Management of schizophrenia
The management of schizophrenia usually involves many aspects including psychological, pharmacological, social, educational, and employment-related interventions directed to recovery, and reducing the impact of schizophrenia on quality of life, social functioning, and longevity.[1]
| Management of schizophrenia | |
|---|---|
| Specialty | Psychiatry |
Hospitalization
Hospitalization may occur with severe episodes of schizophrenia. This can be voluntary or (if mental health legislation allows it) involuntary (called civil or involuntary commitment). Long-term inpatient stays are now less common due to deinstitutionalization, although still occur.[2] Following (or in lieu of) a hospital admission, support services available can include drop-in centers, visits from members of a community mental health team or Assertive Community Treatment team, supported employment[3] and patient-led support groups. Efforts to avoid repeated hospitalization include the obtaining of community treatment orders which, following judicial approval, coerce the affected individual to receive psychiatric treatment including long-acting injections of anti-psychotic medication. This legal mechanism has been shown to increase the affected patient's time out of the hospital.[4]
Medication
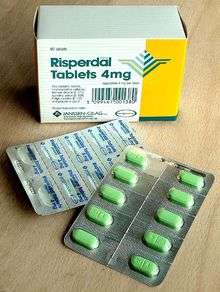
The mainstay of psychiatric treatment for schizophrenia is an antipsychotic medication.[5] Medication might improve a number of outcomes found to be important to patients, including positive, acute and psychotic symptoms, and social and vocational functioning.[6] Medication can reduce the "positive" symptoms of psychosis. Most antipsychotics are thought to take around 7 to 14 days to have their main effect. However, these drugs fail to significantly improve the negative symptoms and cognitive dysfunction.[7][8] There is evidence of clozapine, amisulpride, olanzapine, and risperidone being the most effective medications, although a high proportion of studies of risperidone were undertaken by its manufacturer, Janssen-Cilag, and should be interpreted with this in mind.[9] In those on antipsychotics, continued use decreases the risk of relapse.[10][11] There is little evidence regarding consistent benefits from their use beyond two or three years.[11]
Treatment of schizophrenia changed dramatically in the mid-1950s with the development and introduction of the first antipsychotic chlorpromazine.[12] Others such as haloperidol and trifluoperazine soon followed.
It remains unclear whether the newer antipsychotics reduce the chances of developing neuroleptic malignant syndrome, a rare but serious and potentially fatal neurological disorder most often caused by an adverse reaction to neuroleptic or antipsychotic drugs.[13]
Most people on antipsychotics get side effects. People on typical antipsychotics tend to have a higher rate of extrapyramidal side effects while some atypicals are associated with considerable weight gain, diabetes, and risk of metabolic syndrome; this is most pronounced with olanzapine, while risperidone and quetiapine are also associated with weight gain.[9] Risperidone has a similar rate of extrapyramidal symptoms to haloperidol.[9] The American Psychiatric Association generally recommends that atypicals be used as first line treatment in most patients, but further states that therapy should be individually optimized for each patient.[14]
The response of symptoms to medication is variable; treatment-resistant schizophrenia is the failure to respond to two or more antipsychotic medications given in therapeutic doses for six weeks or more.[15] Patients in this category may be prescribed clozapine, a medication that may be more effective at reducing symptoms of schizophrenia, but treatment may come with a higher risk of several potentially lethal side effects including agranulocytosis and myocarditis.[16][17] Clozapine is the only medication proven to be more effective for people who do not respond to other types of antipsychotics.[18] It also appears to reduce suicide in people with schizophrenia. As clozapine suppresses the development of bone marrow, in turn reducing white blood cells which can lead to infection, blood tests are taken for the first six months on this medication.[19] The risk of experiencing agranulocytosis due to clozapine treatment is higher in elderly people, children, and adolescents.[16] The effectiveness in the studies also needs to be interpreted with caution as the studies may have an increased risk of bias.[16]
Sometimes the use of a second antipsychotic in combination with another is recommended where there has been a poor response. A review of this use found some evidence for an improvement in symptoms but not for relapse or hospitalisation. Other strategies used add a mood stabiliser, ECT, or rTMS but evidence for these is lacking. The use of combination antipsychotics is increasing in spite of limited supporting evidence, with some countries including Finland, France, and the UK recommending its use and others including Canada, Denmark, and Spain in opposition.[20]
Add on agents
Note: Only adjuncts for which at least one double-blind randomized placebo-controlled trial has provided support are listed in this table.
| Adjuncts[21][22] | Symptoms against which efficacy is known | Notable adverse effects seen in clinical trials | Highest quality of clinical data available | N | Notes |
|---|---|---|---|---|---|
| Adjuncts to clozapine[23][24] | |||||
| Antipsychotics | |||||
| Amisulpride | Global | Extrapyramidal side effects (e.g. tremor, dystonia, akathisia, etc.), headache, somnolence, insomnia, elevated serum prolactin, etc. | 1 DB-RPCTs | 16 | Not approved for use in the US or Canada. Approved for use in Australia, Europe and several countries in East Asia. Can prolong the QT interval, some in vivo evidence[25] suggests it may have anti-diabetogenic effects and hence may improve metabolic parameters in patients on clozapine. |
| Aripiprazole | Global, esp. negative | Akathisia | 1 DB-RPCT | 61 | Can also improve metabolic side effects of clozapine (including body weight). Six studies so far; only one negative. |
| Risperidone | Global | Impaired cognitive functioning, prolactin elevation and hyperglycaemia | 2 DB-RPCTs, 1 DB-RCT | 357 (DB-RPCTs) & 24 (DB-RCT) | 11 studies have been conducted, 5 negative. A meta-analysis[23] found no clinically significant difference between risperidone augmentation and placebo augmentation. |
| Sulpiride | Global | Increased serum prolactin | 1 DB-RPCT | 28 | Not approved for use in the US, Canada and Australia. |
| Ziprasidone | Global | QTc interval prolongation | 1 DB-RCT | 24 | Was compared with risperidone in the one DB-RCT. |
| Antidepressants | |||||
| Citalopram | Negative symptoms | Well tolerated | 1 DB-RPCT | 61 | Can prolong the QT interval and since clozapine can prolong the QT interval too it is advisable to avoid their concurrent use in patients with cardiovascular risk factors. |
| Fluvoxamine | Negative and depressive symptoms | Elevated serum levels of clozapine (via inhibition of P450 cytochromes) | Open-label studies | NA | Improved metabolic parameters |
| Mirtazapine | Negative, depressive and cognitive symptoms | Weight gain | 2 DB-RPCTs (1 negative) | 80 | 5-HT2A/2C/3 & α2 adrenoceptor antagonist |
| Anticonvulsants | |||||
| Lamotrigine | Negative & depressive symptoms | Stevens–Johnson syndrome, toxic epidermal necrolysis, etc. | 4 DB-RPCTs (2 negative) | 108 | Usually a relatively well tolerated anticonvulsant, but because of risk of potentially-fatal dermatologic AEs the dose must be slowly titrated up in order to prevent these AEs. A meta-analysis[23] found that it was ineffective. |
| Topiramate | Negative symptoms | Cognitive impairment, sedation, asthenia | 2 DB-RPCTs (1 negative) | 57 | Can cause cognitive impairment and hence should probably be avoided in patients with cognitive impairments. |
| Valproate | Reduced anxiety & depression | Weight gain, hair loss | One open-label study comparing it with lithium | NA | Increases the expression of mGluR2 and GAD67 via histone deacetylase (HDAC) inhibition. |
| Glutamatergic agents[26][27] | |||||
| CX-516 | Global | Well tolerated | 1 DB-RPCT | 18 | Statistically significant improvement in total symptoms but no significant improvement in negative and positive symptoms when considered separately. |
| Memantine | Global | Well tolerated | 1 DB-RPCT | 21 | Statistically significant improvement in negative and total symptomtology. |
| Other | |||||
| Lithium | Global | Weight gain, hypersalivation | 1 DB-RPCT, 1 DB-RCT | 10 (DB-RPCT), 20 (DB-RCT) | Increased risk of neurological side effects such as neuroleptic malignant syndrome. |
| E-EPA | Global (especially negative and cognitive symptoms) | Well tolerated | 3 DB-RPCT (1 negative) | 131 | Ester of the ω-3 fatty acid, eicosapentaenoic acid. |
| Adjuncts to other antipsychotics | |||||
| Anti-inflammatory agents[28][29] | |||||
| Aspirin[30] | Global (especially positive symptoms) | Well tolerated | 1 DB-RPCT | 70 | Increased risk of bleeding, but seems relatively well tolerated. |
| Celecoxib | Global (especially negative symptoms) | Well tolerated | 3 DB-RPCTs (1 negative) | 147 | May increased the risk of cardiovascular events (which is particularly worrisome as schizophrenia patients are a higher risk group for cardiovascular events). Case series (N=2) suggests efficacy in augmenting clozapine. |
| Minocycline[31][32][33][34] | Global | Well tolerated | 4 DB-RPCTs | 164 | Increased risk of blood dyscarsias. |
| ω-3 fatty acids | Global | Well tolerated | 6 DB-RPCTs (1 negative)[35] | 362 | May have protective effects against depression. |
| Pregnenolone[36][37][38][39] | Global | Well tolerated | 3 DB-RPCTs | 100 | Levels of this neurosteroid in the body are elevated by clozapine treatment. |
| Glutamatergics[26][40] | |||||
| D-alanine[41][42] | Global | Well tolerated | 1 DB-RPCT | 31 | A D-amino acid with affinity towards the glycine site on the NMDA receptor. |
| D-serine | Global (especially negative symptoms) | Well tolerated | 4 DB-RPCTs | 183 | Affinity towards the glycine site on NMDA receptors. D. Souza 2013,[43] Heresco-Levy 2005,[44] Lane 2005,[45] Lane 2010,[46] Tsai 1999,[47] Weiser 2012[48] |
| Glycine | Global (predominantly positive symptoms) | Well tolerated | 5 DB-RPCTs | 219 | Endogenous NMDA receptor ligand. |
| N-acetylcysteine[49] | Global (especially negative symptoms) | Well tolerated | 3 DB-RPCTs | 140 | Cystine and glutathione prodrug.[50][51] Cystine increases intracellular glutamate levels via the glutamate-cystine anti porter.
