Concussion
Concussion, also known as mild traumatic brain injury (mTBI), is a head injury that temporarily affects brain functioning.[8] Symptoms may include loss of consciousness (LOC); memory loss; headaches; difficulty with thinking, concentration or balance; nausea; blurred vision; sleep disturbances; and mood changes.[1] Any of these symptoms may begin immediately, or appear days after the injury.[1] Concussion should be suspected if a person indirectly or directly hits their head and experiences any of the symptoms of concussion.[9] It is not unusual for symptoms to last 2 weeks in adults and 4 weeks in children.[10][2] Fewer than 10% of sports-related concussions among children are associated with loss of consciousness.[11]
| Concussion | |
|---|---|
| Other names | Mild brain injury, mild traumatic brain injury (mTBI), mild head injury (MHI), minor head trauma |
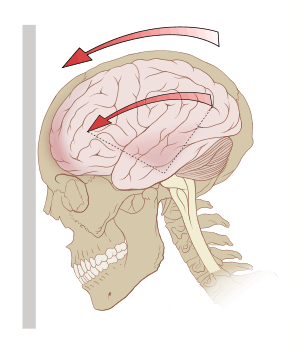 | |
| Acceleration (g-forces) can exert rotational forces in the brain, especially the midbrain and diencephalon. | |
| Specialty | Emergency medicine, neurology |
| Symptoms | Headache, trouble with thinking, memory or concentration, nausea, blurry vision, sleep disturbances, mood changes[1] |
| Duration | Up to 4 weeks[2] |
| Causes | Motor vehicle collisions, falls, sports injuries, bicycle accidents[3][4] |
| Risk factors | Drinking alcohol[5] |
| Diagnostic method | Based on symptoms[6] |
| Prevention | Helmets when bicycling or motorbiking[3] |
| Treatment | Physical and cognitive rest for a day or two with a gradual return to activities[7][2] |
| Medication | Paracetamol (acetaminophen), NSAIDs[2] |
| Frequency | 6 per 1,000 people a year[3] |
Common causes include motor vehicle collisions, falls, sports injuries, and bicycle accidents.[3][4] Risk factors include drinking alcohol and a prior history of concussion.[10][5] The mechanism of injury involves either a direct blow to the head or forces elsewhere on the body that are transmitted to the head.[10] This is believed to result in neuron dysfunction, as there is increased glucose requirements but not enough blood supply.[2] A full differential diagnosis by a physician or nurse practitioner is required to rule out life threatening head injuries, injuries to the cervical spine, and neurological conditions.[6][12] Glasgow coma scale score 13 to 15, loss of consciousness for less than 30 minutes, and memory loss for less than 24 hours may be used to rule out moderate or severe traumatic brain injuries.[6] Diagnostic imaging such as a CT scan or an MRI may also be required to rule out severe head injuries.[12] Routine imaging is not required to diagnose concussion.[13]
Prevention of concussions includes the use of a helmet when bicycling or motorbiking.[3] Treatment includes physical and cognitive rest for 1-2 days, with a gradual step-wise return to activities, school, and work.[7][2][14] Prolonged periods of rest may slow recovery and result in greater depression and anxiety.[2] Paracetamol (acetaminophen) or NSAIDs may be recommended to help with a headache.[2] Physiotherapy may be useful for persistent balance problems; cognitive behavioral therapy may be useful for mood changes.[2] Evidence to support the use of hyperbaric oxygen therapy and chiropractic therapy is lacking.[2]
Worldwide, concussions are estimated to affect more than 3.5 per 1,000 people a year.[15] Concussions are classified as mild traumatic brain injuries and are the most common type of TBIs.[3][15] Males and young adults are most commonly affected.[3][15] Outcomes are generally good.[16] Another concussion before the symptoms of a prior concussion have resolved is associated with worse outcomes.[17][18] Repeated concussions may also increase the risk in later life of chronic traumatic encephalopathy, Parkinson's disease and depression.[19]
Signs and symptoms
Concussions symptoms vary between people and include physical, cognitive, and emotional symptoms.[9] Symptoms may appear immediately or be delayed.[9] Up to one-third of people with concussion experience prolonged or persistent concussion symptoms, also known as post concussion syndrome, which is defined as concussion symptoms lasting for 4-weeks or longer in children/adolescents and symptoms lasting for more than 14 days in an adult.[12][10] The severity of the initial symptoms is the strongest predictor of recovery time in adults.[10]
Physical
Headaches are the most common mTBI symptom.[21] Others include dizziness, vomiting, nausea, lack of motor coordination, difficulty balancing,[21] or other problems with movement or sensation. Visual symptoms include light sensitivity,[22] seeing bright lights,[23] blurred vision,[24] and double vision.[25] Tinnitus, or a ringing in the ears, is also commonly reported.[24] In one in about seventy concussions, concussive convulsions occur, but seizures that take place during or immediately after a concussion are not "post-traumatic seizures", and, unlike post-traumatic seizures, are not predictive of post-traumatic epilepsy, which requires some form of structural brain damage, not just a momentary disruption in normal brain functioning.[26] Concussive convulsions are thought to result from temporary loss or inhibition of motor function and are not associated either with epilepsy or with more serious structural damage. They are not associated with any particular sequelae and have the same high rate of favorable outcomes as concussions without convulsions.[27]
