Granulin
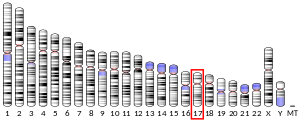
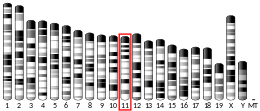
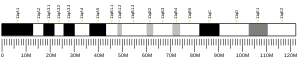
Granulin is a protein that in humans is encoded by the GRN gene.[5][6][7] Each granulin protein is cleaved from the precursor progranulin, a 593 amino acid long and 68.5 kDa protein.[8] While the function of progranulin and granulin have yet to be determined, both forms of the protein have been implicated in development, inflammation, cell proliferation and protein homeostasis. The 2006 discovery of the GRN mutation in a population of patients with frontotemporal dementia has spurred much research in uncovering the function and involvement in disease of progranulin in the body. While there is a growing body of research on progranulin's role in the body, studies on specific granulin residues are still limited.
| Granulin | |||||||||
|---|---|---|---|---|---|---|---|---|---|
 the solution structure of a well-folded peptide based on the 31-residue amino-terminal subdomain of human granulin a | |||||||||
| Identifiers | |||||||||
| Symbol | Granulin | ||||||||
| Pfam | PF00396 | ||||||||
| InterPro | IPR000118 | ||||||||
| PROSITE | PDOC00634 | ||||||||
| SCOPe | 1pcn / SUPFAM | ||||||||
| |||||||||
Progranulin
Progranulin is the precursor protein for granulin. Cleavage of progranulin produces a variety of active 6 kDa granulin peptides. These smaller cleavage products are named granulin A, granulin B, granulin C, etc. Epithelins 1 and 2 are synonymous with granulins A and B, respectively. Cleavage of progranulin into granulin occurs either in the extracellular matrix or the lysosome. Elastase, proteinase 3 and matrix metalloproteinase are proteases capable of cleaving progranulin into individual granulin peptides.[8][9] Progranulin and granulin can be further differentiated by their hypothesized opposing roles in the cell. While progranulin is associated with anti-inflammation, cleaved granulin peptides have been implicated in pro-inflammatory behavior. A C. elegans study showed that granulin peptides may also participate in toxic activity.[9]
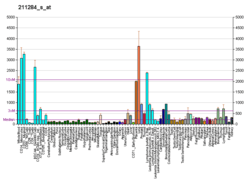
Expression
Progranulin is expressed in a wide variety of cell types both in the periphery and in the central nervous system. Progranulin expression is low in early development, but increases as cells mature.[10] Cell types expressing progranulin include neurons, microglia, astrocytes and endothelial cells.[11] Progranulin has been found to be highly expressed in microglia and up-regulated during injury[11][10] Within the brain, progranulin mRNA is highly expressed in pyramidal, hippocampal and Purkinje cells cells.[8]
Structure
Each individual granulin domain peptide is 60 amino acids in length. Granulin peptides are cysteine rich and capable of forming 6 disulfide bonds per residue.[9] The disulfide bonds form a central rod-like core that shuttles each individual granulin peptide into a stacked β-sheet configuration.[11][8] The structure of the granulin protein is similar to the structure of proteins from protein families that consist of hormones, growth factors, ion channel modulators and enzyme inhibitors.[11] Because of progranulin's structural similarities to these proteins, much research was done to interrogate progranulin's potential role as a growth factor. When progranulin is secreted into the extracellular matrix, it is often glycosylated at 4 confirmed and 1 tentative N-linked glycosylation sites.[11][9] The n-terminus of progranulin is hypothesized to be involved in the secretion of progranulin via secretory vesicles.[11] Specifically, Progranulin may be involved in regulating exosome excretion.[12] The C-terminus of progranulin is hypothesized to be the primary binding partner of SORT1, a receptor of extracellular progranulin.[13][11] The structural differences between each individual granulin peptide have yet to be characterized.
