Embryonic stem cell
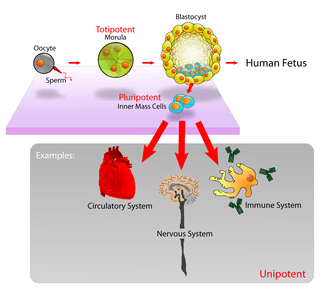
Embryonic stem cells (ES cells or ESCs) are pluripotent stem cells derived from the inner cell mass of a blastocyst, an early-stage pre-implantation embryo.[1][2] Human embryos reach the blastocyst stage 4–5 days post fertilization, at which time they consist of 50–150 cells. Isolating the embryoblast, or inner cell mass (ICM) results in destruction of the blastocyst, a process which raises ethical issues, including whether or not embryos at the pre-implantation stage should have the same moral considerations as embryos in the post-implantation stage of development.[3][4]
Researchers are currently focusing heavily on the therapeutic potential of embryonic stem cells, with clinical use being the goal for many laboratories.[5] Potential uses include the treatment of diabetes and heart disease.[5] The cells are being studied to be used as clinical therapies, models of genetic disorders, and cellular/DNA repair. However, adverse effects in the research and clinical processes such as tumours and unwanted immune responses have also been reported.[6]
Properties

Embryonic stem cells (ESCs), derived from the blastocyst stage of early mammalian embryos, are distinguished by their ability to differentiate into any embryonic cell type and by their ability to self-renew. It is these traits that makes them valuable in the scientific and medical fields. ESCs have a normal karyotype, maintain high telomerase activity, and exhibit remarkable long-term proliferative potential.[7]
Pluripotent
Embryonic stem cells of the inner cell mass are pluripotent, meaning they are able to differentiate to generate primitive ectoderm, which ultimately differentiates during gastrulation into all derivatives of the three primary germ layers: ectoderm, endoderm, and mesoderm. These germ layers generate each of the more than 220 cell types in the adult human body. When provided with the appropriate signals, ESCs initially form precursor cells that in subsequently differentiate into the desired cell types. Pluripotency distinguishes embryonic stem cells from adult stem cells, which are multipotent and can only produce a limited number of cell types.
Self renewal and repair of structure
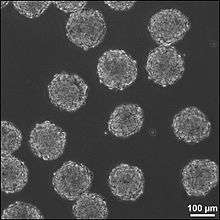
Under defined conditions, embryonic stem cells are capable of self-renewing indefinitely in an undifferentiated state. Self-renewal conditions must prevent the cells from clumping and maintain an environment that supports an unspecialized state.[8] Typically this is done in the lab with media containing serum and leukemia inhibitory factor or serum-free media supplements with two inhibitory drugs ("2i"), the MEK inhibitor PD03259010 and GSK-3 inhibitor CHIR99021.[9]
Growth
ESCs divide very frequently due to a shortened G1 phase in their cell cycle. Rapid cell division allows the cells to quickly grow in number, but not size, which is important for early embryo development. In ESCs, cyclin A and cyclin E proteins involved in the G1/S transition are always expressed at high levels.[10] Cyclin-dependent kinases such as CDK2 that promote cell cycle progression are overactive, in part due to downregulation of their inhibitors.[11] Retinoblastoma proteins that inhibit the transcription factor E2F until the cell is ready to enter S phase are hyperphosphorylated and inactivated in ESCs, leading to continual expression of proliferation genes.[10] These changes result in accelerated cycles of cell division. Although the shortened G1 phase has been linked to maintenance of pluripotency,[12] ESCs grown in serum-free 2i conditions do express hypo-phosphorylated active Retinoblastoma proteins and have an elongated G1 phase.[13] Despite this difference in the cell cycle when compared to ESCs grown in media containing serum these cells have similar pluripotent characteristics.[14] Pluripotency factors Oct4 and Nanog play a role in transcriptionally regulating the ESC cell cycle.[15][16]
Uses
Due to their plasticity and potentially unlimited capacity for self-renewal, embryonic stem cell therapies have been proposed for regenerative medicine and tissue replacement after injury or disease. Pluripotent stem cells have shown promise in treating a number of varying conditions, including but not limited to: spinal cord injuries, age related macular degeneration, diabetes, neurodegenerative disorders (such as Parkinson's disease), AIDS, etc.[17] In addition to their potential in regenerative medicine, embryonic stem cells provide a possible alternative source of tissue/organs which serves as a possible solution to the donor shortage dilemma. There are some ethical controversies surrounding this though (see Ethical debate section below). Aside from these uses, ESCs can also be used for research on early human development, certain genetic disease, and in vitro toxicology testing.[7]
Utilizations
According to a 2002 article in PNAS, "Human embryonic stem cells have the potential to differentiate into various cell types, and, thus, may be useful as a source of cells for transplantation or tissue engineering."[18]
However, embryonic stem cells are not limited to cell/tissue engineering.