Cognitive and emotional
Cognitive symptoms include confusion, disorientation, and difficulty focusing attention. Loss of consciousness may occur, but is not necessarily correlated with the severity of the concussion if it is brief.[28] Post-traumatic amnesia, in which events following the injury cannot be recalled, is a hallmark of concussions.[21] Confusion, another concussion hallmark, may be present immediately or may develop over several minutes.[21] A person may repeat the same questions,[29] be slow to respond to questions or directions, have a vacant stare, or have slurred[21] or incoherent speech.[30] Other mTBI symptoms include changes in sleeping patterns[24] and difficulty with reasoning,[25] concentrating, and performing everyday activities.[21]
A concussion can result in changes in mood including crankiness, loss of interest in favorite activities or items,[31] tearfulness,[32] and displays of emotion that are inappropriate to the situation.[30] Common symptoms in concussed children include restlessness, lethargy, and irritability.[33]
Mechanism
Forces
The brain is surrounded by cerebrospinal fluid, which protects it from light trauma. More severe impacts, or the forces associated with rapid acceleration, may not be absorbed by this cushion.[35] Concussion may be caused by impact forces, in which the head strikes or is struck by something, or impulsive forces, in which the head moves without itself being subject to blunt trauma (for example, when the chest hits something and the head snaps forward).[32]
Forces may cause linear, rotational, or angular movement of the brain or a combination of them.[32] In rotational movement, the head turns around its center of gravity and in angular movement, it turns on an axis, not through its center of gravity.[32] The amount of rotational force is thought to be the major component in concussion[36] and its severity.[37] Studies with athletes have shown that the amount of force and the location of the impact are not necessarily correlated with the severity of the concussion or its symptoms, and have called into question the threshold for concussion previously thought to exist at around 70–75 g.[38][39]
The parts of the brain most affected by rotational forces are the midbrain and diencephalon.[40][4] It is thought that the forces from the injury disrupt the normal cellular activities in the reticular activating system located in these areas and that this disruption produces the loss of consciousness often seen in concussion.[4] Other areas of the brain that may be affected include the upper part of the brain stem, the fornix, the corpus callosum, the temporal lobe, and the frontal lobe.[41] Angular accelerations of 4600, 5900, or 7900 rad/s2 are estimated to have 25, 50, or 80% risk of mTBI respectively.[42]
Pathophysiology
In both animals and humans, mTBI can alter the brain's physiology for hours to years,[43][44] setting into motion a variety of pathological events.[45] As one example, in animal models, after an initial increase in glucose metabolism, there is a subsequent reduced metabolic state which may persist for up to four weeks after injury.[11] Though these events are thought to interfere with neuronal and brain function, the metabolic processes that follow concussion are reversible in a large majority of affected brain cells; however, a few cells may die after the injury.[46]
Included in the cascade of events unleashed in the brain by concussion is impaired neurotransmission, loss of regulation of ions, deregulation of energy use and cellular metabolism, and a reduction in cerebral blood flow.[46] Excitatory neurotransmitters, chemicals such as glutamate that serve to stimulate nerve cells, are released in excessive amounts.[47] The resulting cellular excitation causes neurons to fire excessively.[48] This creates an imbalance of ions such as potassium and calcium across the cell membranes of neurons (a process like excitotoxicity).[46]
At the same time, cerebral blood flow is relatively reduced for unknown reasons,[22] though the reduction in blood flow is not as severe as it is in ischemia.[46] Thus cells get less glucose than they normally do, which causes an "energy crisis".[22]
Concurrently with these processes, the activity of mitochondria may be reduced, which causes cells to rely on anaerobic metabolism to produce energy, increasing levels of the byproduct lactate.[46]
For a period of minutes to days after a concussion, the brain is especially vulnerable to changes in intracranial pressure, blood flow, and anoxia.[22] According to studies performed on animals (which are not always applicable to humans), large numbers of neurons can die during this period in response to slight, normally innocuous changes in blood flow.[22]