Interactive partners
In the extracellular matrix, progranulin binds to receptors on several cell types resulting in either activation of a signal transduction pathway or engulfment into the cell. Several studies have shown progranulin's involvement in the binding of SORT1 and the subsequent trafficking of bounded progranulin to the lysosome.[11] One recent study has shown that progranulin may actually mediate prosaposin trafficking to the lysosome via SORT1.[14] However, the absence of SORT1 does not prevent exogenous progranulin from promoting neurite outgrowth or enhancing cell survival of GRN knockout cells, suggesting that other receptors are involved in mediating extracellular progranulin function[15] For example, SORT1 -/- neuronal cells are still able to bind progranulin.[15] Other studies have suggested tumor necrosis factor and EPH receptor A2 as potential progranulin facilitators.[11] After binding to the receptor, progranulin may induce and modulate signaling pathways such as MAPK/ERK, PI3K/Akt, and FAK.[9][15] Gene ontology enrichment analysis reveals an association between progranulin and notch receptor signaling.[9] Granulin has also been shown to interact with Cyclin T1[16] and TRIB3.[17]
Function
Development
Although progranulin expression increases as cells mature,[10] they are still involved in the development of multiple cell types. Progranulin is hypothesized to be a neurotrophic factor involved in corticogenisis. Induced pluripotent stem cell lines (IPSC) harboring the GRN mutation show a decrease in cortical neuronal differentiation ability.[18] A recent mice study suggests that progranulin may be involved in regulating the early development of cerebellar tissue by selecting for individual climbing fibers as they intersect and form synapses with Purkinje cells.[19] In addition, several studies implicate progranulin in synaptic pruning, a microglial process that occurs during development of the neural network.[20] Cytokines, a neuronal marker for synapse elimination, is found to be upregulated in neurons with the GRN mutation.[20] Increased cytokine tagging results in an increase in microglial density and activity around synapses.[20] Progranulin may also be involved in sexual determination during embryonic development.[8]
Inflammation and wound healing
Progranulin levels are elevated when tissue is inflamed. After wounding, keratinocytes, macrophages and neutrophils increase production of progranulin.[8] Neutrophils are capable of secreting elastase into the extracellular matrix that is capable of cleaving progranulin into granulin peptides, that promote further promote inflammation.[8] SLPI, inhibitors of elastase, are also released by neutrophiles and macrophages to modulate progranulin cleavage.[8] Addition of granulin B in cultured epithelial cells causes cells to secrete IL-8, a chemical that attracts monocytes and neutrophils, which further suggests the involvement of granulin peptides in promoting inflammation.[8] The addition of exogenous SLPI and progranulin is able to alleviate the enhanced inflammatory response of mice that are unable to inhibit the cleavage of progranulin.[8]
Cell proliferation
Progranulin is highly expressed in cells that are highly proliferative in nature.[8] Several studies implicate progranulin in tumorigenesis and neuronal outgrowth. Progranulin promotes mitogenesis in epithelial cultures.[8] When two epithelial lines were cultured in media with recombinant PGRN, proliferation was stimulated.[9] Knockout of both progranulin homologues in a zebrafish model reduces axonal outgrowth.[10] In primary cortical and motor neurons, progranulin regulates neuronal outgrowth and survival.[10] In primary motor neurons, progranulin has been shown to increase neurite outgrowth by regulating the glycogen synthase kinase-3 beta.[10] Progranulin may function as an autocrine growth factor in tumorigenesis.[15]
Lysosomal function
