2003). "Human chorionic gonadotropin contributes to maternal immunotolerance and endometrial apoptosis by regulating Fas-Fas ligand system". J. Immunol. 171 (5): 2305–13. doi:10.4049/jimmunol.171.5.2305. PMID 12928375.
- Askling J, Erlandsson G, Kaijser M, Akre O, Ekbom A (December 1999). "Sickness in pregnancy and sex of child". Lancet. 354 (9195): 2053. doi:10.1016/S0140-6736(99)04239-7. PMID 10636378.
- The Practice Committee of the American Society for Reproductive Medicine, Birmingham, Alabama (November 2008). "Gonadotropin preparations: past, present, and future perspectives". Fertility and Sterility. 90 (5 Suppl): S13–20. doi:10.1016/j.fertnstert.2008.08.031. PMID 19007609.
- "The Diagnosis of Pregnancy".
- "WHO Reference Reagent Human Chorionic Gonadotrophin (Purified) NIBSC code: 99/688 Instructions for use (Version 3.0, Dated 05/11/2007)" (PDF). Archived from the original (PDF) on 2012-12-03.
- Canfield RE, Ross GT (1976). "A new reference preparation of human chorionic gonadotrophin and its subunits". Bulletin of the World Health Organization. 54 (4): 463–472. PMC 2366462. PMID 1088359.
- McPherson RA, Pincus MR (2006). Henry's Clinical Diagnosis and Management by Laboratory Methods (21st ed.). Philadelphia: Saunders. ISBN 978-1-4160-0287-1.
- Waddell RS (2006). "FertilityPlus.org". Home Pregnancy Test hCG Levels and FAQ. Archived from the original on 2006-06-15. Retrieved 2006-06-17.
- "Guideline To HCG Levels During Pregnancy". American Pregnancy Association. 22 August 2017.
- Tualndi T. "Dr". UpToDate. Retrieved 1 June 2013.
- Kirk E, Bottomley C, Bourne T (2013). "Diagnosing ectopic pregnancy and current concepts in the management of pregnancy of unknown location". Human Reproduction Update. 20 (2): 250–61. doi:10.1093/humupd/dmt047. PMID 24101604.
- Wilcox AJ, Baird DD, Weinberg CR (1999). "Time of implantation of the conceptus and loss of pregnancy". New England Journal of Medicine. 340 (23): 1796–1799. doi:10.1056/NEJM199906103402304. PMID 10362823.
- Butler SA, Khanlian SA, Cole LA (2001). "Detection of early pregnancy forms of human chorionic gonadotropin by home pregnancy test devices". Clinical Chemistry. 47 (12): 2131–2136. doi:10.1093/clinchem/47.12.2131. PMID 11719477.
- Giacomello F, Magliocchetti P, Loyola G, Giovarruscio M (1993). "[Serum beta hCG levels and transvaginal echography in the early phases of pregnancy]". Minerva Ginecol (in Italian). 45 (7–8): 333–7. PMID 8414139.
- "Tumor Markers Found in Blood or Urine". American Cancer Society. Retrieved 21 January 2014.
- HCG Injection After Ovulation Induction With Clomiphene Citrate at Medscape. By Peter Kovacs. Posted: 04/23/2004
- IVF.com Archived 2012-02-26 at the Wayback Machine; Ovulation Induction. Retrieved Mars 7, 2010
- Talwar GP, Gupta JC, Rulli SB, Sharma RS, Nand KN, Bandivdekar AH, Atrey N, Singh P (2015). "Advances in development of a contraceptive vaccine against human chorionic gonadotropin". Expert Opinion on Biological Therapy. 15 (8): 1183–90. doi:10.1517/14712598.2015.1049943. PMID 26160491.
- "HCG Pregnyl". 2010-10-13. Archived from the original on 2011-03-25. Retrieved 2010-10-23.
- "Anabolic Steroids and SARMS Handbook for Bodybuilders and Athletes". Retrieved 2019-06-16.
- Williams L (May 8, 2009). "Manny Ramirez suspended; testosterone ratio exceeded limits; fertility drug reported". San Francisco Chronicle.
- van Breda E, Keizer HA, Kuipers H, Wolffenbuttel BH (April 2003). "Androgenic anabolic steroid use and severe hypothalamic-pituitary dysfunction: a case study". Int J Sports Med. 24 (3): 195–6. doi:10.1055/s-2003-39089. PMID 12740738.
- Schmidt MS (May 8, 2009). "Manny Ramirez Is Banned for 50 Games". The New York Times.
- McClain J (2010-05-12). "Cushing suspended for performance-enhancing drugs". Houston Texans Football. Houston Chronicle. Retrieved 2010-10-23.