Concussion involves diffuse (as opposed to focal) brain injury, meaning that the dysfunction occurs over a widespread area of the brain rather than in a particular spot.[49] It is thought to be a milder type of diffuse axonal injury, because axons may be injured to a minor extent due to stretching.[32] Animal studies in which rodents were concussed have revealed lifelong neuropathological consequences such as ongoing axonal degeneration and neuroinflammation in subcortical white matter tracts.[50] Axonal damage has been found in the brains of concussion sufferers who died from other causes, but inadequate blood flow to the brain due to other injuries may have contributed.[24] Findings from a study of the brains of deceased NFL athletes who received concussions suggest that lasting damage is done by such injuries. This damage, the severity of which increases with the cumulative number of concussions sustained, can lead to a variety of other health issues.[51]
The debate over whether concussion is a functional or structural phenomenon is ongoing.[52] Structural damage has been found in the mildly traumatically injured brains of animals, but it is not clear whether these findings would apply to humans.[40] Such changes in brain structure could be responsible for certain symptoms such as visual disturbances, but other sets of symptoms, especially those of a psychological nature, are more likely to be caused by reversible pathophysiological changes in cellular function that occur after concussion, such as alterations in neurons' biochemistry.[37] These reversible changes could also explain why dysfunction is frequently temporary.[52] A task force of head injury experts called the Concussion In Sport Group met in 2001 and decided that "concussion may result in neuropathological changes but the acute clinical symptoms largely reflect a functional disturbance rather than structural injury."[53]
Using animal studies, the pathology of a concussion seems to start with mechanical shearing and stretching forces disrupting the cell membrane of nerve cells through "mechanoporation".[54] This results in potassium outflow from within the cell into the extracellular space with the subsequent release of excitatory neurotransmitters including glutamate which leads to enhanced potassium extrusion, in turn resulting in sustained depolarization, impaired nerve activity and potential nerve damage.[54] Human studies have failed to identify changes in glutamate concentration immediately post-mTBI, though disruptions have been seen 3 days to 2 weeks post-injury.[54] In an effort to restore ion balance, the sodium-potassium ion pumps increase activity, which results in excessive ATP (adenosine triphosphate) consumption and glucose utilization, quickly depleting glucose stores within the cells.[55] Simultaneously, inefficient oxidative metabolism leads to anaerobic metabolism of glucose and increased lactate accumulation.[55] There is a resultant local acidosis in the brain and increased cell membrane permeability, leading to local swelling.[55] After this increase in glucose metabolism, there is a subsequent lower metabolic state which may persist for up to 4 weeks after injury. A completely separate pathway involves a large amount of calcium accumulating in cells, which may impair oxidative metabolism and begin further biochemical pathways that result in cell death. Again, both of these main pathways have been established from animal studies and the extent to which they apply to humans is still somewhat unclear.[11]
Diagnosis
| Red flag[56] |
|---|
| Seizure |
| Worsening headache |
| Difficulty waking up |
| Seeing double |
| Problem recognizing people or places |
| Repeated vomiting |
| Focal neurological problems |
| Not usual self |
Head trauma recipients are initially assessed to exclude a more severe emergency such as an intracranial hemorrhage. This includes the "ABCs" (airway, breathing, circulation) and stabilization of the cervical spine which is assumed to be injured in any athlete who is found to be unconscious after head or neck injury. Indications that screening for more serious injury is needed include worsening of symptoms such as headaches, persistent vomiting,[57] increasing disorientation or a deteriorating level of consciousness,[58] seizures, and unequal pupil size.[59] Those with such symptoms, or those who are at higher risk of a more serious brain injury, may undergo brain imaging to detect lesions and are frequently observed for 24–48 hours. A brain CT or brain MRI should be avoided unless there are progressive neurological symptoms, focal neurological findings or concern of skull fracture on exam.[60]
Diagnosis of concussion requires an assessment performed by a physician or nurse practitioner to rule out severe injuries to the brain and cervical spine, mental health conditions, or other medical conditions.[12] Diagnosis is based on physical and neurological examination findings, duration of unconsciousness (usually less than 30 minutes) and post-traumatic amnesia (PTA; usually less than 24 hours), and the Glasgow Coma Scale (mTBI sufferers have scores of 13 to 15).[61] A CT scan or MRI is not required to diagnose concussion.[12] Neuropsychological tests such as the SCAT5/child SCAT5 may be suggested measure cognitive function.[10][62][63] Such tests may be administered hours, days, or weeks after the injury, or at different times to demonstrate any trend.[64] Some athletes are also being tested pre-season (pre-season baseline testing) to provide a baseline for comparison in the event of an injury, though this may not reduce risk or affect return to play and baseline testing is not required or suggested for most children and adults.[65][66]