The discovery of a GRN mutation leading to lysosomal storage disorder led to many studies that explored progranulin's role in regulating protein homeostasis via the lysosomal pathway. Transcriptional gene network interference study suggests that progranulin is highly involved in lysosomal function and organization.[21] Imaging studies have shown co-localization of progranulin and lysosomal marker LAMP-1.[11] Progranulin expression is regulated by TFEB, a transcription factor that mediates proteins involved in lysosomal biosynthesis.[11] Progranulin may be involved in regulating protease activity. Proteases that could be regulated by progranulin include prosaposin, which is cleaved into saposin peptides in the lysosome, and cathepsin D, the primary protease involved in protein aggregate break down.[9] GRN mutation shares similar neuropathology and clinical phenotype with CHMP2B and VCP mutations, genes that are both involved in the trafficking and breakdown of proteins involved in lysosomal function.[8]
Clinical significance
Frontotemporal dementia
Heterozygous mutation of the GRN gene leading to progranulin haploinsufficiency causes Frontotemporal Dementia. [22][23][24] These mutations include frameshift, splice site, nonsense signal peptide, Kozak sequence disruptions and missense mutations, which result in either nonsense-mediated decay or the production of non-functional protein.[8] Patients with GRN caused FTD (GRN-FTD) exhibit asymmetric brain atrophy, although age of onset, disease progression and clinical symptoms vary, suggesting that other genetic or environmental factors may be involved in disease expression.[10][8] Pathological indicators include cytosolic ubiquitin deposits enriched in hyperphosphorylated TAR DNA Binding Protein (TDP-43), autophagy-related protein aggregates, ubiquitin-binding protein p62, lentiform intranuclear inclusions, dystrophic neurites and inflammation.[15][8][9] Patients with the heterozygote mutation exhibit a reduction of 70-80% serum progranulin levels when compared to controls.[15] Reprogrammed stem cells restore GRN mRNA levels to 50%, further suggesting that some other genetic or environmental factor is involved in regulating FTD disease expression.[15] Mice exhibit reduced autophagic flux and autophagy-dependent clearance.[9] Human FTLD-GRN derived fibroblasts show decrease lysosomal protease activity and lymphoblasts containing neuronal ceroid lipofuscinosis-like storage material.[9] FTLD-GRN IPSC cortical Neurons have enlarged vesicles, lipofuscin accumulation and cathepsin D deficiency.[9]
Neuronal ceroid lipofuscinosis
Homozygous mutation of the GRN gene causes neuronal ceroid lipofuscinosis (NCL) characterized by an accumulation of autofluorescent lipofuscin, enlarged vacuoles, impairment in lysosomal activity, retinal & brain degeneration, exaggerated inflammatory responses, microgliosis, astrogliosis and behavioral dysfunction such as OCD-like and disinhibition-like behavior.[15][9] Aged GRN double mutant mice have lipofuscin deposits and enlarge lysosomes, while one group found phosphorylated TDP-43.[9]
Other diseases
Progranulin may also be involved in cancer development, atherosclerosis and metabolic disease. Progranulin can promote cyclin D1 expression in breast cancer lines and phosphorylation of proteins through extracellular regulated kinase signaling pathways.[8] Progranulin is highly expressed in ovarian, adrenal carcinomas and immortalized epithelial cells.[8] There is a correlation between Progranulin concentration and cancer severity.[9] Granulin release by macrophages has been associated with fibrotic hepatic metastasis in pancreatic cancer.[25] The human liver fluke (Opisthorchis viverrini) contributes to the development of bile duct (liver) cancer by secreting a granulin-like growth hormone.[26] Progranulin may also be involved in promoting the progression of atherosclerosis.[15] While progranulin may be anti-atherogenic, granulins may be pro-atherogenic.[15] Increased serum and plasma progranulin levels in patients with type 2 diabetes and visceral obesity implicating progranulin in metabolic diseases.[15]
References
- GRCh38: Ensembl release 89: ENSG00000030582 - Ensembl, May 2017
- GRCm38: Ensembl release 89: ENSMUSG00000034708 - Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- Bhandari V, Bateman A (October 1992). "Structure and chromosomal location of the human granulin gene". Biochemical and Biophysical Research Communications. 188 (1): 57–63. doi:10.1016/0006-291X(92)92349-3. PMID 1417868.
