Gingival grafting
Gingival grafting, also called gum grafting or periodontal plastic surgery,[1][2][3] is a generic term for the performance of any of a number of periodontal surgical procedures in which the gum tissue is grafted. The aim may be to cover exposed root surfaces or merely to augment the band of keratinized tissue.
| Gingival graft | |
|---|---|
 | |
| ICD-9-CM | 24.2-24.3 |
Anatomy
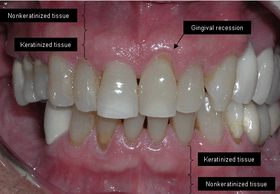
The soft tissue in the oral cavity is classified as either keratinized or nonkeratinized based on the presence of keratin in the epithelium. In health, the soft tissue immediately around the teeth is keratinized and is referred to as keratinized tissue or gingiva. Alveolar mucosa is non keratinized oral epithelium and is located apical to the keratinized tissue, delineated by the mucogingival junction (MGJ). It should also be pointed out that mucosa can surround a tooth in health. (Dorfman and Kennedy et al.) Nonkeratinized tissue also lines the cheeks (buccal mucosa), underside of the tongue and floor of the mouth. The lips contain both non-keratinized tissue (on the inside) and keratinized tissue on the outside, demarcated by the vermillion border. The dorsum of the tongue is keratinized and features many papillae, some of which contain taste buds.
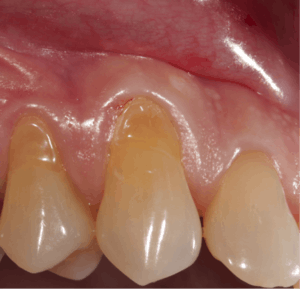
Exposure of the tooth root due to loss of keratinized tissue around the neck of a tooth is referred to as gingival recession. This can result in sensitivity or pain from the exposed tooth root surface (dentin is more permeable and soft compared to enamel and dentin is what makes up the tooth root). Recession may also cause there to be an unasthetic appearance especially if located in the anterior dentition (front teeth). While not all cases of gingival recession require surgical correction, there are various options if that is what the patient desires. It should be reinforced that recession left untreated will not result in tooth loss, contrary to popular belief. Also, recession that is left untreated can be maintained and the inflammation kept at bay with proper brushing and oral hygiene technique (Kennedy and Dorfman et al.) On the other hand, if one desires to pursue corrective therapy, there are a wide variety of techniques ranging from autograft (your own tissue, usually taken from the palate), allograft (someone else's tissue, cadaver), xenograft (animal, usually porcine or bovine) or simply repositioning of the tissue native to the site. The benefits of corrective therapy often result in decreased sensitivity through coverage of the root surface in addition to a gain in the keratinized tissue mentioned beforehand.
Rationale
Gum grafting, also known as a gingival graft or periodontal plastic surgery, is a surgical procedure to reverse gum recession. Gum recession exposes the roots of teeth,[4] which can lead to sensitivity and put teeth at a higher risk of damage or disease[5] due to the loosening of their attachment within the gums and bones of the jaw. Should gum recession continue, bone and keratinized tissue will be at greater risk of being damaged and permanently lost around the teeth. The aim of a gum graft is to extend keratinized tissue of the gums to cover tooth roots,[6] which restores their firm placement within the jaw and prevents further damage.
Options in gum grafting
Traditional gum grafting will have a piece of the gums harvested from the roof of the mouth and sutured facing the exposed root to increase the lost keratinized tissue.[6] The limitation in quantity and the morbidity are the limiting factor of this technique. Allografting techniques (skin from cadavers bought from tissue banks) are used as well to supply the surgeon with larger amount of tissues when needed in larger cases,[7] but the type of healing and the risk of possible disease transmission should be considered and disclosed to the patient when opting for such technique.
Advantages of APRF in gum grafting
Blood-derived growth factors have been used in medicine and oral surgery for more than twenty years with an abundance of scientific data supporting its role in soft and hard tissue regenerations. APRF introduced by Dr. Choukroun represents the fourth improved generation of such technology and has been widely used in the field of dentistry and oral surgery. The advantages of APRF are of multiple folds: Unlimited amount (only 10 millilitres (0.35 imp fl oz; 0.34 US fl oz) per tube harvested), no risk of rejection or disease transmission (using your own blood), high noble type of healing (autogenous growth factors and hematopoietic stem cells).
Technique

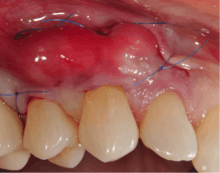
A small amount of blood (10 millilitres (0.35 imp fl oz; 0.34 US fl oz) per tube) is harvested and spun in a centrifuge for eight minutes at 1300 rpm. A fibrin clot packed with blood-derived growth factors, extra cellular matrix and hematopoietic stem cells is fabricated and implanted into the gums above the area of gum recession. Advanced platelet-rich fibrin will promote the patient's own gums to fabricate more gum thus eliminating the need to harvest gums from the roof of the mouth or the use of allografting tissue.

