Health geography
Health geography is the application of geographical information, perspectives, and methods to the study of health, disease, and health care.
Overview
The study of health geography has been influenced by repositioning medical geography within the field of social geography due to a shift towards a social model in health care, rather than a medical model. This advocates for the redefinition of health and health care away from prevention and treatment of illness only to one of promoting well-being in general. Under this model, some previous illnesses (e.g., mental ill health) are recognized as behavior disturbances only, and other types of medicine (e.g., complementary or alternative medicine and traditional medicine) are studied by the medicine researchers, sometimes with the aid of health geographers without medical education. This shift changes the definition of care, no longer limiting it to spaces such as hospitals or doctor's offices. Also, the social model gives priority to the intimate encounters performed at non-traditional spaces of medicine and healthcare as well as to the individuals as health consumers.[1]
This alternative methodological approach means that medical geography is broadened to incorporate philosophies such as Marxian political economy, structuralism, social interactionism, humanism, feminism and queer theory.[2]
History
The relationship between space and health dates back to Hippocrates, who stated that "airs, waters, places" all played significant roles impacting human health and history.[2] A classic piece of research in health geography was done in 1854 as a cholera outbreak gripped a neighborhood in London. Death tolls rang around the clock and the people feared that they were being infected by vapors coming from the ground. John Snow predicted that if he could locate the source of the disease, it could be contained. He drew maps demonstrating the homes of people who had died of cholera and the locations of water pumps. He found that one pump, the public pump on Broad Street, was central to most of the victims. He concluded that infected water from the pump was the culprit. He instructed the authorities to remove the handle to the pump, making it unusable. As a result, the number of new cholera cases decreased.
Areas of study
Health geography is considered to be divided into two distinct elements. The first of which is focused on geographies of disease and ill health, involving descriptive research quantifying disease frequencies and distributions, and analytic research concerned with finding what characteristics make an individual or population susceptible to disease. This requires an understanding of epidemiology.[3] The second component of health geography is the geography of health care, primarily facility location, accessibility, and utilization. This requires the use of spatial analysis and often borrows from behavioral economics.[4]
Geographies of disease and ill health
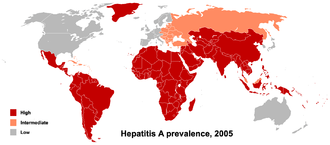
Health geographers are concerned with the prevalence of different diseases along a range of spatial scales from a local to global view, and inspects the natural world, in all of its complexity, for correlations between diseases and locations. This situates health geography alongside other geographical sub-disciplines that trace human-environment relations. Health geographers use modern spatial analysis tools to map the dispersion of various diseases, as individuals spread them amongst themselves, and across wider spaces as they migrate.[2] Health geographers also consider all types of spaces as presenting health risks, from natural disasters, to interpersonal violence, stress, and other potential dangers.[1]
Geography of health care provision
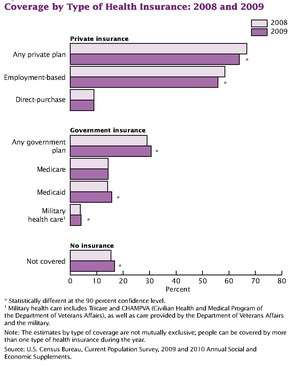
Although healthcare is a public good, it is not equally available to all individuals. Demand for public services is continuously increasing. People need advance knowledge and the latest prediction technology, that health geography offers. The latest example of such technology is Telemedicine. Many people in the United States are not able to access proper healthcare because of inequality in health insurance and the means to afford medical care.[5]
Mobility and Disease Tracking:
With the advent of mobile technology and its spread, it is now possible to track individual mobility. By correlating the movement of individuals through tracking the devices using access towers or other tracking systems, it is now possible to determine and even control disease spread. While privacy laws question the legality of tracking individuals, the commercial mobile service providers are using covert techniques or obtaining government waivers to allow permission to track people.
Health geographers
Notable health geographers include:
- Sarah Curtis
- William C. Gorgas
- Kelvyn Jones
- John Snow
See also
- Cluster (epidemiology)
- Social model of disability
- Spatial epidemiology
References
- Philo, Chris (2009). "Health and Health Care". In Gregory, Derek; Johnston, Ron; Pratt, Geraldine et. al The Dictionary of Human Geography (Fifth Edition). Oxford:Blackwell. pp.325-326
- Philo, Chris (2009). "Medical Geography". In Gregory, Derek; Johnston, Ron; Pratt, Geraldine et. al The Dictionary of Human Geography (Fifth Edition). Oxford:Blackwell. pp.451-453
- Ocaña-Riola, Ricardo (2010). "Common errors in disease mapping". Geospatial Health. 4 (2): 139–54. doi:10.4081/gh.2010.196. PMID 20503184.
- Litva, Andréa (1995). "Coming out: exposing social theory in medical geography". Health. 1 (1): 5–14. doi:10.1016/1353-8292(95)00002-4.
- "The costs of inequality: Money = quality health care = longer life". Harvard Gazette. Retrieved 2017-02-19.