Berk 2008,[52] Berk 2011,[53] Carmeli 2012,[54] Lavoie 2008[55] |
| Sarcosine | Global (especially negative symptoms) | Well tolerated | 3 DB-RPCTs | 112 | GlyT1 antagonist (i.e. glycine reuptake inhibitor). Also known as N-methylglycine. Lane 2005,[45] Lane 2006,[56] Lane 2008,[57] Lane 2010,[46] Tsai 2004[58] |
| Cholinergics[59][60][61] | |||||
| Donepezil | Global | Well tolerated | 6 DB-RPCTs (5 negative; or 12 DB-RPCTs if one includes cross-over trials; 8 negative in total) | 378, 474 (including cross-over trials) | Possesses antidepressant effects according to one trial. |
| Galantamine | Cognition | Well tolerated | 5 DB-RPCTs (1 negative) | 170 | Robust nootropic |
| Rivastigmine | Cognition | Well tolerated | 3 DB-RPCTs (all 3 negative; 5 trials including cross-over trials; 4 negative) | 93, 131 (including cross-over trials) | Seems to be a weaker nootropic |
| Tropisetron†[62][63][64][65] | Cognitive and negative symptoms | Well tolerated | 3 DB-RPCTs | 120 | Agonist at α7 nAChRs; antagonist at 5-HT3. Expensive (>$20 AUD/tablet). |
| Antidepressants[66] | |||||
| Escitalopram†[67] | Negative symptoms | Well tolerated | 1 DB-RPCT | 40 | May increase risk of QT interval prolongation. |
| Fluoxetine | Negative symptoms | Well tolerated | 4 DB-RPCTs (3 negative) | 136 | The safest of antidepressants listed here in overdose.[68] Risk of QT interval prolongation is lower than with escitalopram (but still exists). |
| Mianserin[69] | Negative and cognitive symptoms | Well tolerated | 2 DB-RPCTs | 48 | Weight gain, sedation, dry mouth, constipation and dizziness. Blood dyscarsias are a possible adverse effect and both the Australian Medicines Handbook and British National Formulary 65 (BNF 65) recommend regular complete blood counts to be taken.[70][71] |
| Mirtazapine[69] | Cognition,[72][73] negative and positive symptoms†[74] | Well tolerated | ≥4 DB-RPCTs (one negative) | 127 | Relatively safe in overdose. Produces significant sedation and weight gain, however, which could potentially add to the adverse effects of atypical antipsychotics. Can reduce antipsychotic-induced akathisia.[75] |
| Ritanserin | Negative symptoms | Well tolerated | 2 DB-RPCTs | 73 | 5-HT2A/2C antagonist. Not clinically available. |
| Trazodone | Negative symptoms | Well tolerated | 2 DB-RPCTs | 72 | 5-HT2A antagonist and SSRI. Has sedative effects and hence might exacerbate some of the side effects of atypical antipsychotics. |
| Other | |||||
| Alpha-lipoic acid[76][77] | Weight gain | Well tolerated | 1 DB-RPCT | 360 | Offset antipsychotic drug-induced weight gain. Increased total antioxidant status. May also increase GSH:GSSG (reduced glutathione:oxidized glutathione) ratio.[78] |
| L-Theanine[79][80][81] | Positive, activation, and anxiety symptoms | Well tolerated | 2 DB-RPCTs | 40 | Glutamic acid analog. Primary study noted reduction in positive, activation, and anxiety symptoms. Additional studies have noted improvements in attention.[82][83][84][85] Research suggests that theanime has a regulatory effect on the nicotine acetylcholine receptor-dopamine reward pathway, and was shown to reduced dopamine production in the midbrain of mice.[86] |
| Famotidine†[87] | Global | Well tolerated | 1 DB-RPCT | 30 | May reduce the absorption of vitamin B12 from the stomach. Might also increase susceptibility to food poisoning. |
| Ginkgo biloba | Tardive dyskinesia, positive symptoms | Well tolerated | 4 DB-RPCTs | 157 | Atmaca 2005,[88] Doruk 2008,[89] Zhang 2001,[90] Zhang 2001,[91] Zhang 2006,[92] Zhang 2011,[93] Zhou 1999[94] |
| Ondansetron[95] | Negative and cognitive symptoms | Well tolerated | 3 DB-RPCTs | 151 | 5-HT3 antagonist. May prolong the QT interval. Expensive (>$4 AUD/tablet). |
| SAM-e[96] | Aggression | Well tolerated | 1 DB-RPCT | 18 | Study noted improvement of aggressive behavior and quality of life impairment. while in another study SAM-e has been purported to have a contributory effect on psychosis [97] |
| Vitamin C[98][99][100][101] | Global | Well tolerated | 1 DB-RPCT | 40 | Improves BPRS scores. |
Acronyms used:
DB-RPCT — Double-blind randomized placebo-controlled trial.
DB-RCT — Double-blind randomized controlled trial.
Note: Global in the context of schizophrenia symptoms here refers to all four symptom clusters.
- N refers to the total sample sizes (including placebo groups) of DB-RCTs.
† No secondary sources could be found on the utility of the drug in question, treating the symptom in question (or any symptom in the case of where † has been placed next to the drug's name).
Psychosocial
Psychotherapy is also widely recommended, though not widely used in the treatment of schizophrenia, due to reimbursement problems or lack of training. As a result, treatment is often confined to psychiatric medication.[102]
Cognitive behavioral therapy (CBT) is used to target specific symptoms and improve related issues such as self-esteem and social functioning. Although the results of early trials were inconclusive[103] as the therapy advanced from its initial applications in the mid-1990s, meta-analytic reviews suggested CBT to be an effective treatment for the psychotic symptoms of schizophrenia.[104][105] Nonetheless, more recent meta analyses have cast doubt upon the utility of CBT as a treatment for the symptoms of psychosis[106][107][108]
Another approach is cognitive remediation therapy, a technique aimed at remediating the neurocognitive deficits sometimes present in schizophrenia. Based on techniques of neuropsychological rehabilitation, early evidence has shown it to be cognitively effective, resulting in the improvement of previous deficits in psychomotor speed, verbal memory, nonverbal memory, and executive function, such improvements being related to measurable changes in brain activation as measured by fMRI.[109]
Metacognitive training: In view of many empirical findings [110] suggesting deficits of metacognition (thinking about one's thinking, reflecting upon one's cognitive process) in patients with schizophrenia, metacognitive training (MCT) [110][111] is increasingly adopted as a complementary treatment approach. MCT aims at sharpening the awareness of patients for a variety of cognitive biases (e.g. jumping to conclusions, attributional biases, over-confidence in errors), which are implicated in the formation and maintenance of schizophrenia positive symptoms (especially delusions),[112] and to ultimately replace these biases with functional cognitive strategies.
