Motor nerve
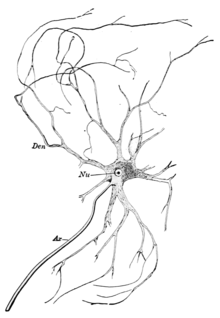
A motor nerve is a nerve located in the central nervous system (CNS), usually the spinal cord, that sends motor signals from the CNS to the muscles of the body. This is different from the motor neuron, which includes a cell body and branching of dendrites, while the nerve is made up of a bundle of axons. Motor nerves act as efferent nerves which carry information out from the CNS, as opposed to afferent nerves (also called sensory nerves), which send signals from sensory receptors in the periphery to the CNS.[1] There are also nerves that serve as both sensory and motor nerves called mixed nerves.[2]
| Motor nerve | |
|---|---|
| Details | |
| Identifiers | |
| Latin | nervus motorius |
| FMA | 5867 |
| Anatomical terms of neuroanatomy | |
Structure and function
Motor nerve fibers transduce signals from the CNS to peripheral neurons of proximal muscle tissue. Motor nerve axon terminals innervate skeletal and smooth muscle, as they are heavily involved in muscle control. Motor nerves tend to be rich in Acetylcholine vesicles because the motor nerve, a bundle of motor nerve axons that deliver motor signals and signal for movement and motor control.[3] Calcium vesicles reside in the axon terminals of the motor nerve bundles. The high calcium concentration outside of presynaptic motor nerves increases the size of EPPs (End-Plate potentials).[4]
Protective tissues
Within motor nerves, each axon is wrapped by the endoneurium, which is a layer of connective tissue that surrounds the myelin sheath. Bundles of axons are called fascicles, which are wrapped in perineurium. All of the fascicles wrapped in the perineurium are wound together and wrapped by a final layer of connective tissue known as the epineurium. These protective tissues defend nerves from injury, pathogens and help to maintain nerve function. Layers of connective tissue maintain the rate at which nerves conduct action potentials.[5]
_(14742157516).jpg)
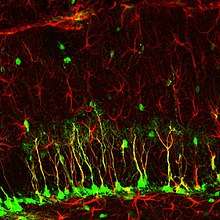
Spinal cord exit
Most motor pathways originate in the motor cortex of the brain. Signals run down the brainstem and spinal cord ipsilaterally, on the same side, and exit the spinal cord at the ventral horn of the spinal cord on either side. Motor nerves communicate with the muscle cells they innervate through motor neurons once they exit the spinal cord.[1][5]
Motor nerve types
Motor nerves can vary based on the subtype of motor neuron they are associate with.[6]
Alpha
Alpha motor neurons target extrafusal muscle fibers. The motor nerves associated with these neurons innervate extrafusal skeletal muscle fibers and are responsible for muscle contraction. These nerve fibers have the largest diameter of the motor neurons and require the highest conduction velocity of the three types.[6]
Beta
Beta motor neurons innervate intrafusal fibers of muscle spindles. These nerves are responsible for signaling slow twitch muscle fibers.[6]
Gamma
Gamma motor neurons, unlike alpha motor neurons, are not directly involved in muscle contraction. The nerves associated with these neurons do not send signals that directly adjust the shortening or lengthening of muscle fibers. However, these nerves are important in keeping muscle spindles taut.[6]
Neurodegeneration
Motor neural degeneration is the progressive weakening of neural tissues and connections in the nervous system. Muscles begin to weaken as there are no longer any motor nerves or pathways that allows for muscle innervation. Motor neuron diseases can be viral, genetic or be a result of environmental factors. The exact causes remain unclear, however many experts believe that toxic and environmental factors play a large role.[7]
Neuroregeneration
There are problems with neuroregeneration due to many sources, both internal and external. There is a weak regenerative ability of nerves and new nerve cells cannot simply be made. The outside environment can also play a role in nerve regeneration. Neural stem cells (NSCs), however, are able to differentiate into many different types of nerve cells. This is one way that nerves can "repair" themselves. NSC transplant into damaged areas usually leads to the cells differentiating into astrocytes which assists the surrounding neurons. Schwann cells have the ability to regenerate, but the capacity that these cells can repair nerve cells declines as time goes on as well as distance the Schwann cells are from site of damage.[8][9][10][11]
References
- Slater, Clarke R. (2015-11-01). "The functional organization of motor nerve terminals". Progress in Neurobiology. 134: 55–103. doi:10.1016/j.pneurobio.2015.09.004. ISSN 0301-0082. PMID 26439950.
- Glass, Jonathan D (2018-03-19). "Neuromuscular Disease: Protecting the nerve terminals". eLife. 7. doi:10.7554/eLife.35664. ISSN 2050-084X. PMC 5858932. PMID 29553367.
- Purves, Dale (2012). Neuroscience 5th Edition. Sunderland, Mass.
- Jang, Sung Ho; Lee, Han Do (December 2017). "Gait recovery by activation of the unaffected corticoreticulospinal tract in a stroke patient: A case report". Medicine. 96 (50): e9123. doi:10.1097/MD.0000000000009123. ISSN 0025-7974. PMC 5815724. PMID 29390312.
- C., Guyton, Arthur (2006). Textbook of medical physiology. Hall, John E. (John Edward), 1946- (11th ed.). Philadelphia: Elsevier Saunders. ISBN 978-0721602400. OCLC 56661571.
- 1825-1861., Gray, Henry (1989). Gray's anatomy. Williams, Peter L. (Peter Llewellyn), Gray, Henry, 1825-1861. (37th ed.). Edinburgh: C. Livingstone. ISBN 978-0443041778. OCLC 18350581.CS1 maint: numeric names: authors list (link)
- "Motor Neuron Disease".
- "Peripheral Nerve Disorders - Columbia Neurosurgery". Columbia Neurosurgery. Retrieved 2018-03-26.
- Gordon, Tessa (2016-05-01). "Nerve Regeneration: Understanding Biology and Its Influence on Return of Function After Nerve Transfers". Hand Clinics. 32 (2): 103–117. doi:10.1016/j.hcl.2015.12.001. ISSN 0749-0712. PMID 27094884.
- Huang, Lixiang; Wang, Gan (2017). "The Effects of Different Factors on the Behavior of Neural Stem Cells". Stem Cells International. 2017: 9497325. doi:10.1155/2017/9497325. ISSN 1687-966X. PMC 5735681. PMID 29358957.
- "Nerve Injuries - OrthoInfo - AAOS". Retrieved 2018-03-26.