Cell replacement therapies
Current research focuses on differentiating ESCs into a variety of cell types for eventual use as cell replacement therapies (CRTs). Some of the cell types that have or are currently being developed include cardiomyocytes (CM), neurons, hepatocytes, bone marrow cells, islet cells and endothelial cells.[19] However, the derivation of such cell types from ESCs is not without obstacles, therefore current research is focused on overcoming these barriers. For example, studies are underway to differentiate ESCs into tissue specific CMs and to eradicate their immature properties that distinguish them from adult CMs.[20]
Clinical potential
- Researchers have differentiated ESCs into dopamine-producing cells with the hope that these neurons could be used in the treatment of Parkinson’s disease.[21][22]
- ESCs have been differentiated to natural killer (NK) cells and bone tissue.[23]
- Studies involving ESCs are underway to provide an alternative treatment for diabetes. For example, D’Amour et al. were able to differentiate ESCs into insulin producing cells[24] and researchers at Harvard University were able to produce large quantities of pancreatic beta cells from ES.[25]
- An article published in the European Heart Journal describes a translational process of generating human embryonic stem cell-derived cardiac progenitor cells to be used in clinical trials of patients with severe heart failure.[26]
Drug discovery
Besides becoming an important alternative to organ transplants, ESCs are also being used in field of toxicology and as cellular screens to uncover new chemical entities (NCEs) that can be developed as small molecule drugs. Studies have shown that cardiomyocytes derived from ESCs are validated in vitro models to test drug responses and predict toxicity profiles.[19] ES derived cardiomyocytes have been shown to respond to pharmacological stimuli and hence can be used to assess cardiotoxicity like Torsades de Pointes.[27]
ESC-derived hepatocytes are also useful models that could be used in the preclinical stages of drug discovery. However, the development of hepatocytes from ESCs has proven to be challenging and this hinders the ability to test drug metabolism. Therefore, current research is focusing on establishing fully functional ESC-derived hepatocytes with stable phase I and II enzyme activity.[28]
Models of genetic disorder
Several new studies have started to address the concept of modeling genetic disorders with embryonic stem cells. Either by genetically manipulating the cells, or more recently, by deriving diseased cell lines identified by prenatal genetic diagnosis (PGD), modeling genetic disorders is something that has been accomplished with stem cells. This approach may very well prove valuable at studying disorders such as Fragile-X syndrome, Cystic fibrosis, and other genetic maladies that have no reliable model system.
Yury Verlinsky, a Russian-American medical researcher who specialized in embryo and cellular genetics (genetic cytology), developed prenatal diagnosis testing methods to determine genetic and chromosomal disorders a month and a half earlier than standard amniocentesis. The techniques are now used by many pregnant women and prospective parents, especially couples who have a history of genetic abnormalities or where the woman is over the age of 35 (when the risk of genetically related disorders is higher). In addition, by allowing parents to select an embryo without genetic disorders, they have the potential of saving the lives of siblings that already had similar disorders and diseases using cells from the disease free offspring.[29]
Repair of DNA damage
Differentiated somatic cells and ES cells use different strategies for dealing with DNA damage. For instance, human foreskin fibroblasts, one type of somatic cell, use non-homologous end joining (NHEJ), an error prone DNA repair process, as the primary pathway for repairing double-strand breaks (DSBs) during all cell cycle stages.[30] Because of its error-prone nature, NHEJ tends to produce mutations in a cell’s clonal descendants.
ES cells use a different strategy to deal with DSBs.[31] Because ES cells give rise to all of the cell types of an organism including the cells of the germ line, mutations arising in ES cells due to faulty DNA repair are a more serious problem than in differentiated somatic cells. Consequently, robust mechanisms are needed in ES cells to repair DNA damages accurately, and if repair fails, to remove those cells with un-repaired DNA damages. Thus, mouse ES cells predominantly use high fidelity homologous recombinational repair (HRR) to repair DSBs.[31] This type of repair depends on the interaction of the two sister chromosomes formed during S phase and present together during the G2 phase of the cell cycle. HRR can accurately repair DSBs in one sister chromosome by using intact information from the other sister chromosome. Cells in the G1 phase of the cell cycle (i.e. after metaphase/cell division but prior the next round of replication) have only one copy of each chromosome (i.e. sister chromosomes aren’t present). Mouse ES cells lack a G1 checkpoint and do not undergo cell cycle arrest upon acquiring DNA damage.[32] Rather they undergo programmed cell death (apoptosis) in response to DNA damage.[33] Apoptosis can be used as a fail-safe strategy to remove cells with un-repaired DNA damages in order to avoid mutation and progression to cancer.[34] Consistent with this strategy, mouse ES stem cells have a mutation frequency about 100-fold lower than that of isogenic mouse somatic cells.[35]
Clinical trial
On January 23, 2009, Phase I clinical trials for transplantation of oligodendrocytes (a cell type of the brain and spinal cord) derived from human ES cells into spinal cord-injured individuals received approval from the U.S. Food and Drug Administration (FDA), marking it the world's first human ES cell human trial.[36] The study leading to this scientific advancement was conducted by Hans Keirstead and colleagues at the University of California, Irvine and supported by Geron Corporation of Menlo Park, CA, founded by Michael D. West, PhD. A previous experiment had shown an improvement in locomotor recovery in spinal cord-injured rats after a 7-day delayed transplantation of human ES cells that had been pushed into an oligodendrocytic lineage.[37] The phase I clinical study was designed to enroll about eight to ten paraplegics who have had their injuries no longer than two weeks before the trial begins, since the cells must be injected before scar tissue is able to form. The researchers emphasized that the injections were not expected to fully cure the patients and restore all mobility. Based on the results of the rodent trials, researchers speculated that restoration of myelin sheathes and an increase in mobility might occur. This first trial was primarily designed to test the safety of these procedures and if everything went well, it was hoped that it would lead to future studies that involve people with more severe disabilities.[38] The trial was put on hold in August 2009 due to FDA concerns regarding a small number of microscopic cysts found in several treated rat models but the hold was lifted on July 30, 2010.[39]
In October 2010 researchers enrolled and administered ESTs to the first patient at Shepherd Center in Atlanta.[40] The makers of the stem cell therapy, Geron Corporation, estimated that it would take several months for the stem cells to replicate and for the GRNOPC1 therapy to be evaluated for success or failure.