The training consists of 8 modules and can be obtained cost-free from the internet in 15 languages.[110][111] Studies confirm the feasibility [113] and lend preliminary support to the efficacy [110][114][115] of the intervention. Recently, an individualized format has been developed which combines the metacognitive approach with methods derived from cognitive-behavioral therapy.[116]
Family Therapy or Education, which addresses the whole family system of an individual with a diagnosis of schizophrenia, may be beneficial, at least if the duration of intervention is longer-term.[117][118][119] A 2010 Cochrane review concluded that many of the clinical trials that studied the effectiveness of family interventions were poorly designed, and may over estimate the effectiveness of the therapy. High-quality randomized controlled trials in this area are required.[119] Aside from therapy, the impact of schizophrenia on families and the burden on careers has been recognized, with the increasing availability of self-help books on the subject.[120][121] There is also some evidence for benefits from social skills training, although there have also been significant negative findings.[122][123] Some studies have explored the possible benefits of music therapy and other creative therapies.[124][125][126]
The Soteria model is alternative to inpatient hospitalization using full non professional care and a minimal medication approach.[127] Although evidence is limited, a review found the programme equally as effective as treatment with medications but due to the limited evidence did not recommend it as a standard treatment.[128] Training in the detection of subtle facial expressions has been used to improve facial emotional recognition.[129]
Supplements
Disruption of the gut microbiota has been linked to inflammation, and disorders of the central nervous system. This includes schizophrenia, and probiotic supplementation has been proposed to improve its symptoms. A review found no evidence to support this but it concludes that probiotics may be of benefit in regulating bowel movements and lessening the metabolic effects of antipsychotics.[130]
A review explains the need for an optimal level of vitamin D and omega-3 fatty acids for the proper synthesis and control of the neurotransmitter serotonin. Serotonin regulates executive function, sensory gating, and social behavior – all of which are commonly impaired in schizophrenia. The model proposed suggests that supplementation would help in preventing and treating these brain dysfunctions.[131] Another review finds that omega-3 fatty acids and vitamin D are among the nutritional factors known to have a beneficial effect on mental health.[132] A Cochrane review found evidence to suggest that the use of omega-3 fatty acids in the prodromal stage may prevent the transition to psychosis but the evidence was poor quality and further studies were called for.[133]
Traditional Chinese medicine
Acupuncture is a procedure generally known to be safe and with few adverse effects. A Cochrane review found limited evidence for its possible antipsychotic effects in the treatment of schizophrenia and called for more studies.[134] Another review found limited evidence for its use as an add-on therapy for the relief of symptoms but positive results were found for the treatment of sleep disorders that often accompany schizophrenia.[135]
Wendan decoction is a classic herbal treatment in traditional Chinese medicine used for symptoms of psychosis, and other conditions. Wendan decoction is safe, accessible, and inexpenive, and a Cochrane review was carried out for its possible effects on schizophrenia symptoms. Limited evidence was found for its positive antipsychotic effects in the short term, and it was associated with fewer adverse effects. Used as an add-on to an antipsychotic, wider positive effects were found. Larger studies of improved quality were called for.[136][137]
Other
Various brain stimulation techniques have been used to treat the positive symptoms of schizophrenia, in particular auditory verbal hallucinations (AVHs), and investigations are ongoing.[138] Most studies focus on transcranial direct-current stimulation (tDCM), and repetitive transcranial magnetic stimulation (rTMS).[139] Transcranial magnetic stimulation is low-cost, noninvasive, and almost free of side-effects making it a good therapeutic choice with promising outcomes.[138] Low-frequency TMS of the left temperoparietal cortex (the region containing Broca's area) can reduce auditory hallucinations.[138] rTMS seems to be the most effective treatment for those with persistent AVHs, as an add-on therapy.[139] AVHs are not resolved in up to 30 per cent of those on antipsychotics and a further percentage still experience only a partial response.[139] Techniques based on focused ultrasound for deep brain stimulation could provide insight for the treatment of AVHs.[139]
An established brain stimulation treatment is electroconvulsive therapy. This is not considered a first-line treatment but may be prescribed in cases where other treatments have failed. It is more effective where symptoms of catatonia are present,[140] and is recommended for use under NICE guidelines in the UK for catatonia if previously effective, though there is no recommendation for use for schizophrenia otherwise.[141] Psychosurgery has now become a rare procedure and is not a recommended treatment for schizophrenia.[142]
A study in 2014 conducted by an Australian researcher indicated that the pericarp powder of Garcinia mangostana L. have the ability to reduce oxidative stress as an effective treatment for schizophrenia by increasing glutathione S-transferase levels which enhances mitochondrial activity over a period of 180 days under a sustained intake of 1000 mg/day.[143][144]
There may be some benefit in trying several treatment modalities at the same time, especially those that could be classed as lifestyle interventions.[145]
Peer support in which people with experiential knowledge of mental illness provide knowledge, experience, emotional, social or practical help to each other is considered an important aspect of coping with schizophrenia and other serious mental health conditions. A 2019 Cochrane reviews of evidence for peer-support interventions compared to supportive or psychosocial interventions were unable to support or refute the effectiveness of peer-support due to limited data.[146]
References
- "Psychosis and schizophrenia in adults: treatment and management | Key-priorities-for-implementation | Guidance and guidelines | NICE".
- Becker T, Kilian R (2006). "Psychiatric services for people with severe mental illness across western Europe: what can be generalized from current knowledge about differences in provision, costs and outcomes of mental health care?". Acta Psychiatrica Scandinavica Supplementum. 113 (429): 9–16. doi:10.1111/j.1600-0447.2005.00711.x. PMID 16445476.
- McGurk, SR; Mueser, KT; Feldman, K; Wolfe, R; Pascaris, A (2007). "Cognitive training for supported employment: 2-3 year outcomes of a randomized controlled trial". The American Journal of Psychiatry. 164 (3): 437–41. doi:10.1176/appi.ajp.164.3.437. PMID 17329468.
- Effects of compulsory treatment orders on time to hospital readmission (2005).
- The Royal College of Psychiatrists & The British Psychological Society (2003). Schizophrenia. Full national clinical guideline on core interventions in primary and secondary care Archived 2007-09-27 at the Wayback Machine (PDF). London: Gaskell and the British Psychological Society. Retrieved on 2007-05-17.
- Eiring, O.; Landmark, B. F.; Aas, E.; Salkeld, G.; Nylenna, M.; Nytroen, K. (2015). "What matters to patients? A systematic review of preferences for medication-associated outcomes in mental disorders". BMJ Open. 5 (4): e007848. doi:10.1136/bmjopen-2015-007848. PMC 4390680. PMID 25854979.
- Smith T, Weston C, Lieberman J (August 2010). "Schizophrenia (maintenance treatment)". American Family Physician. 82 (4): 338–9. PMID 20704164.
- Tandon R, Keshavan MS, Nasrallah HA (March 2008). "Schizophrenia, "Just the Facts": what we know in 2008 part 1: overview". Schizophrenia Research. 100 (1–3): 4–19. doi:10.1016/j.schres.2008.01.022. PMID 18291627.
- Barry SJ, Gaughan TM, Hunter R (2012). "Schizophrenia". BMJ Clinical Evidence. 2012. PMC 3385413. PMID 23870705. Archived from the original on 2014-09-11.
- Leucht S, Tardy M, Komossa K, et al. (June 2012). "Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis". Lancet. 379 (9831): 2063–71. doi:10.1016/S0140-6736(12)60239-6. PMID 22560607.
- Harrow M, Jobe TH (19 March 2013). "Does long-term treatment of dchizophrenia with antipsychotic medications facilitate recovery?". Schizophrenia Bulletin. 39 (5): 962–5. doi:10.1093/schbul/sbt034. PMC 3756791. PMID 23512950.
- Turner, T. (2007). "Chlorpromazine: Unlocking psychosis". BMJ. 334: s7. doi:10.1136/bmj.39034.609074.94. PMID 17204765.
- Ananth J, Parameswaran S, Gunatilake S, Burgoyne K, Sidhom T (2004). "Neuroleptic malignant syndrome and atypical antipsychotic drugs". Journal of Clinical Psychiatry. 65 (4): 464–70. doi:10.4088/JCP.v65n0403. PMID 15119907.
- "PsychiatryOnline | APA Practice Guidelines | Practice Guideline for the Treatment of Patients With Schizophrenia Second Edition". Archived from the original on 2014-03-06.
- Semple.David"Oxford Handbook Of Psychiatry". Oxford Press. 2005. p 207.
- Essali, Adib; Al-Haj Haasan, Nahla; Li, Chunbo; Rathbone, John (2009-01-21). "Clozapine versus typical neuroleptic medication for schizophrenia". Cochrane Database of Systematic Reviews (1): CD000059. doi:10.1002/14651858.cd000059.pub2. PMC 7065592. PMID 19160174.
- Haas SJ, Hill R, Krum H (2007). "Clozapine-associated myocarditis: a review of 116 cases of suspected myocarditis associated with the use of clozapine in Australia during 1993–2003". Drug Safety. 30 (1): 47–57. doi:10.2165/00002018-200730010-00005. PMID 17194170.
- Lieberman, Jeffrey A.; Stroup, T. Scott; McEvoy, Joseph P.; Swartz, Marvin S.; Rosenheck, Robert A.; Perkins, Diana O.; Keefe, Richard S.E.; Davis, Sonia M.; Davis, Clarence E.; Lebowitz, Barry D.; Severe, Joanne; Hsiao, John K.; Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators (2005). "Effectiveness of Antipsychotic Drugs in Patients with Chronic Schizophrenia". New England Journal of Medicine. 353 (12): 1209–23. doi:10.1056/NEJMoa051688. PMID 16172203.
- Kozier, B et al. (2008). Fundamentals Of Nursing, Concepts, Process, and Practice. London: Pearson Education. p. 189.
