Nosebleed
A nosebleed, also known as epistaxis, is bleeding from the nose.[1] Blood can also flow down into the stomach and cause nausea and vomiting.[8] In more severe cases blood may come out of both nostrils.[9] Rarely bleeding may be so significant low blood pressure occurs.[1] Rarely the blood can come up the nasolacrimal duct and out from the eye.[10]
| Nosebleed | |
|---|---|
| Other names | Epistaxis, bloody nose, nasal hemorrhage[1] |
 | |
| A three-year-old child with a minor nosebleed from falling and hitting his face on the floor. | |
| Pronunciation |
|
| Specialty | Otorhinolaryngology |
| Symptoms | Bleeding from the nose[1] |
| Usual onset | Less than 10 and over 50 years old[2] |
| Risk factors | Trauma, Excessive Nose-picking, blood thinners, high blood pressure, alcoholism, seasonal allergies, dry weather[3] |
| Diagnostic method | Direct observation[1] |
| Differential diagnosis | Bleeding from the lungs, esophageal varices[1] |
| Prevention | Petroleum jelly in the nose[4] |
| Treatment | Pressure over the lower half of the nose, nasal packing, endoscopy[5] |
| Medication | Tranexamic acid[6] |
| Frequency | 60% at some point in time[7] |
| Deaths | Rare[3] |
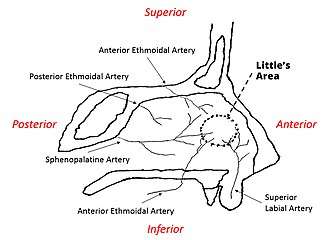
Risk factors include trauma including putting the finger in the nose, blood thinners, high blood pressure, alcoholism, seasonal allergies, dry weather, and inhaled corticosteroids.[3] There are two types: anterior, which is more common; and posterior, which is less common but more serious.[3] Anterior nosebleeds generally occur from Kiesselbach's plexus while posterior bleeds generally occur from the sphenopalatine artery.[3] The diagnosis is by direct observation.[1]
Prevention may include the use of petroleum jelly in the nose.[4] Initially treatment is generally by applying pressure for at least five minutes over the lower half of the nose.[5] If this is not sufficient nasal packing may be used.[5] Tranexamic acid may also be helpful.[6] If bleeding episodes continue endoscopy is recommended.[5]
About 60% of people have a nosebleed at some point in their life.[7] About 10% of nosebleeds are serious.[7] Nosebleeds are rarely fatal, accounting for only 4 of the 2.4 million deaths in the U.S. in 1999.[11] Nosebleeds most commonly affect those younger than 10 and older than 50.[2]
Cause

Nosebleeds can occur due to a variety of reasons. Some of the most common causes include trauma from nose picking, blunt trauma (such as a motor vehicle accident), or insertion of a foreign object (more likely in children).[4] Relative humidity (including centrally heated buildings), respiratory tract infections, chronic sinusitis, rhinitis or environmental irritants can cause inflammation and thinning of the tissue in the nose, leading to a greater likelihood of bleeding from the nose.[4]
Most causes of nose bleeding are self-limiting and do not require medical attention. However, if nosebleeds are recurrent or do not respond to home therapies, an underlying cause may need to be investigated. Some rarer causes are listed below:[2][4][12]
Coagulopathy
- Thrombocytopenia (thrombotic thrombocytopenic purpura, idiopathic thrombocytopenic purpura)
- Von Willebrand's disease
- Hemophilia
- Leukemia
- HIV
- Chronic liver disease—cirrhosis causes deficiency of factor II, VII, IX,& X
Dietary
- Sulfur dioxide (sulphur dioxide) E220 (as a food preservative used particularly in wines, dried fruits, etc. )
- Sulphites as food preservatives
- Salicylates naturally occurring in some fruits and vegetables
Inflammatory
- Granulomatosis with polyangiitis
- Systemic lupus erythematosus
Medications/Drugs
- Anticoagulation (warfarin, heparin, aspirin, etc)
- Insufflated drugs (particularly cocaine)
- Nasal sprays (particularly prolonged or improper use of nasal steroids)
Neoplastic
- Squamous cell carcinoma
- Adenoid Cystic Carcinoma
- Melanoma
- Nasopharyngeal carcinoma
- Nasopharyngeal angiofibroma
Traumatic
- Anatomical deformities (e.g. septal spurs)
- Blunt trauma (usually a sharp blow to the face such as a punch, sometimes accompanying a nasal fracture)
- Foreign bodies (such as fingers during nose-picking)
- Digital trauma
- Middle ear barotrauma (such as from descent in aircraft or ascent in scuba diving)
- Nasal bone fracture
- Septal fracture/perforation
- Surgery (e.g. septoplasty and functional endoscopic sinus surgery)
- Nasal bleeds may be due to fracture of facial bones namely maxilla and zygoma.