Following this procedure, patients have an improved quality of recovery and require less recovery time due to enhanced healing factors.[8][9][10][11]
Specific procedures
Coronally and apically positioned flaps, although technically not grafting procedures, are other forms of a pedicle grafts in that gingival tissue is freed up and moved either coronally or apically. This requires adequate thickness and width of gingival tissue at the base of the recession defect.
A free gingival graft is a dental procedure where a small layer of tissue is removed from the palate of the patient's mouth and then relocated to the site of gum recession. It is sutured (stitched) into place and will serve to protect the exposed root as living tissue. The donor site will heal over a period of time without damage. This procedure is often used to increase the thickness of very thin gum tissue.
A subepithelial connective tissue graft takes tissue from under healthy gum tissue in the palate, which may be placed at the area of gum recession. This procedure has the advantage of excellent predictability of root coverage,[12] as well as decreased pain at the palatal donor site compared to the free gingival graft. The subepithelial connective tissue graft is a very common procedure for covering exposed roots.
A lateral pedicle graft, or pedicle graft, takes tissue from the area immediately adjacent to the damaged gingiva. This is not always an option, as the constraint that there must be sufficient tissue immediately lateral to the area of interest is an onerous one. When this procedure is performed, the transplant tissue is cut away and rotated over the damaged area. This can place the donor area at risk of recession as well.
An acellular dermal matrix (such as Alloderm) graft uses donated medically processed human skin tissue as a source for the graft. The advantage of this procedure is no need for a palatal donor site, and though some periodontists consider it equally successful as a subepithelial connective tissue graft,[13] others consider it less successful.[14]
Guided bone reconstruction is a technique in which bone growth is enhanced by preventing soft tissue ingrowth into the desired area and utilizes either resorbable or nonresorbable membranes. Metallic membranes[15] or membranes supported by a titanium frame[16] have been tested and have been successful. The acellular dermal matrix has been used as a barrier membrane with demineralized freeze-dried bone allograft.
Through the advent of micro-surgical procedures these procedures have become more predictable and comfortable for the patients. Gum grafts are usually performed by periodontists who are trained in these procedures, though general-purpose dentists may offer the procedures themselves. Outcome comparisons between both are highly variable, though with periodontists being specially-trained, periodontists generally recommend patients seeking their services over general-practice dentists.
References
- "Receding Gums Chandler, Gum Graft Tempe, Gingival Grafting Phoenix". Scholesperio.com. Retrieved 2015-12-12.
- Archived February 10, 2009, at the Wayback Machine
- Archived January 5, 2010, at the Wayback Machine
- "Receding Gums: Causes, Treatment, Surgery, and Prevention". Webmd.com. Retrieved 2015-12-12.
- "Gum Recession Treatment Los Angeles". Implant Perio Center. Retrieved 2015-12-12.
- "Gum Tissue Graft Surgery: Procedure, Recovery, Complications, and More". Webmd.com. Retrieved 2015-12-12.
- "Allograft definition – MedicineNet – Health and Medical Information Produced by Doctors". MedicineNet.vom. 2012-03-19. Retrieved 2015-12-12.
- "RejuvaGum Lift with Dr. Aalam and Dr. Krivitsky | KABC 7 EYEWITNESS NEWS | Los Angeles". YouTube. Retrieved 2015-12-12.
- Jankovic S, Aleksic Z, Klokkevold P, Lekovic V, Dimitrijevic B, Kenney EB, Camargo P (2012). "Use of platelet-rich fibrin membrane following treatment of gingival recession: a randomized clinical trial". The International Journal of Periodontics & Restorative Dentistry. 32 (2): e41–50. PMID 22292152.
- "RejuvaGum Lift Gum Recession Los Angeles | Implant PerioCent". Implantperiocenter.com. Retrieved 2015-12-12.
- Sunitha Raja V, Munirathnam Naidu E (2008). "Platelet-rich fibrin: evolution of a second-generation platelet concentrate". Indian Journal of Dental Research. 19 (1): 42–6. doi:10.4103/0970-9290.38931. PMID 18245923.
- Wennström JL (1996). "Mucogingival therapy". Annals of Periodontology. 1 (1): 671–701. doi:10.1902/annals.1996.1.1.671. PMID 9118276.
- Hirsch A, Goldstein M, Goultschin J, Boyan BD, Schwartz Z (2005). "A 2-year follow-up of root coverage using sub-pedicle acellular dermal matrix allografts and subepithelial connective tissue autografts". Journal of Periodontology. 76 (8): 1323–8. doi:10.1902/jop.2005.76.8.1323. PMID 16101365.
- Harris RJ (2004). "A short-term and long-term comparison of root coverage with an acellular dermal matrix and a subepithelial graft". Journal of Periodontology. 75 (5): 734–43. doi:10.1902/jop.2004.75.5.734. PMID 15212356.
- von Arx T, Hardt N, Wallkamm B (1996). "The TIME technique: a new method for localized alveolar ridge augmentation prior to placement of dental implants". The International Journal of Oral & Maxillofacial Implants. 11 (3): 387–94. PMID 8752560.
- Simion et al. 1994, 1998, 2001