- Ortiz-Orendain J, Castiello-de Obeso S, Colunga-Lozano LE, et al. (June 2017). "Antipsychotic combinations for schizophrenia". Cochrane Database Syst Rev (Review). 6: CD009005. doi:10.1002/14651858.CD009005.pub2. PMC 6481822. PMID 28658515.
- Ritsner, MS (2013). Ritsner, Michael S (ed.). Polypharmacy in Psychiatry Practice, Volume I. Springer Science+Business Media Dordrecht. doi:10.1007/978-94-007-5805-6. ISBN 9789400758056.
- Ritsner, MS (2013). Ritsner, Michael S (ed.). Polypharmacy in Psychiatry Practice, Volume II. Springer Science+Business Media Dordrecht. doi:10.1007/978-94-007-5799-8. ISBN 9789400757998.
- Porcelli, S; Balzarro, B; Serretti, A (March 2012). "Clozapine resistance: augmentation strategies". European Neuropsychopharmacology. 22 (3): 165–182. doi:10.1016/j.euroneuro.2011.08.005. PMID 21906915.
- Sommer, IE; Begemann, MJ; Temmerman, A; Leucht, S (September 2012). "Pharmacological Augmentation Strategies for Schizophrenia Patients With Insufficient Response to Clozapine: A Quantitative Literature Review". Schizophrenia Bulletin. 38 (5): 1003–1011. doi:10.1093/schbul/sbr004. PMC 3446238. PMID 21422107.
- Roix, JJ; DeCrescenzo, GA; Cheung, PH; Ciallella, JR; Sulpice, T; Saha, S; Halse, R (April 2012). "Effect of the antipsychotic agent amisulpride on glucose lowering and insulin secretion". Diabetes, Obesity & Metabolism. 14 (4): 329–334. doi:10.1111/j.1463-1326.2011.01529.x. PMID 22059694.
- Singh, SP; Singh, V (October 2011). "Meta-Analysis of the Efficacy of Adjunctive NMDA Receptor Modulators in Chronic Schizophrenia". CNS Drugs. 25 (10): 859–885. doi:10.2165/11586650-000000000-00000. PMID 21936588.
- Choi, KH; Wykes, T; Kurtz, MM (September 2013). "Adjunctive pharmacotherapy for cognitive deficits in schizophrenia: meta-analytical investigation of efficacy". The British Journal of Psychiatry. 203 (3): 172–178. doi:10.1192/bjp.bp.111.107359. PMC 3759029. PMID 23999481.
- Keller, WR; Kum, LM; Wehring, HJ; Koola, MM; Buchanan, RW; Kelly, DL (April 2013). "A review of anti-inflammatory agents for symptoms of schizophrenia". Journal of Psychopharmacology. 27 (4): 337–342. doi:10.1177/0269881112467089. PMC 3641824. PMID 23151612.
- Sommer, I. E.; Van Westrhenen, R.; Begemann, M. J. H.; De Witte, L. D.; Leucht, S.; Kahn, R. S. (2013). "Efficacy of Anti-inflammatory Agents to Improve Symptoms in Patients with Schizophrenia: An Update". Schizophrenia Bulletin. 40 (1): 181–191. doi:10.1093/schbul/sbt139. PMC 3885306. PMID 24106335.
- Laan, W.; Grobbee, D. E.; Selten, J. P.; Heijnen, C. J.; Kahn, R. S.; Burger, H. (2010). "Adjuvant Aspirin Therapy Reduces Symptoms of Schizophrenia Spectrum Disorders" (PDF). The Journal of Clinical Psychiatry. 71 (5): 520–527. doi:10.4088/JCP.09m05117yel. hdl:11370/5644f8cd-b8ea-4ecc-9755-0f7c9ed86d02. PMID 20492850.
- Liu, F.; Guo, X.; Wu, R.; Ou, J.; Zheng, Y.; Zhang, B.; Xie, L.; Zhang, L.; Yang, L.; Yang, S.; Yang, J.; Ruan, Y.; Zeng, Y.; Xu, X.; Zhao, J. (2014). "Minocycline supplementation for treatment of negative symptoms in early-phase schizophrenia: A double blind, randomized, controlled trial". Schizophrenia Research. 153 (1–3): 169–76. doi:10.1016/j.schres.2014.01.011. PMID 24503176.
- Khodaie-Ardakani, M. R.; Mirshafiee, O.; Farokhnia, M.; Tajdini, M.; Hosseini, S. M. R.; Modabbernia, A.; Rezaei, F.; Salehi, B.; Yekehtaz, H.; Ashrafi, M.; Tabrizi, M.; Akhondzadeh, S. (2014). "Minocycline add-on to risperidone for treatment of negative symptoms in patients with stable schizophrenia: Randomized double-blind placebo-controlled study". Psychiatry Research. 215 (3): 540–6. doi:10.1016/j.psychres.2013.12.051. PMID 24480077.
- Chaudhry, I. B.; Hallak, J.; Husain, N.; Minhas, F.; Stirling, J.; Richardson, P.; Dursun, S.; Dunn, G.; Deakin, B. (2012). "Minocycline benefits negative symptoms in early schizophrenia: A randomised double-blind placebo-controlled clinical trial in patients on standard treatment". Journal of Psychopharmacology. 26 (9): 1185–1193. doi:10.1177/0269881112444941. PMID 22526685.
- Levkovitz, Y.; Mendlovich, S.; Riwkes, S.; Braw, Y.; Levkovitch-Verbin, H.; Gal, G.; Fennig, S.; Treves, I.; Kron, S. (2010). "A Double-Blind, Randomized Study of Minocycline for the Treatment of Negative and Cognitive Symptoms in Early-Phase Schizophrenia". The Journal of Clinical Psychiatry. 71 (2): 138–149. doi:10.4088/JCP.08m04666yel. PMID 19895780.
- Irving, CB; Mumby-Croft, R; Joy, LA (July 2006). "Polyunsaturated fatty acid supplementation for schizophrenia(Review)". Cochrane Database of Systematic Reviews (3): CD001257. doi:10.1002/14651858.CD001257.pub2. PMC 7032618. PMID 16855961.
- Ritsner, M. S.; Gibel, A.; Shleifer, T.; Boguslavsky, I.; Zayed, A.; Maayan, R.; Weizman, A.; Lerner, V. (2010). "Pregnenolone and Dehydroepiandrosterone as an Adjunctive Treatment in Schizophrenia and Schizoaffective Disorder". The Journal of Clinical Psychiatry. 71 (10): 1351–1362. doi:10.4088/JCP.09m05031yel. PMID 20584515.
- Marx, C. E.; Keefe, R. S. E.; Buchanan, R. W.; Hamer, R. M.; Kilts, J. D.; Bradford, D. W.; Strauss, J. L.; Naylor, J. C.; Payne, V. M.; Lieberman, J. A.; Savitz, A. J.; Leimone, L. A.; Dunn, L.; Porcu, P.; Morrow, A. L.; Shampine, L. J. (2009). "Proof-of-Concept Trial with the Neurosteroid Pregnenolone Targeting Cognitive and Negative Symptoms in Schizophrenia". Neuropsychopharmacology. 34 (8): 1885–1903. doi:10.1038/npp.2009.26. PMC 3427920. PMID 19339966.
- Wong, P.; Chang, C. C. R.; Marx, C. E.; Caron, M. G.; Wetsel, W. C.; Zhang, X. (2012). Hashimoto, Kenji (ed.). "Pregnenolone Rescues Schizophrenia-Like Behavior in Dopamine Transporter Knockout Mice". PLOS ONE. 7 (12): e51455. Bibcode:2012PLoSO...751455W. doi:10.1371/journal.pone.0051455. PMC 3519851. PMID 23240026.
- Marx, C. E.; Stevens, R. D.; Shampine, L. J.; Uzunova, V.; Trost, W. T.; Butterfield, M. I.; Massing, M. W.; Hamer, R. M.; Morrow, A. L.; Lieberman, J. A. (2005). "Neuroactive Steroids are Altered in Schizophrenia and Bipolar Disorder: Relevance to Pathophysiology and Therapeutics". Neuropsychopharmacology. 31 (6): 1249–63. doi:10.1038/sj.npp.1300952. PMID 16319920.
- Javitt, D. C.; Zukin, S. R.; Heresco-Levy, U.; Umbricht, D. (2012). "Has an Angel Shown the Way? Etiological and Therapeutic Implications of the PCP/NMDA Model of Schizophrenia". Schizophrenia Bulletin. 38 (5): 958–966. doi:10.1093/schbul/sbs069. PMC 3446214. PMID 22987851.
- Hatano, T.; Ohnuma, T.; Sakai, Y.; Shibata, N.; Maeshima, H.; Hanzawa, R.; Suzuki, T.; Arai, H. (2010). "Plasma alanine levels increase in patients with schizophrenia as their clinical symptoms improve—Results from the Juntendo University Schizophrenia Projects (JUSP)". Psychiatry Research. 177 (1–2): 27–31. doi:10.1016/j.psychres.2010.02.014. PMID 20226539.