In November 2011 Geron announced it was halting the trial and dropping out of stem cell research for financial reasons, but would continue to monitor existing patients, and was attempting to find a partner that could continue their research.[41] In 2013 BioTime, led by CEO Dr. Michael D. West, acquired all of Geron's stem cell assets, with the stated intention of restarting Geron's embryonic stem cell-based clinical trial for spinal cord injury research.[42]
BioTime company Asterias Biotherapeutics (NYSE MKT: AST) was granted a $14.3 million Strategic Partnership Award by the California Institute for Regenerative Medicine (CIRM) to re-initiate the world’s first embryonic stem cell-based human clinical trial, for spinal cord injury. Supported by California public funds, CIRM is the largest funder of stem cell-related research and development in the world.[43]
The award provides funding for Asterias to reinitiate clinical development of AST-OPC1 in subjects with spinal cord injury and to expand clinical testing of escalating doses in the target population intended for future pivotal trials.[43]
AST-OPC1 is a population of cells derived from human embryonic stem cells (hESCs) that contains oligodendrocyte progenitor cells (OPCs). OPCs and their mature derivatives called oligodendrocytes provide critical functional support for nerve cells in the spinal cord and brain. Asterias recently presented the results from phase 1 clinical trial testing of a low dose of AST-OPC1 in patients with neurologically-complete thoracic spinal cord injury. The results showed that AST-OPC1 was successfully delivered to the injured spinal cord site. Patients followed 2–3 years after AST-OPC1 administration showed no evidence of serious adverse events associated with the cells in detailed follow-up assessments including frequent neurological exams and MRIs. Immune monitoring of subjects through one year post-transplantation showed no evidence of antibody-based or cellular immune responses to AST-OPC1. In four of the five subjects, serial MRI scans performed throughout the 2–3 year follow-up period indicate that reduced spinal cord cavitation may have occurred and that AST-OPC1 may have had some positive effects in reducing spinal cord tissue deterioration. There was no unexpected neurological degeneration or improvement in the five subjects in the trial as evaluated by the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) exam.[43]
The Strategic Partnership III grant from CIRM will provide funding to Asterias to support the next clinical trial of AST-OPC1 in subjects with spinal cord injury, and for Asterias’ product development efforts to refine and scale manufacturing methods to support later-stage trials and eventually commercialization. CIRM funding will be conditional on FDA approval for the trial, completion of a definitive agreement between Asterias and CIRM, and Asterias’ continued progress toward the achievement of certain pre-defined project milestones.[43]
Concern and controversy
Adverse effects
The major concern with the possible transplantation of ESC into patients as therapies is their ability to form tumors including teratoma.[44] Safety issues prompted the FDA to place a hold on the first ESC clinical trial, however no tumors were observed.
The main strategy to enhance the safety of ESC for potential clinical use is to differentiate the ESC into specific cell types (e.g. neurons, muscle, liver cells) that have reduced or eliminated ability to cause tumors. Following differentiation, the cells are subjected to sorting by flow cytometry for further purification. ESC are predicted to be inherently safer than IPS cells created with genetically-integrating viral vectors because they are not genetically modified with genes such as c-Myc that are linked to cancer. Nonetheless, ESC express very high levels of the iPS inducing genes and these genes including Myc are essential for ESC self-renewal and pluripotency,[45] and potential strategies to improve safety by eliminating c-Myc expression are unlikely to preserve the cells' "stemness". However, N-myc and L-myc have been identified to induce iPS cells instead of c-myc with similar efficiency.[46] More recent protocols to induce pluripotency bypass these problems completely by using non-integrating RNA viral vectors such as sendai virus or mRNA transfection.
Ethical debate
Due to the nature of embryonic stem cell research, there are a lot of controversial opinions on the topic. Since harvesting embryonic stem cells necessitates destroying the embryo from which those cells are obtained, the moral status of the embryo comes into question. Some people argue that the 5-day old mass of cells is too young to achieve personhood or that the embryo, if donated from an IVF clinic (which is where labs typically acquire embryos from), would otherwise go to medical waste anyway. Opponents of ESC research claim that an embryo is a human life, therefore destroying it is murder and the embryo must be protected under the same ethical view as a more developed human being.[47]
History
- 1964: Lewis Kleinsmith and G. Barry Pierce Jr. isolated a single type of cell from a teratocarcinoma, a tumor now known from a germ cell.[48] These cells were isolated from the teratocarcinoma replicated and grew in cell culture as a stem cell and are now known as embryonal carcinoma (EC) cells. Although similarities in morphology and differentiating potential (pluripotency) led to the use of EC cells as the in vitro model for early mouse development,[49] EC cells harbor genetic mutations and often abnormal karyotypes that accumulated during the development of the teratocarcinoma. These genetic aberrations further emphasized the need to be able to culture pluripotent cells directly from the inner cell mass.

- 1981: Embryonic stem cells (ES cells) were independently first derived from a mouse embryos by two groups. Martin Evans and Matthew Kaufman from the Department of Genetics, University of Cambridge published first in July, revealing a new technique for culturing the mouse embryos in the uterus to allow for an increase in cell number, allowing for the derivation of ES cell from these embryos.[50] Gail R. Martin, from the Department of Anatomy, University of California, San Francisco, published her paper in December and coined the term “Embryonic Stem Cell”.[51] She showed that embryos could be cultured in vitro and that ES cells could be derived from these embryos.
- 1989: Mario R. Cappechi, Martin J. Evans, and Oliver Smithies publish their research that details their isolation and genetic modifications of embryonic stem cells, creating the first "knockout mice".[52] In creating knockout mice, this publication provided scientists with an entirely new way to study disease.