- Holland JS (April 24, 2014). "Dennis Siver fined, suspended nine months for positive drug test following UFC 168". MMAMania.com.
- Simeons AT (2010). Pounds & Inches: A New Approach To Obesity. Popular Publishing. ISBN 978-0-615-42755-3.
- In the Matter of Simeon Management Corp. (Fed. Trade Comm'n, 1976) 87 F.T.C. 1184; affirmed by Simeon Management Corp. v. FTC (9th Cir. 1978) 579 F.2d 1137, 49 ALR-Fed 1.
- Kevin Trudeau Banned from Infomercials For Three Years, Ordered to Pay More Than $5 Million for False Claims About Weight-Loss Book; FTC v. Trudeau (7th Cir., 2009) 579 F.3d 754 remanded (N.D.Ill., 2010) 708 F.Supp.2d 711, affirmed (7th Cir. 2011) 662 F.3d 947, certiorari denied (Oct. 9, 2012) _U.S._, 133 S.Ct. 426, 184 L.Ed.2d 257; and a ten-year prison sentence for violating a court order, U.S. v. Trudeau (N.D.Ill., Jan. 29, 2014) 2014 u.s.dist. LEXIS 10717, 2014 WL 321373. And the article, The Curious Case of Kevin Trudeau, King Catch Me If You Can by Catherine Bryant Bell, Mississippi Law Journal, vol. 79 page 1043 (summer 2010), http://heinonline.org/HOL/Page?handle=hein.journals/mislj79&div=44&g_sent=1&collection=journals#1053.
- Stein MR, Julis RE, Peck CC, Hinshaw W, Sawicki JE, Deller JJ (September 1976). "Ineffectiveness of human chorionic gonadotropin in weight reduction: a small double-blind study". Am. J. Clin. Nutr. 29 (9): 940–8. doi:10.1093/ajcn/29.9.940. PMID 786001.
- Barrett S. "HCG Worthless as Weight-Loss Aid". Diet Scam Watch. dietscam.org. Retrieved 2009-02-03.
- Lijesen GK, Theeuwen I, Assendelft WJ, Van Der Wal G (September 1995). "The effect of human chorionic gonadotropin (HCG) in the treatment of obesity by means of the Simeons therapy: a criteria-based meta-analysis". Br J Clin Pharmacol. 40 (3): 237–43. doi:10.1111/j.1365-2125.1995.tb05779.x. PMC 1365103. PMID 8527285.
- Association, Obesity Medicine. "Obesity Medicine Association Applauds American Medical Association's Decision to Adopt New Anti-HCG Policy". GlobeNewswire News Room. Retrieved 2016-11-16.
- American Society of Bariatric Physicians Archived 2012-05-11 at the Wayback Machine, position statement on HCG diet
- Does the HCG diet work — and is it safe?, Mayo Clinic
- "Chorionic Gonadotropin (Human) Injection Shortage". Bulletin. American Society of Health-System Pharmacists. 2010-10-13. Retrieved 2010-10-23.
- Hellmich N (2011-01-23). "HCG weight-loss products are fraudulent, FDA says - USATODAY.com". USA Today. Retrieved 2011-02-03.
- "Hormone-Free HCG Drops are Quickly Replacing Homeopathic Counterparts". San Francisco Chronicle. March 9, 2012.
- Ohlheiser, Abby. "The tense standoff between Catholic bishops and the Kenyan government over tetanus vaccines". Washington Post. Retrieved 2020-06-04.
- "Is Tetanus Vaccine Spiked with Sterilization Chemicals?". Snopes.com. Retrieved 2020-06-04.
- Talwar GP (1997). "Fertility regulating and immunotherapeutic vaccines reaching human trials stage" (PDF). Human Reproduction Update. 3 (4): 301–10. doi:10.1093/humupd/3.4.301. PMID 9459276.
- "Tetanus vaccine may be laced with anti-fertility drug. International / developing countries". Vaccine Weekly: 9–10. 1995. PMID 12346214.
- Griffin B (9 March 2015). "WHO, UNICEF deny Kenyan bishops' claim that they supplied sterility-causing tetanus vaccines". National Catholic Reporter.
- Gorski D (15 November 2014). "Fear mongering about vaccines as "racist population control" in Kenya". Science-Based Medicine.
- Shiundu A (5 November 2014). "Health officials want to punish doctor in tetanus vaccine dispute". Standard Digital.
External links
- Chorionic+Gonadotropin at the US National Library of Medicine Medical Subject Headings (MeSH)
- History of pregnancy test (NIH)