- Tsai, G. E.; Yang, P.; Chang, Y. C.; Chong, M. Y. (2006). "D-Alanine Added to Antipsychotics for the Treatment of Schizophrenia". Biological Psychiatry. 59 (3): 230–234. doi:10.1016/j.biopsych.2005.06.032. PMID 16154544.
- d'Souza, D. C.; Radhakrishnan, R.; Perry, E.; Bhakta, S.; Singh, N. M.; Yadav, R.; Abi-Saab, D.; Pittman, B.; Chaturvedi, S. K.; Sharma, M. P.; Bell, M.; Andrade, C. (2012). "Feasibility, Safety, and Efficacy of the Combination of D-Serine and Computerized Cognitive Retraining in Schizophrenia: An International Collaborative Pilot Study". Neuropsychopharmacology. 38 (3): 492–503. doi:10.1038/npp.2012.208. PMC 3547200. PMID 23093223.
- Heresco-Levy, U.; Javitt, D. C.; Ebstein, R.; Vass, A.; Lichtenberg, P.; Bar, G.; Catinari, S.; Ermilov, M. (2005). "D-serine efficacy as add-on pharmacotherapy to risperidone and olanzapine for treatment-refractory schizophrenia". Biological Psychiatry. 57 (6): 577–585. doi:10.1016/j.biopsych.2004.12.037. PMID 15780844.
- Lane, H. Y.; Chang, Y. C.; Liu, Y. C.; Chiu, C. C.; Tsai, G. E. (2005). "Sarcosine or D-Serine Add-on Treatment for Acute Exacerbation of Schizophrenia". Archives of General Psychiatry. 62 (11): 1196–1204. doi:10.1001/archpsyc.62.11.1196. PMID 16275807.
- Lane, H. Y.; Lin, C. H.; Huang, Y. J.; Liao, C. H.; Chang, Y. C.; Tsai, G. E. (2009). "A randomized, double-blind, placebo-controlled comparison study of sarcosine ( N-methylglycine) and d-serine add-on treatment for schizophrenia". The International Journal of Neuropsychopharmacology. 13 (4): 451–460. doi:10.1017/S1461145709990939. PMID 19887019.
- Tsai, G. E.; Yang, P.; Chung, L. C.; Tsai, I. C.; Tsai, C. W.; Coyle, J. T. (1999). "D-serine added to clozapine for the treatment of schizophrenia". The American Journal of Psychiatry. 156 (11): 1822–1825. doi:10.1176/ajp.156.11.1822 (inactive 2020-03-11). PMID 10553752.
- Weiser, M.; Heresco-Levy, U.; Davidson, M.; Javitt, D. C.; Werbeloff, N.; Gershon, A. A.; Abramovich, Y.; Amital, D.; Doron, A.; Konas, S.; Levkovitz, Y.; Liba, D.; Teitelbaum, A.; Mashiach, M.; Zimmerman, Y. (2012). "A Multicenter, Add-On Randomized Controlled Trial of Low-Dosed-Serine for Negative and Cognitive Symptoms of Schizophrenia". The Journal of Clinical Psychiatry. 73 (6): e728–34. doi:10.4088/JCP.11m07031. PMID 22795211.
- Dean, O.; Giorlando, F.; Berk, M. (2011). "N-acetylcysteine in psychiatry: Current therapeutic evidence and potential mechanisms of action". Journal of Psychiatry & Neuroscience. 36 (2): 78–86. doi:10.1503/jpn.100057. PMC 3044191. PMID 21118657.
- Aoyama, K.; Watabe, M.; Nakaki, T. (2008). "Regulation of Neuronal Glutathione Synthesis". Journal of Pharmacological Sciences. 108 (3): 227–238. doi:10.1254/jphs.08R01CR. PMID 19008644.
- Jain, A.; Mårtensson, J.; Stole, E.; Auld, P. A.; Meister, A. (1991). "Glutathione deficiency leads to mitochondrial damage in brain". Proceedings of the National Academy of Sciences of the United States of America. 88 (5): 1913–1917. Bibcode:1991PNAS...88.1913J. doi:10.1073/pnas.88.5.1913. PMC 51136. PMID 2000395.
- Berk, M.; Copolov, D.; Dean, O.; Lu, K.; Jeavons, S.; Schapkaitz, I.; Anderson-Hunt, M.; Judd, F.; Katz, F.; Katz, P.; Ording-Jespersen, S.; Little, J.; Conus, P.; Cuenod, M.; Do, K. Q.; Bush, A. I. (2008). "N-Acetyl Cysteine as a Glutathione Precursor for Schizophrenia—A Double-Blind, Randomized, Placebo-Controlled Trial". Biological Psychiatry. 64 (5): 361–368. doi:10.1016/j.biopsych.2008.03.004. PMID 18436195.
- Berk, M.; Munib, A.; Dean, O.; Malhi, G. S.; Kohlmann, K.; Schapkaitz, I.; Jeavons, S.; Katz, F.; Anderson-Hunt, M.; Conus, P.; Hanna, B.; Otmar, R. E.; Ng, F.; Copolov, D. L.; Bush, A. I. (2011). "Qualitative Methods in Early-Phase Drug Trials". The Journal of Clinical Psychiatry. 72 (7): 909–913. doi:10.4088/JCP.09m05741yel. PMID 20868637.
- Carmeli, C.; Knyazeva, M. G.; Cuénod, M.; Do, K. Q. (2012). Burne, Thomas (ed.). "Glutathione Precursor N-Acetyl-Cysteine Modulates EEG Synchronization in Schizophrenia Patients: A Double-Blind, Randomized, Placebo-Controlled Trial". PLOS ONE. 7 (2): e29341. Bibcode:2012PLoSO...729341C. doi:10.1371/journal.pone.0029341. PMC 3285150. PMID 22383949.
- Lavoie, S.; Murray, M. M.; Deppen, P.; Knyazeva, M. G.; Berk, M.; Boulat, O.; Bovet, P.; Bush, A. I.; Conus, P.; Copolov, D.; Fornari, E.; Meuli, R.; Solida, A.; Vianin, P.; Cuénod, M.; Buclin, T.; Do, K. Q. (2007). "Glutathione Precursor, N-Acetyl-Cysteine, Improves Mismatch Negativity in Schizophrenia Patients". Neuropsychopharmacology. 33 (9): 2187–2199. doi:10.1038/sj.npp.1301624. PMID 18004285.
- Lane, H. Y.; Huang, C. L.; Wu, P. L.; Liu, Y. C.; Chang, Y. C.; Lin, P. Y.; Chen, P. W.; Tsai, G. (2006). "Glycine Transporter I Inhibitor, N-methylglycine (Sarcosine), Added to Clozapine for the Treatment of Schizophrenia". Biological Psychiatry. 60 (6): 645–649. doi:10.1016/j.biopsych.2006.04.005. PMID 16780811.
- Lane, H. Y.; Liu, Y. C.; Huang, C. L.; Chang, Y. C.; Liau, C. H.; Perng, C. H.; Tsai, G. E. (2008). "Sarcosine (N-Methylglycine) Treatment for Acute Schizophrenia: A Randomized, Double-Blind Study". Biological Psychiatry. 63 (1): 9–12. doi:10.1016/j.biopsych.2007.04.038. PMID 17659263.
- Tsai, G.; Lane, H. Y.; Yang, P.; Chong, M. Y.; Lange, N. (2004). "Glycine transporter I inhibitor, N-Methylglycine (sarcosine), added to antipsychotics for the treatment of schizophrenia". Biological Psychiatry. 55 (5): 452–456. doi:10.1016/j.biopsych.2003.09.012. PMID 15023571.
- Singh, J; Kour, K; Jayaram, MB (January 2012). "Acetylcholinesterase inhibitors for schizophrenia". Cochrane Database of Systematic Reviews. 1: CD007967. doi:10.1002/14651858.CD007967.pub2. PMC 6823258. PMID 22258978.
- Choi, KH; Wykes, T; Kurtz, MM (September 2013). "Adjunctive pharmacotherapy for cognitive deficits in schizophrenia: meta-analytical investigation of efficacy". The British Journal of Psychiatry. 203 (3): 172–178. doi:10.1192/bjp.bp.111.107359. PMC 3759029. PMID 23999481.
- Ribeiz, SR; Bassitt, DP; Arrais, JA; Avila, R; Steffens, DC; Bottino, CM (April 2010). "Cholinesterase Inhibitors as Adjunctive Therapy in Patients with Schizophrenia and Schizoaffective Disorder A Review and Meta-Analysis of the Literature". CNS Drugs. 24 (4): 303–317. doi:10.2165/11530260-000000000-00000. PMID 20297855.
- Koike, K; Hashimoto, K; Takai, N; Shimizu, E; Komatsu, N; Watanabe, H; Nakazato, M; Okamura, N; Stevens, KE; Freedman, R; Iyo, M (July 2005). "Tropisetron improves deficits in auditory P50 suppression in schizophrenia". Schizophrenia Research. 76 (1): 67–72. doi:10.1016/j.schres.2004.12.016. PMID 15927799.