- 1998: A team from the University of Wisconsin, Madison (James A. Thomson, Joseph Itskovitz-Eldor, Sander S. Shapiro, Michelle A. Waknitz, Jennifer J. Swiergiel, Vivienne S. Marshall, and Jeffrey M. Jones) publish a paper titled "Embryonic Stem Cell Lines Derived From Human Blastocysts". The researchers behind this study not only created the first embryonic stem cells, but recognized their pluripotency, as well as their capacity for self-renewal. The abstract of the paper notes the significance of the discovery with regards to the fields of developmental biology and drug discovery.[53]
- 2001: President George W. Bush allows federal funding to support research on roughly 60—at this time, already existing—lines of embryonic stem cells. Seeing as the limited lines that Bush allowed research on had already been established, this law supported embryonic stem cell research without raising any ethical questions that could arise with the creation of new lines under federal budget.[54]
- 2006: Japanese scientists Shinya Yamanaka and Kazutoshi Takashi publish a paper describing the induction of pluripotent stem cells from cultures of adult mouse fibroblasts. Induced pluripotent stem cells (iPSCs) are a huge discovery, as they are seemingly identical to embryonic stem cells and could be used without sparking the same moral controversy.[55]
- January, 2009: The US Food and Drug Administration (FDA) provides approval for Geron Corporation's phase I trial of their human embryonic stem cell-derived treatment for spinal cord injuries. The announcement was met with excitement from the scientific community, but also with wariness from stem cell opposers. The treatment cells were, however, derived from the cell lines approved under George W. Bush's ESC policy.[56]
- March, 2009: Executive Order 13505 is signed by President Barack Obama, removing the restrictions put in place on federal funding for human stem cells by the previous presidential administration. This would allow the National Institutes of Health (NIH) to provide funding for hESC research. The document also states that the NIH must provide revised federal funding guidelines within 120 days of the order's signing.[57]
Techniques and conditions for derivation and culture
Derivation from humans
In vitro fertilization generates multiple embryos. The surplus of embryos is not clinically used or is unsuitable for implantation into the patient, and therefore may be donated by the donor with consent. Human embryonic stem cells can be derived from these donated embryos or additionally they can also be extracted from cloned embryos using a cell from a patient and a donated egg.[58] The inner cell mass (cells of interest), from the blastocyst stage of the embryo, is separated from the trophectoderm, the cells that would differentiate into extra-embryonic tissue. Immunosurgery, the process in which antibodies are bound to the trophectoderm and removed by another solution, and mechanical dissection are performed to achieve separation. The resulting inner cell mass cells are plated onto cells that will supply support. The inner cell mass cells attach and expand further to form a human embryonic cell line, which are undifferentiated. These cells are fed daily and are enzymatically or mechanically separated every four to seven days. For differentiation to occur, the human embryonic stem cell line is removed from the supporting cells to form embryoid bodies, is co-cultured with a serum containing necessary signals, or is grafted in a three-dimensional scaffold to result.[59]
Derivation from other animals
Embryonic stem cells are derived from the inner cell mass of the early embryo, which are harvested from the donor mother animal. Martin Evans and Matthew Kaufman reported a technique that delays embryo implantation, allowing the inner cell mass to increase. This process includes removing the donor mother's ovaries and dosing her with progesterone, changing the hormone environment, which causes the embryos to remain free in the uterus. After 4–6 days of this intrauterine culture, the embryos are harvested and grown in in vitro culture until the inner cell mass forms “egg cylinder-like structures,” which are dissociated into single cells, and plated on fibroblasts treated with mitomycin-c (to prevent fibroblast mitosis). Clonal cell lines are created by growing up a single cell. Evans and Kaufman showed that the cells grown out from these cultures could form teratomas and embryoid bodies, and differentiate in vitro, all of which indicating that the cells are pluripotent.[50]
Gail Martin derived and cultured her ES cells differently. She removed the embryos from the donor mother at approximately 76 hours after copulation and cultured them overnight in a medium containing serum. The following day, she removed the inner cell mass from the late blastocyst using microsurgery. The extracted inner cell mass was cultured on fibroblasts treated with mitomycin-c in a medium containing serum and conditioned by ES cells. After approximately one week, colonies of cells grew out. These cells grew in culture and demonstrated pluripotent characteristics, as demonstrated by the ability to form teratomas, differentiate in vitro, and form embryoid bodies. Martin referred to these cells as ES cells.[51]
It is now known that the feeder cells provide leukemia inhibitory factor (LIF) and serum provides bone morphogenetic proteins (BMPs) that are necessary to prevent ES cells from differentiating.[60][61] These factors are extremely important for the efficiency of deriving ES cells. Furthermore, it has been demonstrated that different mouse strains have different efficiencies for isolating ES cells.[62] Current uses for mouse ES cells include the generation of transgenic mice, including knockout mice. For human treatment, there is a need for patient specific pluripotent cells. Generation of human ES cells is more difficult and faces ethical issues. So, in addition to human ES cell research, many groups are focused on the generation of induced pluripotent stem cells (iPS cells).[63]
Potential method for new cell line derivation
On August 23, 2006, the online edition of Nature scientific journal published a letter by Dr. Robert Lanza (medical director of Advanced Cell Technology in Worcester, MA) stating that his team had found a way to extract embryonic stem cells without destroying the actual embryo.[64] This technical achievement would potentially enable scientists to work with new lines of embryonic stem cells derived using public funding in the USA, where federal funding was at the time limited to research using embryonic stem cell lines derived prior to August 2001. In March, 2009, the limitation was lifted.[65]
Induced pluripotent stem cells
The iPSC technology was pioneered by Shinya Yamanaka’s lab in Kyoto, Japan, who showed in 2006 that the introduction of four specific genes encoding transcription factors could convert adult cells into pluripotent stem cells.[66] He was awarded the 2012 Nobel Prize along with Sir John Gurdon "for the discovery that mature cells can be reprogrammed to become pluripotent." [67]
In 2007 it was shown that pluripotent stem cells highly similar to embryonic stem cells can be generated by the delivery of three genes (Oct4, Sox2, and Klf4) to differentiated cells.[68] The delivery of these genes "reprograms" differentiated cells into pluripotent stem cells, allowing for the generation of pluripotent stem cells without the embryo. Because ethical concerns regarding embryonic stem cells typically are about their derivation from terminated embryos, it is believed that reprogramming to these "induced pluripotent stem cells" (iPS cells) may be less controversial. Both human and mouse cells can be reprogrammed by this methodology, generating both human pluripotent stem cells and mouse pluripotent stem cells without an embryo.[69]
This may enable the generation of patient specific ES cell lines that could potentially be used for cell replacement therapies. In addition, this will allow the generation of ES cell lines from patients with a variety of genetic diseases and will provide invaluable models to study those diseases.