- Zhang H, Serrero G (November 1998). "Inhibition of tumorigenicity of the teratoma PC cell line by transfection with antisense cDNA for PC cell-derived growth factor (PCDGF, epithelin/granulin precursor)". Proceedings of the National Academy of Sciences of the United States of America. 95 (24): 14202–7. Bibcode:1998PNAS...9514202Z. doi:10.1073/pnas.95.24.14202. PMC 24351. PMID 9826678.
- "Entrez Gene: GRN granulin".
- Eriksen JL, Mackenzie IR (January 2008). "Progranulin: normal function and role in neurodegeneration". Journal of Neurochemistry. 104 (2): 287–97. doi:10.1111/j.1471-4159.2007.04968.x. PMID 17953663.
- Paushter DH, Du H, Feng T, Hu F (May 2018). "The lysosomal function of progranulin, a guardian against neurodegeneration". Acta Neuropathologica. 136 (1): 1–17. doi:10.1007/s00401-018-1861-8. PMC 6117207. PMID 29744576.
- Petkau TL, Leavitt BR (July 2014). "Progranulin in neurodegenerative disease". Trends in Neurosciences. 37 (7): 388–98. doi:10.1016/j.tins.2014.04.003. PMID 24800652.
- Kao AW, McKay A, Singh PP, Brunet A, Huang EJ (June 2017). "Progranulin, lysosomal regulation and neurodegenerative disease". Nature Reviews. Neuroscience. 18 (6): 325–333. doi:10.1038/nrn.2017.36. PMC 6040832. PMID 28435163.
- Benussi L, Ciani M, Tonoli E, Morbin M, Palamara L, Albani D, et al. (April 2016). "Loss of exosomes in progranulin-associated frontotemporal dementia". Neurobiology of Aging. 40: 41–49. doi:10.1016/j.neurobiolaging.2016.01.001. PMID 26973102.
- Hu F, Padukkavidana T, Vægter CB, Brady OA, Zheng Y, Mackenzie IR, et al. (November 2010). "Sortilin-mediated endocytosis determines levels of the frontotemporal dementia protein, progranulin". Neuron. 68 (4): 654–67. doi:10.1016/j.neuron.2010.09.034. PMC 2990962. PMID 21092856.
- Zhou X, Sun L, Bracko O, Choi JW, Jia Y, Nana AL, et al. (May 2017). "Impaired prosaposin lysosomal trafficking in frontotemporal lobar degeneration due to progranulin mutations". Nature Communications. 8: 15277. Bibcode:2017NatCo...815277Z. doi:10.1038/ncomms15277. PMC 5477518. PMID 28541286.
- Nguyen AD, Nguyen TA, Martens LH, Mitic LL, Farese RV (December 2013). "Progranulin: at the interface of neurodegenerative and metabolic diseases". Trends in Endocrinology and Metabolism. 24 (12): 597–606. doi:10.1016/j.tem.2013.08.003. PMC 3842380. PMID 24035620.
- Hoque M, Young TM, Lee CG, Serrero G, Mathews MB, Pe'ery T (March 2003). "The growth factor granulin interacts with cyclin T1 and modulates P-TEFb-dependent transcription". Molecular and Cellular Biology. 23 (5): 1688–702. doi:10.1128/MCB.23.5.1688-1702.2003. PMC 151712. PMID 12588988.
- Zhou Y, Li L, Liu Q, Xing G, Kuai X, Sun J, et al. (May 2008). "E3 ubiquitin ligase SIAH1 mediates ubiquitination and degradation of TRB3". Cellular Signalling. 20 (5): 942–8. doi:10.1016/j.cellsig.2008.01.010. PMID 18276110.
- Raitano S, Ordovàs L, De Muynck L, Guo W, Espuny-Camacho I, Geraerts M, et al. (January 2015). "Restoration of progranulin expression rescues cortical neuron generation in an induced pluripotent stem cell model of frontotemporal dementia". Stem Cell Reports. 4 (1): 16–24. doi:10.1016/j.stemcr.2014.12.001. PMC 4297877. PMID 25556567.
