Metoidioplasty
Metoidioplasty or metaoidioplasty (informally called a meto or meta) is a female-to-male sex reassignment surgery.[1]

| Part of a series on |
| Transgender topics |
|---|
|
|
|
Health care and medicine |
|
Rights issues
|
|
Society and culture
|
|
By country
|
|
|
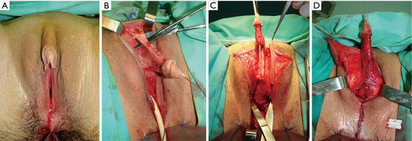
Testosterone replacement therapy gradually enlarges the clitoris to a mean maximum size of 4.6 cm (1.6–2 in)[2] (as the clitoris and the penis are developmentally homologous). In a metoidioplasty, the urethral plate and urethra are completely dissected from the clitoral corporeal bodies, then divided at the distal end, and the testosterone-enlarged clitoris straightened out and elongated. A longitudinal vascularized island flap is configured and harvested from the dorsal skin of the clitoris, reversed to the ventral side, tubularized and an anastomosis is formed with the native urethra. The new urethral meatus is placed along the neophallus to the distal end and the skin of the neophallus and scrotum reconstructed using labia minora and majora flaps.[3] The new neophallus ranges in size from 4-10 cm (with an average of 5.7 cm) and has the approximate girth of a human adult thumb. [4]
Comparison with phalloplasty
Metoidioplasty is technically simpler than phalloplasty, costs less, and has fewer potential complications. However, phalloplasty patients are far more likely to be capable of sexual penetration (mainly due to size constraints) after they recover from surgery.[5]
In a phalloplasty, the surgeon fabricates a neopenis by grafting tissue from a donor site (such as from the patient's back, arm or leg). A phalloplasty takes about 8–10 hours to complete (the first stage), and is generally followed by multiple (up to 3) additional surgical procedures including glansplasty, scrotoplasty, testicular prosthesis, and/or penile implant.
Metoidioplasty typically requires 2–3 hours to complete. Because the clitoris' erectile tissue functions normally, a prosthesis is unnecessary for erection (although the clitoris might not become as rigid as a penile erection). In nearly all cases, metoidioplasty patients can continue to have clitoral orgasms after surgery.
Operation
- After patient prep, the skin surrounding the enlarged clitoris is incised on the underside and the lateral crura, which suspend the tissue in place, are cut, freeing the clitoral tissue from the pubic bone.
- If the urethra is to be extended, the process starts now using mucosal tissues from either the vaginal area or from inside the mouth/cheeks. An experimental option is a graft from the intestines. The labia minora can be used to protect the graft, as well as provide greater girth. A catheter is placed in the extension to facilitate healing for two to three weeks.
- The neopenis is then provided with skin by cutting the labia minora and wrapping around the tissue and secured with stitches. Scrotoplasty is usually done at the same time as metoidioplasty surgery. Vaginectomy, hysterectomy and/or oophorectomy can also be performed at this time if they have not been done already.
Alternative techniques
If a metoidioplasty is performed without extending the urethra and/or a scrotoplasty, this is sometimes called a clitoral release. This is less expensive than a complete metoidioplasty but does not allow for urination through the neopenis while standing. However this also offers surgery with less risk because the urinary system remains unaltered without a urethral extension, and still affords some of the visual effects of a complete metoidioplasty along with the ability to use the neopenis for sexual penetration. Vaginectomy is an option with this surgery.
Penile Implants
| Companies | Year | Model | Images | Description |
|---|---|---|---|---|
| ZSI | 2017 | ZSI 100 D4 IN LYON |  Metoidioplasty Implant |
Bendable and "positionable" rods are inserted into the penis. The rods have an outer coating of silicone and inner stainless steel core or interlocking plastic joints. Non inflatable (or semi-rigid) implants are always firm. They can be bent into different positions for erect and flaccid states |
Complications
Complications occur in up to 50% of surgeries, varying in severity between those requiring only minor supportive care to those requiring surgical correction. Complications include bleeding from the surgical site that may require surgery, bacterial infections, ileus, wound dehiscence, tissue necrosis, urinary fistula requiring surgical correction, urethral stricture, loss of sensation (uncommon), anorgasmia, scarring of varying degrees. [6] In a study of post-operative trans men, 28% of patients who had the urethra extended had temporary swelling resulting in dribbling and spraying of urine; no medical intervention was needed. There was only a small chance of urethral strictures (narrowing of the urethra) and less than 10% had instance of a fistula (hole in the urethra) requiring minor revision. The average neophallic length after was 5.7 cm (with a range 4–10 cm). All patients reported ability to achieve an erection and normal sensation. In patients who had scrotoplasty, some have reported rejection or complications related to the testicular prostheses.
See also
- List of transgender-related topics
- Penile Implant
Notes
- Metoidioplasty: a variant of phalloplasty in female transsexuals by S.V. Perovic and M.L. Djordjevic (BJU International, Volume 92 Issue 9, December 2003)
- Physical and hormonal evaluation of transsexual patients: A longitudinal study by Meyer W, et al. (Archives of Sexual Behavior, Volume 15, Number 2, April 1986)
- Perovic, S. and Djordjevic, M. (2003), Metoidioplasty: a variant of phalloplasty in female transsexuals. BJU International, 92: 981-985. doi:10.1111/j.1464-410X.2003.04524.x
- Metoidioplasty as a Single Stage Sex Reassignment Surgery in Female Transsexuals: Belgrade Experience Djordjevic, Miroslav L. et al., Journal of Sexual Medicine, Volume 6, Issue 5, 1306 - 1313
- Frey, Jordan D. et al. “A Systematic Review of Metoidioplasty and Radial Forearm Flap Phalloplasty in Female-to-Male Transgender Genital Reconstruction: Is the ‘Ideal’ Neophallus an Achievable Goal?” Plastic and Reconstructive Surgery Global Open 4.12 (2016): e1131. PMC. Web. 5 July 2018.
- http://www.gendersurgeryamsterdam.com/operation-female-male/metaidoioplasty/complications/
- Metoidioplasty as a Single Stage Sex Reassignment Surgery in Female Transsexuals: Belgrade Experience by Miroslav L. Djordjevic, Dusan Stanojevic (Journal of Sexual Medicine, Volume 6 Issue 5, Oct 2008)
- Metaidoioplasty: An Alternative Phalloplasty Technique in Transsexuals by Hage, J. Joris (Journal of Plastic & Reconstructive Surgery, Volume 97 Issue 1, January 1996)
- Gender Reassigment by Dan Greenwald and Wayne Stadelmann (eMedicine Journal, Volume 2 Number 7, July 6, 2001)