Vascular
- Hereditary hemorrhagic telangiectasia (Osler–Weber–Rendu disease)
- Angioma
- Aneurysm of the carotid artery
Pathophysiology
The nasal mucosa contains a rich blood supply that can be easily ruptured and cause bleeding. Rupture may be spontaneous or initiated by trauma. Nosebleeds are reported in up to 60% of the population with peak incidences in those under the age of ten and over the age of 50 and appear to occur in males more than females.[13] An increase in blood pressure (e.g. due to general hypertension) tends to increase the duration of spontaneous epistaxis.[14] Anticoagulant medication and disorders of blood clotting can promote and prolong bleeding. Spontaneous epistaxis is more common in the elderly as the nasal mucosa (lining) becomes dry and thin and blood pressure tends to be higher. The elderly are also more prone to prolonged nosebleeds as their blood vessels are less able to constrict and control the bleeding.
The vast majority of nosebleeds occur in the anterior (front) part of the nose from the nasal septum. This area is richly endowed with blood vessels (Kiesselbach's plexus). This region is also known as Little's area. Bleeding farther back in the nose is known as a posterior bleed and is usually due to bleeding from Woodruff's plexus, a venous plexus situated in the posterior part of inferior meatus.[15] Posterior bleeds are often prolonged and difficult to control. They can be associated with bleeding from both nostrils and with a greater flow of blood into the mouth.[13]
Sometimes blood flowing from other sources of bleeding passes through the nasal cavity and exits the nostrils. It is thus blood coming from the nose but is not a true nosebleed, that is, not truly originating from the nasal cavity. Such bleeding is called "pseudoepistaxis" (pseudo + epistaxis). Examples include blood coughed up through the airway and ending up in the nasal cavity, then dripping out.
Prevention
People with uncomplicated nosebleeds can use conservative methods to prevent future nosebleeds such as sleeping in a humidified environment or applying petroleum jelly to the nasal nares.[4]
Treatment
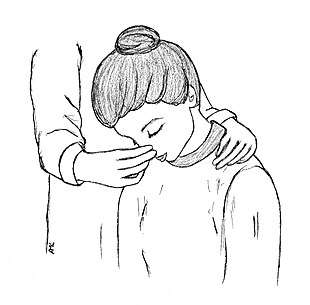
Most anterior nosebleeds can be stopped by applying direct pressure, which helps by promoting blood clots.[4] Those who suffer a nosebleed should first attempt to blow out any blood clots and then apply pressure for at least five minutes and up to 20 minutes.[4] Pressure should be firm and tilting the head forward helps decrease the chance of nausea and airway obstruction as seen in the picture on the right.[13] When attempting to stop a nosebleed at home, the head should not be tilted back.[2] Swallowing excess blood can irritate the stomach and cause vomiting. Vasoconstrictive medications such as oxymetazoline (Afrin) or phenylephrine are widely available over the counter for treatment of allergic rhinitis and may also be used to control benign cases of epistaxis.[16] Those with nosebleeds that last longer than 20 minutes (in the setting of direct pressure as seen in the image to the right) should seek medical attention.[4]
Nasal packing
If pressure and chemical cauterization cannot stop bleeding, nasal packing is the mainstay of treatment.[17] There are several forms of nasal packing that can be contrasted by anterior nasal packing and posterior nasal packing.[18] Traditionally, nasal packing was accomplished by packing gauze into the nose, thereby placing pressure on the vessels in the nose and stopping the bleeding. Traditional gauze packing has been replaced with products such as Merocel and the Rapid Rhino.[17] The Merocel nasal tampon is similar to gauze packing except it is a synthetic foam polymer (made of polyvinyl alcohol and expands in the nose after application of water) that provides a less hospitable medium for bacteria.[4] The Rapid Rhino stops nosebleeds using a balloon catheter, made of carboxymethylcellulose, which has a cuff that is inflated by air to stop bleeding through extra pressure in the nasal cavity.