- Shiina, A; Shirayama, Y; Niitsu, T; Hashimoto, T; Yoshida, T; Hasegawa, T; Haraguchi, T; Kanahara, N; Shiraishi, T; Fujisaki, M; Fukami, G; Nakazato, M; Iyo, M; Hashimoto, K (June 2010). "A randomised, double-blind, placebo-controlled trial of tropisetron in patients with schizophrenia". Annals of General Psychiatry. 9 (1): 27. doi:10.1186/1744-859X-9-27. PMC 2901366. PMID 20573264.
- Zhang, XY; Liu, L; Liu, S; Hong, X; Chen da, C; Xiu, MH; Yang, FD; Zhang, Z; Zhang, X; Kosten, TA; Kosten, TR (September 2012). "Short-Term Tropisetron Treatment and Cognitive and P50 Auditory Gating Deficits in Schizophrenia". The American Journal of Psychiatry. 169 (9): 974–981. doi:10.1176/appi.ajp.2012.11081289. PMID 22952075.
- Noroozian, M; Ghasemi, S; Hosseini, SM; Modabbernia, A; Khodaie-Ardakani, MR; Mirshafiee, O; Farokhnia, M; Tajdini, M; Rezaei, F; Salehi, B; Ashrafi, M; Yekehtaz, H; Tabrizi, M; Akhondzadeh, S (Aug 2013). "A placebo-controlled study of tropisetron added to risperidone for the treatment of negative symptoms in chronic and stable schizophrenia". Psychopharmacology. 228 (4): 595–602. doi:10.1007/s00213-013-3064-2. PMID 23515583.
- Singh, SP; Singh, V; Kar, N; Chan, K (September 2010). "Efficacy of antidepressants in treating the negative symptoms of chronic schizophrenia: meta-analysis". The British Journal of Psychiatry. 197 (3): 174–179. doi:10.1192/bjp.bp.109.067710. PMID 20807960.
- Iancu, I; Tschernihovsky, E; Bodner, E; Piconne, AS; Lowengrub, K (August 2010). "Escitalopram in the treatment of negative symptoms in patients with chronic schizophrenia: a randomized double-blind placebo-controlled trial". Psychiatry Research. 179 (1): 19–23. doi:10.1016/j.psychres.2010.04.035. PMID 20472299.
- White, N; Litovitz, T; Clancy, C (December 2008). "Suicidal antidepressant overdoses: a comparative analysis by antidepressant type". Journal of Medical Toxicology. 4 (4): 238–250. doi:10.1007/BF03161207. PMC 3550116. PMID 19031375.
- Hecht, EM; Landy, DC (February 2012). "Alpha-2 receptor antagonist add-on therapy in the treatment of schizophrenia; a meta-analysis". Schizophrenia Research. 134 (2–3): 202–206. doi:10.1016/j.schres.2011.11.030. PMID 22169246.
- Rossi, S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- Joint Formulary Committee (2013). British National Formulary (BNF) (65 ed.). London, UK: Pharmaceutical Press. p. 247. ISBN 978-0-85711-084-8.
- Ritsner, MS (2013). Ritsner, Michael S (ed.). Polypharmacy in Psychiatry Practice, Volume I. Springer Science+Business Media Dordrecht. doi:10.1007/978-94-007-5805-6. ISBN 9789400758056.
- Vidal, C; Reese, C; Fischer, BA; Chiapelli, J; Himelhoch, S (March 2013). "Meta-Analysis of Efficacy of Mirtazapine as an Adjunctive Treatment of Negative Symptoms in Schizophrenia". Clinical Schizophrenia & Related Psychoses. 9 (2): 88–95. doi:10.3371/CSRP.VIRE.030813. ISSN 1935-1232. PMID 23491969.
- Stenberg, JH; Terevnikov, V; Joffe, M; Tiihonen, J; Tchoukhine, E; Burkin, M; Joffe, G (June 2011). "More evidence on proneurocognitive effects of add-on mirtazapine in schizophrenia". Progress in Neuro-Psychopharmacology and Biological Psychiatry. 35 (4): 1080–1086. doi:10.1016/j.pnpbp.2011.03.004. PMID 21402120.
- Kumar, R; Sachdev, PS (May 2009). "Akathisia and Second-generation Antipsychotic Drugs". Current Opinion in Psychiatry. 22 (3): 293–299. doi:10.1097/YCO.0b013e32832a16da. PMID 19378382.
- Koh, E. H.; Lee, W. J.; Lee, S. A.; Kim, E. H.; Cho, E. H.; Jeong, E.; Kim, D. W.; Kim, M. S.; Park, J. Y.; Park, K. G.; Lee, H. J.; Lee, I. K.; Lim, S.; Jang, H. C.; Lee, K. H.; Lee, K. U. (2011). "Effects of Alpha-Lipoic Acid on Body Weight in Obese Subjects". The American Journal of Medicine. 124 (1): 85.e1–85.e8. doi:10.1016/j.amjmed.2010.08.005. PMID 21187189.
- Kim, E.; Park, D. W.; Choi, S. H.; Kim, J. J.; Cho, H. S. (2008). "A Preliminary Investigation of α-Lipoic Acid Treatment of Antipsychotic Drug-Induced Weight Gain in Patients with Schizophrenia". Journal of Clinical Psychopharmacology. 28 (2): 138–146. doi:10.1097/JCP.0b013e31816777f7. PMID 18344723.
- Jariwalla, R. J.; Lalezari, J.; Cenko, D.; Mansour, S. E.; Kumar, A.; Gangapurkar, B.; Nakamura, D. (2008). "Restoration of Blood Total Glutathione Status and Lymphocyte Function Followingα-Lipoic Acid Supplementation in Patients with HIV Infection". The Journal of Alternative and Complementary Medicine. 14 (2): 139–146. doi:10.1089/acm.2006.6397. PMID 18315507.
- Ritsner, M. S.; Miodownik, C.; Ratner, Y.; Shleifer, T.; Mar, M.; Pintov, L.; Lerner, V. (2011). "L-Theanine Relieves Positive, Activation, and Anxiety Symptoms in Patients with Schizophrenia and Schizoaffective Disorder". The Journal of Clinical Psychiatry. 72 (1): 34–42. doi:10.4088/JCP.09m05324gre. PMID 21208586.
- Miodownik, C.; Maayan, R.; Ratner, Y.; Lerner, V.; Pintov, L.; Mar, M.; Weizman, A.; Ritsner, M. S. (2011). "Serum Levels of Brain-Derived Neurotrophic Factor and Cortisol to Sulfate of Dehydroepiandrosterone Molar Ratio Associated with Clinical Response to l-Theanine as Augmentation of Antipsychotic Therapy in Schizophrenia and Schizoaffective Disorder Patients". Clinical Neuropharmacology. 34 (4): 155–160. doi:10.1097/WNF.0b013e318220d8c6. PMID 21617527.
- Lardner, A. L. (2013). "Neurobiological effects of the green tea constituent theanine and its potential role in the treatment of psychiatric and neurodegenerative disorders". Nutritional Neuroscience. 17 (4): 145–155. doi:10.1179/1476830513Y.0000000079. PMID 23883567.
- Kelly, S. P.; Gomez-Ramirez, M.; Montesi, J. L.; Foxe, J. J. (2008). "L-theanine and caffeine in combination affect human cognition as evidenced by oscillatory alpha-band activity and attention task performance". The Journal of Nutrition. 138 (8): 1572S–1577S. doi:10.1093/jn/138.8.1572S. PMID 18641209.
- Park, S. K.; Jung, I. C.; Lee, W. K.; Lee, Y. S.; Park, H. K.; Go, H. J.; Kim, K.; Lim, N. K.; Hong, J. T.; Ly, S. Y.; Rho, S. S. (2011). "A Combination of Green Tea Extract andl-Theanine Improves Memory and Attention in Subjects with Mild Cognitive Impairment: A Double-Blind Placebo-Controlled Study". Journal of Medicinal Food. 14 (4): 334–343. doi:10.1089/jmf.2009.1374. PMID 21303262.
- Foxe, J. J.; Morie, K. P.; Laud, P. J.; Rowson, M. J.; De Bruin, E. A.; Kelly, S. P. (2012). "Assessing the effects of caffeine and theanine on the maintenance of vigilance during a sustained attention task". Neuropharmacology. 62 (7): 2320–2327. doi:10.1016/j.neuropharm.2012.01.020. PMID 22326943.
- Nobre, A. C.; Rao, A.; Owen, G. N. (2008). "L-theanine, a natural constituent in tea, and its effect on mental state". Asia Pacific Journal of Clinical Nutrition. 17 Suppl 1: 167–168. PMID 18296328.
- Di, X.; Yan, J.; Zhao, Y.; Chang, Y.; Zhao, B. (2012). "L-theanine inhibits nicotine-induced dependence via regulation of the nicotine acetylcholine receptor-dopamine reward pathway". Science China Life Sciences. 55 (12): 1064–1074. doi:10.1007/s11427-012-4401-0. PMID 23233221.