However, as a first indication that the induced pluripotent stem cell (iPS) cell technology can in rapid succession lead to new cures, it was used by a research team headed by Rudolf Jaenisch of the Whitehead Institute for Biomedical Research in Cambridge, Massachusetts, to cure mice of sickle cell anemia, as reported by Science journal's online edition on December 6, 2007.[70][71]
On January 16, 2008, a California-based company, Stemagen, announced that they had created the first mature cloned human embryos from single skin cells taken from adults. These embryos can be harvested for patient matching embryonic stem cells.[72]
Contamination by reagents used in cell culture
The online edition of Nature Medicine published a study on January 24, 2005, which stated that the human embryonic stem cells available for federally funded research are contaminated with non-human molecules from the culture medium used to grow the cells.[73] It is a common technique to use mouse cells and other animal cells to maintain the pluripotency of actively dividing stem cells. The problem was discovered when non-human sialic acid in the growth medium was found to compromise the potential uses of the embryonic stem cells in humans, according to scientists at the University of California, San Diego.[74]
However, a study published in the online edition of Lancet Medical Journal on March 8, 2005 detailed information about a new stem cell line that was derived from human embryos under completely cell- and serum-free conditions. After more than 6 months of undifferentiated proliferation, these cells demonstrated the potential to form derivatives of all three embryonic germ layers both in vitro and in teratomas. These properties were also successfully maintained (for more than 30 passages) with the established stem cell lines.[75]
See also
References
- Thomson; Itskovitz-Eldor, J; Shapiro, SS; Waknitz, MA; Swiergiel, JJ; Marshall, VS; Jones, JM (1998). "Blastocysts Embryonic Stem Cell Lines Derived from Human". Science. 282 (5391): 1145–1147. Bibcode:1998Sci...282.1145T. doi:10.1126/science.282.5391.1145. PMID 9804556.
- "NIH Stem Cell Basics. What are embryonic stem cells?". Archived from the original on 2016-08-31. Retrieved 2014-03-25.
- Baldwing A (2009). "Morality and human embryo research. Introduction to the Talking Point on morality and human embryo research". EMBO Reports. 10 (4): 299–300. doi:10.1038/embor.2009.37. PMC 2672902. PMID 19337297.
- Nakaya, Andrea C. (August 1, 2011). Biomedical ethics. San Diego, CA: ReferencePoint Press. pp. 96. ISBN 978-1601521576.
- "Introduction: What are stem cells, and why are they important?". National Institutes of Health. Retrieved 28 October 2018.
- Carla A Herberts; Marcel SG Kwa; Harm PH Hermsen (2011). "Risk factors in the development of stem cell therapy". Journal of Translational Medicine. 9 (29): 29. doi:10.1186/1479-5876-9-29. PMC 3070641. PMID 21418664.
- Thomson, J. A.; Itskovitz-Eldor, J; Shapiro, S. S.; Waknitz, M. A.; Swiergiel, J. J.; Marshall, V. S.; Jones, J. M. (1998). "Embryonic Stem Cell Lines Derived from Human Blastocysts". Science. 282 (5391): 1145–7. Bibcode:1998Sci...282.1145T. doi:10.1126/science.282.5391.1145. PMID 9804556.
- Ying; Nichols, J; Chambers, I; Smith, A (2003). "BMP Induction of Id Proteins Suppresses Differentiation and Sustains Embryonic Stem Cell Self-Renewal in Collaboration with STAT3". Cell. 115 (3): 281–292. doi:10.1016/S0092-8674(03)00847-X. PMID 14636556.
- Martello, G.; Smith, A. (2014). "The nature of embryonic stem cells". Annual Review of Cell and Developmental Biology. 30: 647–75. doi:10.1146/annurev-cellbio-100913-013116. PMID 25288119.
- Boward, B.; Wu, T.; Dalton, S. (2016). "Concise Review: Control of Cell Fate Through Cell Cycle and Pluripotency Networks". Stem Cells. 34 (6): 1427–36. doi:10.1002/stem.2345. PMC 5201256. PMID 26889666.
- White, J.; Stead, E.; Faast, R.; Conn, S.; Cartwright, P.; Dalton, S. (2005). "Developmental activation of the Rb-E2F pathway and establishment of cell cycle-regulated cyclin-dependent kinase activity during embryonic stem cell differentiation". Molecular Biology of the Cell. 16 (4): 2018–27. doi:10.1091/mbc.e04-12-1056. PMC 1073679. PMID 15703208.
- Singh, Amar M.; Dalton, Stephen (2009-08-07). "The cell cycle and Myc intersect with mechanisms that regulate pluripotency and reprogramming". Cell Stem Cell. 5 (2): 141–149. doi:10.1016/j.stem.2009.07.003. ISSN 1875-9777. PMC 2909475. PMID 19664987.