[17] Systematic review articles have demonstrated that the efficacy in stopping nosebleeds is similar between the Rapid Rhino and Merocel packs; however, the Rapid Rhino has been shown to have greater ease of insertion and reduced discomfort.[17] People who receive nasal packing need to return to a medical professional in 24–72 hours in order to have packing removed.[4][3] There are also several dissolvable packing materials that stop bleeding through use of thrombotic agents that promote blood clots, such as surgicel.[4] The thrombogenic foams and gels do not require removal and dissolve after a few days. Posterior nasal packing can be achieved by using a Foley catheter, blowing up the balloon when it is in the back of the throat, and applying traction.[18] Complications of nasal packing include abscesses, septal hematomas, sinusitis, and pressure necrosis.[2] In rare cases toxic shock syndrome can occur with prolonged nasal packing. As a result, many forms of nasal packing involve use of topical antistaphylococcal antibiotic ointment.[2]
Tranexamic acid
Tranexamic acid helps promote blood clotting.[6] For nosebleeds it can be applied to the site of bleeding, taken by mouth, or injected into a vein.[6]
Cauterization
This method involves applying a chemical such as silver nitrate to the nasal mucosa, which burns and seals off the bleeding.[12] Eventually the nasal tissue to which the chemical is applied will undergo necrosis.[12] This form of treatment is best for mild bleeds, especially in children, that are clearly visible.[12] A topical anesthetic (such as lidocaine) is usually applied prior to cauterization. Silver nitrate can cause blackening of the skin due to silver sulfide deposit, though this will fade with time.[19]
Surgery
Ongoing bleeding despite good nasal packing is a surgical emergency and can be treated by endoscopic evaluation of the nasal cavity under general anesthesia to identify an elusive bleeding point or to directly ligate (tie off) the blood vessels supplying the nose. These blood vessels include the sphenopalatine, anterior and posterior ethmoidal arteries. More rarely the maxillary or a branch of the external carotid artery can be ligated. The bleeding can also be stopped by intra-arterial embolization using a catheter placed in the groin and threaded up the aorta to the bleeding vessel by an interventional radiologist.[20] There is no difference in outcomes between embolization and ligation as treatment options, but embolization is considerably more expensive.[21] Continued bleeding may be an indication of more serious underlying conditions.[20]
Society and culture
In the visual language of Japanese manga and anime, a sudden, violent nosebleed indicates that the bleeding person is sexually aroused.[26][27] In Western fiction, nosebleeds often signify intense mental focus or effort, particularly during the use of psychic powers.[28][29]
In American and Canadian usage, "nosebleed section" or "nosebleed seats" are common slang for seating at sporting or other spectator events that are the highest up and farthest away from the event. The reference alludes to the propensity for nasal hemorrhage at high altitudes, usually owing to lower barometric pressure.
The oral history of the Native American Sioux tribe includes reference to women who experience nosebleeds as a result of a lover's playing of music, implying sexual arousal.[30]
In Finnish language, "picking blood from one's nose" and "begging for a nosebleed" are commonly used in abstract meaning to describe self-destructive behaviour, for example ignoring safety procedures or deliberately aggravating stronger parties.[31]
In Filipino slang, to "have a nosebleed" is to have serious difficulty conversing in English with a fluent or native English speaker. It can also refer to anxiety brought on by a stressful event such as an examination or a job interview.[32]
In the Dutch language, "pretending to have a nosebleed" is a saying that means pretending not to know anything about something.[33]
Etymology
The word epistaxis is from Greek: ἐπιστάζω epistazo, "to bleed from the nose" from ἐπί epi, "above, over" and στάζω stazo, "to drip [from the nostrils]".