- Meskanen, K; Ekelund, H; Laitinenm, J; Neuvonen, PJ; Haukka, J; Panula P; Ekelund, J (August 2013). "A randomized clinical trial of histamine 2 receptor antagonism in treatment-resistant schizophrenia". Journal of Clinical Psychopharmacology. 33 (4): 472–478. doi:10.1097/JCP.0b013e3182970490. PMID 23764683.
- Atmaca, M.; Tezcan, E.; Kuloglu, M.; Ustundag, B.; Kirtas, O. (2005). "The effect of extract of ginkgo biloba addition to olanzapine on therapeutic effect and antioxidant enzyme levels in patients with schizophrenia". Psychiatry and Clinical Neurosciences. 59 (6): 652–656. doi:10.1111/j.1440-1819.2005.01432.x. PMID 16401239.
- Doruk, A.; Uzun, Ö.; Ozşahin, A. (2008). "A placebo-controlled study of extract of ginkgo biloba added to clozapine in patients with treatment-resistant schizophrenia". International Clinical Psychopharmacology. 23 (4): 223–227. doi:10.1097/YIC.0b013e3282fcff2f. PMID 18545061.
- Zhang, X. Y.; Zhou, D. F.; Su, J. M.; Zhang, P. Y. (2001). "The effect of extract of ginkgo biloba added to haloperidol on superoxide dismutase in inpatients with chronic schizophrenia". Journal of Clinical Psychopharmacology. 21 (1): 85–88. doi:10.1097/00004714-200102000-00015. PMID 11199954.
- Zhang, X. Y.; Zhou, D. F.; Zhang, P. Y.; Wu, G. Y.; Su, J. M.; Cao, L. Y. (2001). "A double-blind, placebo-controlled trial of extract of Ginkgo biloba added to haloperidol in treatment-resistant patients with schizophrenia". The Journal of Clinical Psychiatry. 62 (11): 878–883. doi:10.4088/JCP.v62n1107. PMID 11775047.
- Zhang, X. Y.; Zhou, D. F.; Cao, L. Y.; Wu, G. Y. (2006). "The effects of Ginkgo biloba extract added to haloperidol on peripheral T cell subsets in drug-free schizophrenia: A double-blind, placebo-controlled trial". Psychopharmacology. 188 (1): 12–17. doi:10.1007/s00213-006-0476-2. PMID 16906395.
- Zhang, W. F.; Tan, Y. L.; Zhang, X. Y.; Chan, R. C. K.; Wu, H. R.; Zhou, D. F. (2011). "Extract ofGinkgo bilobaTreatment for Tardive Dyskinesia in Schizophrenia". The Journal of Clinical Psychiatry. 72 (5): 615–621. doi:10.4088/JCP.09m05125yel. PMID 20868638.
- Zhou, D.; Zhang, X.; Su, J.; Nan, Z.; Cui, Y.; Liu, J.; Guan, Z.; Zhang, P.; Shen, Y. (1999). "The effects of classic antipsychotic haloperidol plus the extract of ginkgo biloba on superoxide dismutase in patients with chronic refractory schizophrenia". Chinese Medical Journal. 112 (12): 1093–1096. PMID 11721446.
- Bennett, AC; Vila, TM (July–August 2010). "The role of ondansetron in the treatment of schizophrenia". Annals of Pharmacotherapy. 44 (7–8): 1301–1306. doi:10.1345/aph.1P008. PMID 20516364.
- Strous, R. D.; Ritsner, M. S.; Adler, S.; Ratner, Y.; Maayan, R.; Kotler, M.; Lachman, H.; Weizman, A. (2009). "SAM-e has mixed evidence as an adjunct. In one study improvement of aggressive behavior and quality of life following S-Adenosyl-Methionine (SAM-e) augmentation in schizophrenia". European Neuropsychopharmacology. 19 (1): 14–22. doi:10.1016/j.euroneuro.2008.08.004. PMID 18824331.
- Guidotti A, Ruzicka W, Grayson DR, Veldic M, Pinna G, Davis JM, Costa E (Jan 2007). "S-adenosyl methionine and DNA methyltransferase-1 mRNA overexpression in psychosis". NeuroReport. 18 (1): 57–60. doi:10.1097/WNR.0b013e32800fefd7. PMID 17259861.
- Dakhale, G. N.; Khanzode, S. D.; Khanzode, S. S.; Saoji, A. (2005). "Supplementation of vitamin C with atypical antipsychotics reduces oxidative stress and improves the outcome of schizophrenia". Psychopharmacology. 182 (4): 494–498. doi:10.1007/s00213-005-0117-1. PMID 16133138.
- Wang, Y.; Liu, X. J.; Robitaille, L.; Eintracht, S.; MacNamara, E.; Hoffer, L. J. (2013). "Effects of vitamin C and vitamin D administration on mood and distress in acutely hospitalized patients". American Journal of Clinical Nutrition. 98 (3): 705–711. doi:10.3945/ajcn.112.056366. PMID 23885048.
- Zhang, M.; Robitaille, L.; Eintracht, S.; Hoffer, L. J. (2011). "Vitamin C provision improves mood in acutely hospitalized patients". Nutrition. 27 (5): 530–533. doi:10.1016/j.nut.2010.05.016. PMID 20688474.
- Kennedy, D. O.; Veasey, R.; Watson, A.; Dodd, F.; Jones, E.; Maggini, S.; Haskell, C. F. (2010). "Effects of high-dose B vitamin complex with vitamin C and minerals on subjective mood and performance in healthy males". Psychopharmacology. 211 (1): 55–68. doi:10.1007/s00213-010-1870-3. PMC 2885294. PMID 20454891.
- Moran M (18 November 2005). "Psychosocial Treatment Often Missing From Schizophrenia Regimens". Psychiatric News. 40 (22): 24–37. doi:10.1176/pn.40.22.0024b. Retrieved 2007-05-17.
- Jones, C.; Cormac, I.; Silveira da Mota Neto, J. I.; Campbell, C. (2004-10-18). Jones, Christopher (ed.). "Cognitive behaviour therapy for schizophrenia". The Cochrane Database of Systematic Reviews (4): CD000524. doi:10.1002/14651858.CD000524.pub2. ISSN 1469-493X. PMID 15495000. (Retracted, see doi:10.1002/14651858.cd000524.pub3. If this is an intentional citation to a retracted paper, please replace
{{Retracted}}with{{Retracted|intentional=yes}}.) - Wykes T, Steel C, Everitt B, Tarrier N (May 2008). "Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor". Schizophrenia Bulletin. 34 (3): 523–37. doi:10.1093/schbul/sbm114. PMC 2632426. PMID 17962231.
- Zimmermann G, Favrod J, Trieu VH, Pomini V (September 2005). "The effect of cognitive behavioral treatment on the positive symptoms of schizophrenia spectrum disorders: a meta-analysis". Schizophrenia Research. 77 (1): 1–9. doi:10.1016/j.schres.2005.02.018. PMID 16005380.
- Lynch D.; Laws K. R.; McKenna P. J. (2010). "Cognitive behavioural therapy for major psychiatric disorder: does it really work? A meta-analytical review of well-controlled trials". Psychological Medicine. 40 (1): 9–24. doi:10.1017/s003329170900590x. PMID 19476688.
- Newton‐Howes, Giles and Rebecca Wood. "Cognitive behavioural therapy and the psychopathology of schizophrenia: Systematic review and meta‐analysis." Psychology and Psychotherapy: Theory, Research and Practice (2011).
- Jones Christopher; et al. (2011). "Cognitive behaviour therapy versus other psychosocial treatments for schizophrenia". The Cochrane Library (4): CD000524. doi:10.1002/14651858.cd000524.pub3. PMID 21491377.
- Wykes T, Brammer M, Mellers J, et al. (2002). "Effects on the brain of a psychological treatment: cognitive remediation therapy: functional magnetic resonance imaging in schizophrenia". British Journal of Psychiatry. 181: 144–52. doi:10.1192/bjp.181.2.144. PMID 12151286.
- Moritz S, Woodward TS (2007). "Metacognitive training in schizophrenia: from basic research to knowledge translation and intervention". Current Opinion in Psychiatry. 20 (6): 619–625. doi:10.1097/YCO.0b013e3282f0b8ed. PMID 17921766.
- Moritz S, Woodward TS, Burlon M (2005). "Metacognitive skill training for patients with schizophrenia (MCT)" (PDF). Hamburg: VanHam Campus. Retrieved 1 April 2011. Cite journal requires
|journal=(help) - Bell V, Halligan PW, Ellis HD (2006). "Explaining delusions: a cognitive perspective". Trends in Cognitive Sciences. 10 (5): 219–226. doi:10.1016/j.tics.2006.03.004. PMID 16600666.