- Ter Huurne, Menno; Chappell, James; Dalton, Stephen; Stunnenberg, Hendrik G. (5 October 2017). "Distinct Cell-Cycle Control in Two Different States of Mouse Pluripotency". Cell Stem Cell. 21 (4): 449–455.e4. doi:10.1016/j.stem.2017.09.004. ISSN 1875-9777. PMC 5658514. PMID 28985526.
- Ying, Qi-Long; Wray, Jason; Nichols, Jennifer; Batlle-Morera, Laura; Doble, Bradley; Woodgett, James; Cohen, Philip; Smith, Austin (2008-05-22). "The ground state of embryonic stem cell self-renewal". Nature. 453 (7194): 519–523. Bibcode:2008Natur.453..519Y. doi:10.1038/nature06968. ISSN 1476-4687. PMC 5328678. PMID 18497825.
- Lee, J.; Go, Y.; Kang, I.; Han, Y. M.; Kim, J. (2010). "Oct-4 controls cell-cycle progression of embryonic stem cells". The Biochemical Journal. 426 (2): 171–81. doi:10.1042/BJ20091439. PMC 2825734. PMID 19968627.
- Zhang, X.; Neganova, I.; Przyborski, S.; Yang, C.; Cooke, M.; Atkinson, S. P.; Anyfantis, G.; Fenyk, S.; Keith, W. N.; Hoare, S. F.; Hughes, O.; Strachan, T.; Stojkovic, M.; Hinds, P. W.; Armstrong, L.; Lako, M. (2009). "A role for NANOG in G1 to S transition in human embryonic stem cells through direct binding of CDK6 and CDC25A". The Journal of Cell Biology. 184 (1): 67–82. doi:10.1083/jcb.200801009. PMC 2615089. PMID 19139263.
- Mahla, Ranjeet (July 19, 2016). "Stem Cell Applications in Regenerative Medicine and Disease Therapeutics". International Journal of Cell Biology. 2016: 6940283. doi:10.1155/2016/6940283. PMC 4969512. PMID 27516776.
- Levenberg, S. (2002). "Endothelial cells derived from human embryonic stem cells". Proceedings of the National Academy of Sciences. 99 (7): 4391–4396. Bibcode:2002PNAS...99.4391L. doi:10.1073/pnas.032074999. PMC 123658. PMID 11917100.
- Davila, JC; Cezar, GG; Thiede, M; Strom, S; Miki, T; Trosko, J (2004). "Use and application of stem cells in toxicology". Toxicological Sciences. 79 (2): 214–23. doi:10.1093/toxsci/kfh100. PMID 15014205.
- Siu, CW; Moore, JC; Li, RA (2007). "Human embryonic stem cell-derived cardiomyocytes for heart therapies". Cardiovascular & Hematological Disorders Drug Targets. 7 (2): 145–52. doi:10.2174/187152907780830851. PMID 17584049.
- Perrier, A. L. (2004). "Derivation of midbrain dopamine neurons from human embryonic stem cells". Proceedings of the National Academy of Sciences. 101 (34): 12543–12548. Bibcode:2004PNAS..10112543P. doi:10.1073/pnas.0404700101. PMC 515094. PMID 15310843.
- Parish, CL; Arenas, E (2007). "Stem-cell-based strategies for the treatment of Parkinson's disease". Neuro-Degenerative Diseases. 4 (4): 339–47. doi:10.1159/000101892. PMID 17627139.
- Waese, EY; Kandel, RA; Stanford, WL (2008). "Application of stem cells in bone repair". Skeletal Radiology. 37 (7): 601–8. doi:10.1007/s00256-007-0438-8. PMID 18193216.
- d'Amour, KA; Bang, AG; Eliazer, S; Kelly, OG; Agulnick, AD; Smart, NG; Moorman, MA; Kroon, E; Carpenter, MK; Baetge, EE (2006). "Production of pancreatic hormone-expressing endocrine cells from human embryonic stem cells". Nature Biotechnology. 24 (11): 1392–401. doi:10.1038/nbt1259. PMID 17053790.
- Colen, B.D. (9 October 2014) Giant leap against diabetes The Harvard Gazette, Retrieved 24 November 2014
- Menasché, Phillip; Vanneaux, Valérie; Fabreguettes, Jean-Roch; Bel, Alain; Tosca, Lucie; Garcia, Sylvie (21 March 2015). "Towards a clinical use of human embryonic stem cell derived-cardiac progenitors: a translational experience". European Heart Journal. 36 (12): 743–750. doi:10.1093/eurheartj/ehu192. PMID 24835485.
- Jensen, J; Hyllner, J; Björquist, P (2009). "Human embryonic stem cell technologies and drug discovery". Journal of Cellular Physiology. 219 (3): 513–9. doi:10.1002/jcp.21732. PMID 19277978.
- Söderdahl, T; Küppers-Munther, B; Heins, N; Edsbagge, J; Björquist, P; Cotgreave, I; Jernström, B (2007). "Glutathione transferases in hepatocyte-like cells derived from human embryonic stem cells". Toxicology in Vitro. 21 (5): 929–37. doi:10.1016/j.tiv.2007.01.021. PMID 17346923.
- "Dr. Yury Verlinsky, 1943–2009: Expert in reproductive technology" Archived 2009-08-08 at the Wayback Machine Chicago Tribune, July 20, 2009
- Mao Z, Bozzella M, Seluanov A, Gorbunova V (September 2008). "DNA repair by nonhomologous end joining and homologous recombination during cell cycle in human cells". Cell Cycle. 7 (18): 2902–6. doi:10.4161/cc.7.18.6679. PMC 2754209. PMID 18769152.
- Tichy ED, Pillai R, Deng L, et al. (November 2010). "Mouse embryonic stem cells, but not somatic cells, predominantly use homologous recombination to repair double-strand DNA breaks". Stem Cells Dev. 19 (11): 1699–711. doi:10.1089/scd.2010.0058. PMC 3128311. PMID 20446816.