References
- Ferri, Fred F. (2013). Ferri's Clinical Advisor 2014 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 399. ISBN 978-0-323-08431-4.
- Kucik, Corry J.; Clenney, Timothy (2005-01-15). "Management of epistaxis". American Family Physician. 71 (2): 305–311. ISSN 0002-838X. PMID 15686301.
- Tabassom, A; Cho, JJ (January 2020). "Epistaxis (Nose Bleed)". StatPearls. PMID 28613768.
- Morgan, Daniel J.; Kellerman, Rick (March 2014). "Epistaxis". Primary Care: Clinics in Office Practice. 41 (1): 63–73. doi:10.1016/j.pop.2013.10.007. ISSN 0095-4543. PMID 24439881.
- Tunkel, David E.; Anne, Samantha; Payne, Spencer C.; Ishman, Stacey L.; Rosenfeld, Richard M.; Abramson, Peter J.; Alikhaani, Jacqueline D.; Benoit, Margo McKenna; Bercovitz, Rachel S.; Brown, Michael D.; Chernobilsky, Boris; Feldstein, David A.; Hackell, Jesse M.; Holbrook, Eric H.; Holdsworth, Sarah M.; Lin, Kenneth W.; Lind, Meredith Merz; Poetker, David M.; Riley, Charles A.; Schneider, John S.; Seidman, Michael D.; Vadlamudi, Venu; Valdez, Tulio A.; Nnacheta, Lorraine C.; Monjur, Taskin M. (7 January 2020). "Clinical Practice Guideline: Nosebleed (Epistaxis) Executive Summary". Otolaryngology–Head and Neck Surgery. 162 (1): 8–25. doi:10.1177/0194599819889955. PMID 31910122.
- Joseph, Jonathan; Martinez-Devesa, Pablo; Bellorini, Jenny; Burton, Martin J (2018-12-31). Cochrane ENT Group (ed.). "Tranexamic acid for patients with nasal haemorrhage (epistaxis)". Cochrane Database of Systematic Reviews. 12: CD004328. doi:10.1002/14651858.CD004328.pub3. PMC 6517002. PMID 30596479.
- Wackym, James B. Snow,... P. Ashley (2009). Ballenger's otorhinolaryngology : head and neck surgery (17th ed.). Shelton, Conn.: People's Medical Pub. House/B C Decker. p. 551. ISBN 9781550093377.
- Wilson, I. Dodd (1990). Walker, H. Kenneth; Hall, W. Dallas; Hurst, J. Willis (eds.). Clinical Methods: The History, Physical, and Laboratory Examinations (3rd ed.). Boston: Butterworths. ISBN 978-0409900774. PMID 21250251.
- Krulewitz, NA; Fix, ML (February 2019). "Epistaxis". Emergency Medicine Clinics of North America. 37 (1): 29–39. doi:10.1016/j.emc.2018.09.005. PMID 30454778.
- Riordan-Eva, Paul (2000). Vaughan and Asbury's General Ophthalmology. McGraw Hill Professional. p. 92. ISBN 978-0-07-137831-4.
- "Work Table I. Deaths from each cause by 5-year age groups, race and sex: US, 1999" (PDF). CDC. 2011. p. 1922. Retrieved 13 April 2020.
- Svider, Peter; Arianpour, Khashayar; Mutchnick, Sean (June 2018). "Management of Epistaxis in Children and Adolescents". Pediatric Clinics of North America. 65 (3): 607–621. doi:10.1016/j.pcl.2018.02.007. ISSN 0031-3955. PMID 29803286.
- Corry J. Kucik; Timothy Clenney (January 15, 2005). "Management of Epistaxis". American Family Physician. American Academy of Family Physicians. 71 (2): 305–311. PMID 15686301. Retrieved January 31, 2010.