- Moritz S, Woodward TS (2007). "Metacognitive training for schizophrenia patients (MCT): A pilot study on feasibility, treatment adherence, and subjective efficacy" (PDF). German Journal of Psychiatry. 10: 69–78. Archived from the original (PDF) on 2016-03-05. Retrieved 2011-04-01.
- Aghotor J, Pfueller U, Moritz S, Weisbrod M, Roesch-Ely D (September 2010). "Metacognitive training for patients with schizophrenia (MCT): feasibility and preliminary evidence for its efficacy". Journal of Behavior Therapy and Experimental Psychiatry. 41 (3): 207–11. doi:10.1016/j.jbtep.2010.01.004. PMID 20167306.
- Ross K, Freeman D, Dunn G, Garety P (March 2011). "A randomized experimental investigation of reasoning training for people with delusions". Schizophrenia Bulletin. 37 (2): 324–33. doi:10.1093/schbul/sbn165. PMC 3044626. PMID 19520745.
- Moritz S, Veckenstedt R, Randjbar S, Vitzthum F (in press). "Individualized metacognitive therapy for people with schizophrenia psychosis (MCT+)", Springer, Heidelberg.
- McFarlane WR, Dixon L, Lukens E, Lucksted A (April 2003). "Family psychoeducation and schizophrenia: a review of the literature". Journal of Marital and Family Therapy. 29 (2): 223–45. doi:10.1111/j.1752-0606.2003.tb01202.x. PMID 12728780.
- Glynn SM, Cohen AN, Niv N (January 2007). "New challenges in family interventions for schizophrenia". Expert Review of Neurotherapeutics. 7 (1): 33–43. doi:10.1586/14737175.7.1.33. PMID 17187495.
- Pharoah, Fiona; Mari, Jair; Rathbone, John; Wong, Winson (2010-12-08). Pharoah, Fiona (ed.). "Family intervention for schizophrenia". The Cochrane Database of Systematic Reviews (12): CD000088. doi:10.1002/14651858.CD000088.pub2. ISSN 1469-493X. PMC 4204509. PMID 21154340.
- Jones, S., Hayward, P. (2004). Coping with Schizophrenia: A Guide for Patients, Families and Caregivers. Oxford, England: Oneworld Pub. ISBN 978-1-85168-344-4.CS1 maint: multiple names: authors list (link)
- Torrey, EF (2006). Surviving Schizophrenia: A Manual for Families, Consumers, and Providers (5th Edition). HarperCollins. ISBN 978-0-06-084259-8.
- Kopelowicz A, Liberman RP, Zarate R (Oct 2006). "Recent advances in social skills training for schizophrenia". Schizophrenia Bulletin. 32 (Suppl 1): S12–23. doi:10.1093/schbul/sbl023. PMC 2632540. PMID 16885207.
- American Psychiatric Association (2004) Practice Guideline for the Treatment of Patients With Schizophrenia. Second Edition.
- Talwar N, Crawford MJ, Maratos A, Nur U, McDermott O, Procter S (November 2006). "Music therapy for in-patients with schizophrenia: Exploratory randomised controlled trial". The British Journal of Psychiatry. 189 (5): 405–9. doi:10.1192/bjp.bp.105.015073. PMID 17077429.
- Ruddy R, Milnes D (2005). Ruddy R (ed.). "Art therapy for schizophrenia or schizophrenia-like illnesses". Cochrane Database of Systematic Reviews (4): CD003728. doi:10.1002/14651858.CD003728.pub2. PMID 16235338.
- Ruddy RA, Dent-Brown K (2007). Ruddy R (ed.). "Drama therapy for schizophrenia or schizophrenia-like illnesses". Cochrane Database of Systematic Reviews (1): CD005378. doi:10.1002/14651858.CD005378.pub2. PMID 17253555.
- Mosher LR. Soteria and other alternatives to acute psychiatric hospitalization: a personal and professional review. Journal of Nervous and Mental Disease. 1999;187(3):142–9. doi:10.1097/00005053-199903000-00003. PMID 10086470.
- Calton T, Ferriter M, Huband N, Spandler H. A systematic review of the Soteria paradigm for the treatment of people diagnosed with schizophrenia. Schizophrenia Bulletin. 2008 [Retrieved 2008-07-03];34(1):181–92. doi:10.1093/schbul/sbm047. PMID 17573357. PMC 2632384.
- Bartholomeusz, Call (2011). Handbook of Schizophrenia Spectrum Disorders, Volume III: Therapeutic Approaches, Comorbidity, and Outcomes. Springer. p. 189. ISBN 9789400708341.
- Ng QX, Soh AY, Venkatanarayanan N, et al. (2019). "A Systematic Review of the Effect of Probiotic Supplementation on Schizophrenia Symptoms". Neuropsychobiology. 78 (1): 1–6. doi:10.1159/000498862. PMID 30947230.
- Patrick RP, Ames BN (June 2015). "Vitamin D and the omega-3 fatty acids control serotonin synthesis and action, part 2: relevance for ADHD, bipolar disorder, schizophrenia, and impulsive behavior". FASEB Journal. 29 (6): 2207–22. doi:10.1096/fj.14-268342. PMID 25713056.
- Lim SY (July 2016). "Nutritional Factors Affecting Mental Health". Clinical Nutrition Research. 5 (3): 143–52. doi:10.7762/cnr.2016.5.3.143. PMC 4967717. PMID 27482518.
- Bosnjak Kuharic D, Kekin I, Hew J, Rojnic Kuzman M, Puljak L (1 November 2019). "Interventions for prodromal stage of psychosis". The Cochrane Database of Systematic Reviews. 2019 (11). doi:10.1002/14651858.CD012236.pub2. PMC 6823626. PMID 31689359.
- Shen X, Xia J, Adams CE (20 October 2014). "Acupuncture for schizophrenia". The Cochrane Database of Systematic Reviews (10): CD005475. doi:10.1002/14651858.CD005475.pub2. PMC 4193731. PMID 25330045.
- van den Noort M, Yeo S, Lim S, et al. (30 March 2018). "Acupuncture as Add-On Treatment of the Positive, Negative, and Cognitive Symptoms of Patients with Schizophrenia: A Systematic Review". Medicines. 5 (2): 29. doi:10.3390/medicines5020029. PMC 6023351. PMID 29601477.
- Deng H, Xu J (28 June 2017). "Wendan decoction (Traditional Chinese medicine) for schizophrenia". The Cochrane Database of Systematic Reviews. 6: CD012217. doi:10.1002/14651858.CD012217.pub2. PMC 6481906. PMID 28657646.
- Wieland LS, Santesso N (October 2017). "Summary of a Cochrane review: Wendan decoction traditional Chinese medicine for schizophrenia". European Journal of Integrative Medicine. 15: 81–82. doi:10.1016/j.eujim.2017.09.009. PMC 5649251. PMID 29062436.
- Pinault, D (28 March 2017). "A Neurophysiological Perspective on a Preventive Treatment against Schizophrenia Using Transcranial Electric Stimulation of the Corticothalamic Pathway". Brain Sciences. 7 (4): 34. doi:10.3390/brainsci7040034. PMC 5406691. PMID 28350371.
- Nathou C, Etard O, Dollfus S (2019). "Auditory verbal hallucinations in schizophrenia: current perspectives in brain stimulation treatments". Neuropsychiatric Disease and Treatment. 15: 2105–2117. doi:10.2147/NDT.S168801. PMC 6662171. PMID 31413576.
- Greenhalgh J, Knight C, Hind D, Beverley C, Walters S (March 2005). "Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modeling studies". Health Technology Assessment. 9 (9): 1–156. doi:10.3310/hta9090. PMID 15774232.
- National Institute for Health and Clinical Excellence (April 2003). "The clinical effectiveness and cost effectiveness of electroconvulsive Therapy (ECT) for depressive illness, schizophrenia, catatonia and mania". National Institute for Health and Clinical Excellence. Retrieved 2007-06-17.
- Mashour GA, Walker EE, Martuza RL (2005). "Psychosurgery: past, present, and future". Brain Research. Brain Research Reviews. 48 (3): 409–19. doi:10.1016/j.brainresrev.2004.09.002. PMID 15914249.
- Laupu, Wendy Kay (2014). The efficacy of Garcinia mangostana L. (mangosteen) pericarp as an adjunctive to second-generation antipsychotics for the treatment of schizophrenia: a double blind, randomised, placebo-controlled trial (phd). James Cook University. 40097. Retrieved April 24, 2017.
- Laupu, W (September 2016). "Interpreting outcomes from the supplementation of mangosteen rind powder capsules in schizophrenia and schizoaffective disorders". British Journal of Medical and Health Research. 3 (9). Retrieved April 24, 2017.
- Helman DS (2018). "Recovery from schizophrenia: An autoethnography". Deviant Behavior. 39 (3): 380–399. doi:10.1080/01639625.2017.1286174.
- Chien, W.T., Clifton, A.V., Zhao, S. and Lui, S., 2019. Peer support for people with schizophrenia or other serious mental illness. Cochrane Database of Systematic Reviews, (4).