- Hong Y, Stambrook PJ (October 2004). "Restoration of an absent G1 arrest and protection from apoptosis in embryonic stem cells after ionizing radiation". Proc. Natl. Acad. Sci. U.S.A. 101 (40): 14443–8. Bibcode:2004PNAS..10114443H. doi:10.1073/pnas.0401346101. PMC 521944. PMID 15452351.
- Aladjem MI, Spike BT, Rodewald LW, et al. (January 1998). "ES cells do not activate p53-dependent stress responses and undergo p53-independent apoptosis in response to DNA damage". Curr. Biol. 8 (3): 145–55. doi:10.1016/S0960-9822(98)70061-2. PMID 9443911.
- Bernstein C, Bernstein H, Payne CM, Garewal H (June 2002). "DNA repair/pro-apoptotic dual-role proteins in five major DNA repair pathways: fail-safe protection against carcinogenesis". Mutat. Res. 511 (2): 145–78. doi:10.1016/S1383-5742(02)00009-1. PMID 12052432.
- Cervantes RB, Stringer JR, Shao C, Tischfield JA, Stambrook PJ (March 2002). "Embryonic stem cells and somatic cells differ in mutation frequency and type". Proc. Natl. Acad. Sci. U.S.A. 99 (6): 3586–90. Bibcode:2002PNAS...99.3586C. doi:10.1073/pnas.062527199. PMC 122567. PMID 11891338.
- "FDA approves human embryonic stem cell study - CNN.com". January 23, 2009. Retrieved May 1, 2010.
- Keirstead HS, Nistor G, Bernal G, et al. (2005). "Human embryonic stem cell-derived oligodendrocyte progenitor cell transplants remyelinate and restore locomotion after spinal cord injury" (PDF). J. Neurosci. 25 (19): 4694–705. doi:10.1523/JNEUROSCI.0311-05.2005. PMC 6724772. PMID 15888645.
- Reinberg, Steven (2009-01-23) FDA OKs 1st Embryonic Stem Cell Trial. The Washington Post
- Geron comments on FDA hold on spinal cord injury trial. geron.com (August 27, 2009)
- Vergano, Dan (11 October 2010). "Embryonic stem cells used on patient for first time". USA Today. Retrieved 12 October 2010.
- Brown, Eryn (November 15, 2011). "Geron exits stem cell research". LA Times. Retrieved 2011-11-15.
- "Great news: BioTime Subsidiary Asterias Acquires Geron Embryonic Stem Cell Program". iPScell.com. October 1, 2013.
- California Institute of Regenerative Medicine Archived 2017-10-24 at the Wayback Machine. BioTime, Inc.
- Knoepfler, Paul S. (2009). "Deconstructing Stem Cell Tumorigenicity: A Roadmap to Safe Regenerative Medicine". Stem Cells. 27 (5): 1050–6. doi:10.1002/stem.37. PMC 2733374. PMID 19415771.
- Varlakhanova, Natalia V.; Cotterman, Rebecca F.; Devries, Wilhelmine N.; Morgan, Judy; Donahue, Leah Rae; Murray, Stephen; Knowles, Barbara B.; Knoepfler, Paul S. (2010). "Myc maintains embryonic stem cell pluripotency and self-renewal". Differentiation. 80 (1): 9–19. doi:10.1016/j.diff.2010.05.001. PMC 2916696. PMID 20537458.
- Wernig, Marius; Meissner, Alexander; Cassady, John P; Jaenisch, Rudolf (2008). "C-Myc is Dispensable for Direct Reprogramming of Mouse Fibroblasts". Cell Stem Cell. 2 (1): 10–2. doi:10.1016/j.stem.2007.12.001. PMID 18371415.
- King, Nancy; Perrin, Jacob (July 7, 2014). "Ethical issues in stem cell research and therapy". Stem Cell Research & Therapy. 5 (4): 85. doi:10.1186/scrt474. PMC 4097842. PMID 25157428.
- Kleinsmith LJ, Pierce GB Jr (1964). "Multipotentiality of Single Embryoncal Carcinoma Cells". Cancer Res. 24: 1544–51. PMID 14234000.
- Martin GR (1980). "Teratocarcinomas and mammalian embryogenesis". Science. 209 (4458): 768–76. Bibcode:1980Sci...209..768M. doi:10.1126/science.6250214. PMID 6250214.
- Evans M, Kaufman M (1981). "Establishment in culture of pluripotent cells from mouse embryos". Nature. 292 (5819): 154–6. Bibcode:1981Natur.292..154E. doi:10.1038/292154a0. PMID 7242681.
- Martin G (1981). "Isolation of a pluripotent cell line from early mouse embryos cultured in medium conditioned by teratocarcinoma stem cells". Proc Natl Acad Sci USA. 78 (12): 7634–8. Bibcode:1981PNAS...78.7634M. doi:10.1073/pnas.78.12.7634. PMC 349323. PMID 6950406.
- "The 2007 Nobel Prize in Physiology or Medicine - Advanced Information". Nobel Prize. Nobel Media.
- Thompson, James A.; Itskovitz-Eldor, Joseph; Shapiro, Sander S.; Waknitz, Michelle A.; Swiergiel, Jennifer J.; Marshall, Vivienne S.; Jones, Jeffrey M. (6 November 1998). "Embryonic Stem Cell Lines Derived From Human Blastocyst". Science. 282 (5391): 1145–1147. Bibcode:1998Sci...282.1145T. doi:10.1126/science.282.5391.1145. PMID 9804556.
- "President George W. Bush's address on stem cell research". CNN Inside Politics. CNN. Aug 9, 2001.