- J. F. Lubianca Neto; F. D. Fuchs; S. R. Facco; M. Gus; L. Fasolo; R. Mafessoni; A. L. Gleissner (1999). "Is epistaxis evidence of end-organ damage in patients with hypertension?". Laryngoscope. 109 (7): 1111–1115. doi:10.1097/00005537-199907000-00019. PMID 10401851.
- The Journal of Laryngology & Otology (2008), 122: 1074–1077
- Guarisco JL, Graham HD (1989). "Epistaxis in children: causes, diagnosis, and treatment". Ear Nose Throat J. 68 (7): 522, 528–30, 532 passim. PMID 2676467.
- Iqbal, I. Z.; Jones, G. H.; Dawe, N.; Mamais, C.; Smith, M. E.; Williams, R. J.; Kuhn, I.; Carrie, S. (December 2017). "Intranasal packs and haemostatic agents for the management of adult epistaxis: systematic review". The Journal of Laryngology & Otology. 131 (12): 1065–1092. doi:10.1017/S0022215117002055. ISSN 0022-2151. PMID 29280695.
- Killick, N; Malik, V; Nirmal Kumar, B (Mar 2014). "Nasal packing for epistaxis: an evidence-based review". British Journal of Hospital Medicine. 75 (3): 143–7. doi:10.12968/hmed.2014.75.3.143. PMID 24621629.
- Béquignon, E.; Teissier, N.; Gauthier, A.; Brugel, L.; Kermadec, H. De; Coste, A.; Prulière-Escabasse, V. (2017-08-01). "Emergency Department care of childhood epistaxis". Emerg Med J. 34 (8): 543–548. doi:10.1136/emermed-2015-205528. ISSN 1472-0205. PMID 27542804.
- MedlinePlus Medical Encyclopedia: Nosebleed U.S. National Library of Medicine Medline Plus service. Retrieved 2010-03-15.
- Villwock, JA; Jones, K (Dec 2013). "Recent trends in epistaxis management in the United States: 2008–2010". JAMA Otolaryngology–Head & Neck Surgery. 139 (12): 1279–84. doi:10.1001/jamaoto.2013.5220. PMID 24136624.
- Folz, BJ; Kanne, M; Werner, JA (November 2008). "[Current aspects in epistaxis]". HNO. 56 (11): 1157–65, quiz 1166. doi:10.1007/s00106-008-1838-3. PMID 18936903.
- al.], edited by Roger Jones ... [et (2004). Oxford textbook of primary medical care (repr. ed.). Oxford: Oxford University Press. p. 711. ISBN 9780198567820.CS1 maint: extra text: authors list (link)
- Bissonnette, Bruno (2010). Pediatric Anesthesia. New York: McGraw-Hill Medical. p. 1182. ISBN 9781607950936.
- al.], A.Y. Elzouki ... [et (2011-10-29). Textbook of clinical pediatrics (2nd ed.). Berlin: Springer. p. 3968. ISBN 9783642022012.
- "Manga: The Complete Guide, reviewed by Richard von Busack". Metroactive. Retrieved 5 August 2011.
- Morgan, Joyce (February 10, 2007). "Superheroes for a complex world". The Sydney Morning Herald. Retrieved 5 August 2011.
- Tracey, Liz (30 August 2016). ""Stranger Things" and the Psychic Nosebleed". JSTOR Daily. Retrieved 6 November 2016.
- Meehan, Paul (2009-10-21). Cinema of the Psychic Realm: A Critical Survey. McFarland. p. 193. ISBN 9780786454747.
- Various (1984). Erdoes, Richard; Ortiz, Alfonso (eds.). American Indian Myths and Legends (2 ed.). Toronto, Ontario: Random House of Canada Limited. p. 274.
- "Finnish idioms and proverbs". saaressa.blogspot.fr. Retrieved 2017-12-19.
- OMG! Nosebleed! Say what?! Retrieved 28 August 2013
- "Doen alsof je neus bloedt". OnzeTaal. Retrieved 8 June 2020.