- Uesaka N, Abe M, Konno K, Yamazaki M, Sakoori K, Watanabe T, et al. (February 2018). "Retrograde Signaling from Progranulin to Sort1 Counteracts Synapse Elimination in the Developing Cerebellum". Neuron. 97 (4): 796–805.e5. doi:10.1016/j.neuron.2018.01.018. PMID 29398357.
- Lui H, Zhang J, Makinson SR, Cahill MK, Kelley KW, Huang HY, et al. (May 2016). "Progranulin Deficiency Promotes Circuit-Specific Synaptic Pruning by Microglia via Complement Activation". Cell. 165 (4): 921–35. doi:10.1016/j.cell.2016.04.001. PMC 4860138. PMID 27114033.
- Götzl JK, Lang CM, Haass C, Capell A (December 2016). "Impaired protein degradation in FTLD and related disorders". Ageing Research Reviews. 32: 122–139. doi:10.1016/j.arr.2016.04.008. PMID 27166223.
- Mackenzie IR (July 2007). "The neuropathology and clinical phenotype of FTD with progranulin mutations". Acta Neuropathologica. 114 (1): 49–54. doi:10.1007/s00401-007-0223-8. PMID 17458552.
- Baker M, Mackenzie IR, Pickering-Brown SM, Gass J, Rademakers R, Lindholm C, et al. (August 2006). "Mutations in progranulin cause tau-negative frontotemporal dementia linked to chromosome 17". Nature. 442 (7105): 916–9. Bibcode:2006Natur.442..916B. doi:10.1038/nature05016. PMID 16862116.
- Cruts M, Gijselinck I, van der Zee J, Engelborghs S, Wils H, Pirici D, et al. (August 2006). "Null mutations in progranulin cause ubiquitin-positive frontotemporal dementia linked to chromosome 17q21". Nature. 442 (7105): 920–4. Bibcode:2006Natur.442..920C. doi:10.1038/nature05017. PMID 16862115.
- Nielsen SR, Quaranta V, Linford A, Emeagi P, Rainer C, Santos A, et al. (May 2016). "Macrophage-secreted granulin supports pancreatic cancer metastasis by inducing liver fibrosis". Nature Cell Biology. 18 (5): 549–60. doi:10.1038/ncb3340. PMC 4894551. PMID 27088855.
- Smout MJ, Laha T, Mulvenna J, Sripa B, Suttiprapa S, Jones A, et al. (October 2009). "A granulin-like growth factor secreted by the carcinogenic liver fluke, Opisthorchis viverrini, promotes proliferation of host cells". PLoS Pathogens. 5 (10): e1000611. doi:10.1371/journal.ppat.1000611. PMC 2749447. PMID 19816559.
Further reading
- Serrero G (August 2003). "Autocrine growth factor revisited: PC-cell-derived growth factor (progranulin), a critical player in breast cancer tumorigenesis". Biochemical and Biophysical Research Communications. 308 (3): 409–13. doi:10.1016/S0006-291X(03)01452-9. PMID 12914763.
- Ahmed Z, Mackenzie IR, Hutton ML, Dickson DW (February 2007). "Progranulin in frontotemporal lobar degeneration and neuroinflammation". Journal of Neuroinflammation. 4: 7. doi:10.1186/1742-2094-4-7. PMC 1805428. PMID 17291356.
- Pickering-Brown SM (July 2007). "Progranulin and frontotemporal lobar degeneration". Acta Neuropathologica. 114 (1): 39–47. doi:10.1007/s00401-007-0241-6. PMID 17572900.
- Bhandari V, Palfree RG, Bateman A (March 1992). "Isolation and sequence of the granulin precursor cDNA from human bone marrow reveals tandem cysteine-rich granulin domains". Proceedings of the National Academy of Sciences of the United States of America. 89 (5): 1715–9. Bibcode:1992PNAS...89.1715B. doi:10.1073/pnas.89.5.1715. PMC 48523. PMID 1542665.