- Yamanaka, Shinya; Takahashi, Kazutoshi (25 Aug 2006). "Induction of Pluripotent Stem Cells From Mouse Embryonic and Adult Fibroblast Cultures by Defined Factors". Cell. 126 (4): 663–676. doi:10.1016/j.cell.2006.07.024. hdl:2433/159777. PMID 16904174.
- Wadman, Meredith (27 January 2009). "Stem cells ready for primetime". Nature. 457 (7229): 516. doi:10.1038/457516a. PMID 19177087.
- "Executive Order 13505—Removing Barriers To Responsible Scientific Research Involving Human Stem Cells" (PDF). Federal Register: Presidential Documents. 74 (46). 11 March 2009.
- Mountford, JC (2008). "Human embryonic stem cells: origins, characteristics and potential for regenerative therapy". Transfus Med. 18 (1): 1–12. doi:10.1111/j.1365-3148.2007.00807.x. PMID 18279188.
- Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, Jones JM (1998). "Embryonic stem cell lines derived from human blastocysts". Science. 282 (5391): 1145–1147. Bibcode:1998Sci...282.1145T. doi:10.1126/science.282.5391.1145. PMID 9804556.
- Smith AG, Heath JK, Donaldson DD, Wong GG, Moreau J, Stahl M, Rogers D (1988). "Inhibition of pluripotential embryonic stem cell differentiation by purified polypeptides". Nature. 336 (6200): 688–690. Bibcode:1988Natur.336..688S. doi:10.1038/336688a0. PMID 3143917.
- Williams RL, Hilton DJ, Pease S, Willson TA, Stewart CL, Gearing DP, Wagner EF, Metcalf D, Nicola NA, Gough NM (1988). "Myeloid leukaemia inhibitory factor maintains the developmental potential of embryonic stem cells". Nature. 336 (6200): 684–687. Bibcode:1988Natur.336..684W. doi:10.1038/336684a0. PMID 3143916.
- Ledermann B, Bürki K (1991). "Establishment of a germ-line competent C57BL/6 embryonic stem cell line". Exp Cell Res. 197 (2): 254–258. doi:10.1016/0014-4827(91)90430-3. PMID 1959560.
- Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, Yamanaka S (2007). "Induction of pluripotent stem cells from adult human fibroblasts by defined factors". Cell. 131 (5): 861–872. doi:10.1016/j.cell.2007.11.019. hdl:2433/49782. PMID 18035408.
- Klimanskaya I, Chung Y, Becker S, Lu SJ, Lanza R (2006). "Human embryonic stem cell lines derived from single blastomeres". Nature. 444 (7118): 481–5. Bibcode:2006Natur.444..481K. doi:10.1038/nature05142. PMID 16929302.
- US scientists relieved as Obama lifts ban on stem cell research, The Guardian, 10 March 2009
- Takahashi, K; Yamanaka, S (2006). "Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors". Cell. 126 (4): 663–76. doi:10.1016/j.cell.2006.07.024. hdl:2433/159777. PMID 16904174.

- "The Nobel Prize in Physiology or Medicine – 2012 Press Release". Nobel Media AB. 8 October 2012.
- Wernig, Marius; Meissner, Alexander; Foreman, Ruth; Brambrink, Tobias; Ku, Manching; Hochedlinger, Konrad; Bernstein, Bradley E.; Jaenisch, Rudolf (2007-07-19). "In vitro reprogramming of fibroblasts into a pluripotent ES-cell-like state". Nature. 448 (7151): 318–324. Bibcode:2007Natur.448..318W. doi:10.1038/nature05944. ISSN 1476-4687. PMID 17554336.
- "Embryonic stem cells made without embryos". Reuters. 2007-11-21.
- Weiss, Rick (2007-12-07). "Scientists Cure Mice Of Sickle Cell Using Stem Cell Technique: New Approach Is From Skin, Not Embryos". The Washington Post. pp. A02.
- Hanna, J.; Wernig, M.; Markoulaki, S.; Sun, C.-W.; Meissner, A.; Cassady, J. P.; Beard, C.; Brambrink, T.; Wu, L.-C.; Townes, T. M.; Jaenisch, R. (2007). "Treatment of Sickle Cell Anemia Mouse Model with iPS Cells Generated from Autologous Skin". Science. 318 (5858): 1920–3. Bibcode:2007Sci...318.1920H. doi:10.1126/science.1152092. PMID 18063756.
- Helen Briggs (2008-01-17). "US team makes embryo clone of men". BBC. pp. A01.
- Ebert, Jessica (24 January 2005). "Human stem cells trigger immune attack". Nature News. London: Nature Publishing Group. doi:10.1038/news050124-1. Archived from the original on 2010-09-24. Retrieved 2009-02-27.
- Martin MJ, Muotri A, Gage F, Varki A (2005). "Human embryonic stem cells express an immunogenic nonhuman sialic acid". Nat. Med. 11 (2): 228–32. doi:10.1038/nm1181. PMID 15685172.
- Klimanskaya I, Chung Y, Meisner L, Johnson J, West MD, Lanza R (2005). "Human embryonic stem cells derived without feeder cells". Lancet. 365 (9471): 1636–41. doi:10.1016/S0140-6736(05)66473-2. PMID 15885296.
External links
| Wikimedia Commons has media related to Embryonic stem cells. |
- Understanding Stem Cells: A View of the Science and Issues from the National Academies
- National Institutes of Health
- University of Oxford practical workshop on pluripotent stem cell technology
- Fact sheet on embryonic stem cells
- Fact sheet on ethical issues in embryonic stem cell research
- Information & Alternatives to Embryonic Stem Cell Research
- A blog focusing specifically on ES cells and iPS cells including research, biotech, and patient-oriented issues