- Plowman GD, Green JM, Neubauer MG, Buckley SD, McDonald VL, Todaro GJ, Shoyab M (June 1992). "The epithelin precursor encodes two proteins with opposing activities on epithelial cell growth". The Journal of Biological Chemistry. 267 (18): 13073–8. PMID 1618805.
- Bateman A, Belcourt D, Bennett H, Lazure C, Solomon S (December 1990). "Granulins, a novel class of peptide from leukocytes". Biochemical and Biophysical Research Communications. 173 (3): 1161–8. doi:10.1016/S0006-291X(05)80908-8. PMID 2268320.
- Maruyama K, Sugano S (January 1994). "Oligo-capping: a simple method to replace the cap structure of eukaryotic mRNAs with oligoribonucleotides". Gene. 138 (1–2): 171–4. doi:10.1016/0378-1119(94)90802-8. PMID 8125298.
- Baba T, Hoff HB, Nemoto H, Lee H, Orth J, Arai Y, Gerton GL (March 1993). "Acrogranin, an acrosomal cysteine-rich glycoprotein, is the precursor of the growth-modulating peptides, granulins, and epithelins, and is expressed in somatic as well as male germ cells". Molecular Reproduction and Development. 34 (3): 233–43. doi:10.1002/mrd.1080340302. PMID 8471244.
- Kardana A, Bagshawe KD, Coles B, Read D, Taylor M (April 1993). "Characterisation of UGP and its relationship with beta-core fragment". British Journal of Cancer. 67 (4): 686–92. doi:10.1038/bjc.1993.127. PMC 1968365. PMID 8471426.
- Zhou J, Gao G, Crabb JW, Serrero G (May 1993). "Purification of an autocrine growth factor homologous with mouse epithelin precursor from a highly tumorigenic cell line". The Journal of Biological Chemistry. 268 (15): 10863–9. PMID 8496151.
- Andersson B, Wentland MA, Ricafrente JY, Liu W, Gibbs RA (April 1996). "A "double adaptor" method for improved shotgun library construction". Analytical Biochemistry. 236 (1): 107–13. doi:10.1006/abio.1996.0138. PMID 8619474.
- Bhandari V, Daniel R, Lim PS, Bateman A (October 1996). "Structural and functional analysis of a promoter of the human granulin/epithelin gene". The Biochemical Journal. 319 ( Pt 2) (2): 441–7. doi:10.1042/bj3190441. PMC 1217788. PMID 8912679.
- Yu W, Andersson B, Worley KC, Muzny DM, Ding Y, Liu W, Ricafrente JY, Wentland MA, Lennon G, Gibbs RA (April 1997). "Large-scale concatenation cDNA sequencing". Genome Research. 7 (4): 353–8. doi:10.1101/gr.7.4.353. PMC 139146. PMID 9110174.
- Suzuki Y, Yoshitomo-Nakagawa K, Maruyama K, Suyama A, Sugano S (October 1997). "Construction and characterization of a full length-enriched and a 5'-end-enriched cDNA library". Gene. 200 (1–2): 149–56. doi:10.1016/S0378-1119(97)00411-3. PMID 9373149.
- Trinh DP, Brown KM, Jeang KT (March 1999). "Epithelin/granulin growth factors: extracellular cofactors for HIV-1 and HIV-2 Tat proteins". Biochemical and Biophysical Research Communications. 256 (2): 299–306. doi:10.1006/bbrc.1999.0317. PMID 10079180.
- He Z, Bateman A (July 1999). "Progranulin gene expression regulates epithelial cell growth and promotes tumor growth in vivo". Cancer Research. 59 (13): 3222–9. PMID 10397269.
- Thornton MA, Poncz M, Korostishevsky M, Yakobson E, Usher S, Seligsohn U, Peretz H (September 1999). "The human platelet alphaIIb gene is not closely linked to its integrin partner beta3". Blood. 94 (6): 2039–47. PMID 10477733.