If the Glasgow coma scale is less than 15 at two hours or less than 14 at any time, a CT is recommended.[4] In addition, a CT scan is more likely to be performed if observation after discharge is not assured or intoxication is present, there is suspected increased risk for bleeding, age greater than 60,[4] or less than 16. Most concussions, without complication, cannot be detected with MRI or CT scans.[36] However, changes have been reported on MRI and SPECT imaging in those with concussion and normal CT scans, and post-concussion syndrome may be associated with abnormalities visible on SPECT and PET scans.[46] Mild head injury may or may not produce abnormal EEG readings.[67] A blood test known as the Brain Trauma Indicator was approved in the United States in 2018 and may be able to rule out the risk of intracranial bleeding and thus the need for a CT scan for adults.[68]
Concussion may be under-diagnosed because of the lack of the highly noticeable signs and symptoms while athletes may minimize their injuries to remain in the competition.[69] A retrospective survey in 2005 suggested that more than 88% of concussions are unrecognized.[70]
Diagnosis can be complex because concussion shares symptoms with other conditions. For example, post-concussion symptoms such as cognitive problems may be misattributed to brain injury when, in fact, due to post-traumatic stress disorder (PTSD).[71]
There are no fluid biomarkers (i.e., blood or urine tests) that are validated for diagnosing concussion in children or adolescents.[72]
Classification
No single definition of concussion, minor head injury,[73] or mild traumatic brain injury is universally accepted.[74] In 2001, the expert Concussion in Sport Group of the first International Symposium on Concussion in Sport[53] defined concussion as "a complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces."[28] It was agreed that concussion typically involves temporary impairment of neurological function that heals by itself within time, and that neuroimaging normally shows no gross structural changes to the brain as the result of the condition.[37]
However, although no structural brain damage occurs according to the classic definition,[75] some researchers have included injuries in which structural damage has occurred and the National Institute for Health and Clinical Excellence definition includes physiological or physical disruption in the brain's synapses.[76] Also, by definition, concussion has historically involved a loss of consciousness. However, the definition has evolved over time to include a change in consciousness, such as amnesia,[77] although controversy continues about whether the definition should include only those injuries in which loss of consciousness occurs.[40] This debate resurfaces in some of the best-known concussion grading scales, in which those episodes involving loss of consciousness are graded as being more severe than those without.[78]
Definitions of mild traumatic brain injury (mTBI) were inconsistent until the World Health Organization's International Statistical Classification of Diseases and Related Health Problems (ICD-10) provided a consistent, authoritative definition across specialties in 1992.[79] Since then, various organizations such as the American Congress of Rehabilitation Medicine[21] and the American Psychiatric Association in its Diagnostic and Statistical Manual of Mental Disorders[79] have defined mTBI using some combination of loss of consciousness (LOC), post-traumatic amnesia (PTA), and the Glasgow Coma Scale (GCS).
Concussion falls under the classification of mild TBI,[80] but it is not clear whether concussion is implied in mild brain injury or mild head injury.[81] "mTBI" and "concussion" are often treated as synonyms in medical literature[21] but other injuries such as intracranial hemorrhages (e.g. intra-axial hematoma, epidural hematoma, and subdural hematoma) are not necessarily precluded in mTBI[37] or mild head injury,[82][83] as they are in concussion.[84] mTBI associated with abnormal neuroimaging may be considered "complicated mTBI".[46] "Concussion" can be considered to imply a state in which brain function is temporarily impaired and "mTBI" to imply a pathophysiological state, but in practice, few researchers and clinicians distinguish between the terms.[37] Descriptions of the condition, including the severity and the area of the brain affected, are now used more often than "concussion" in clinical neurology.[85]
Prevention
Prevention of mTBI involves general measures such as wearing seat belts, using airbags in cars, and protective equipment such as helmets for high-risk sports.[21][86] Older people are encouraged to reduce fall risk by keeping floors free of clutter and wearing thin, flat, shoes with hard soles that do not interfere with balance.[31]
Protective equipment such as helmets and other headgear and policy changes such as the banning of body checking in youth hockey leagues have been found to reduce the number and severity of concussions in athletes.[87] Secondary prevention such as a Return to Play Protocol for an athlete may reduce the risk of repeat concussions.[88] New "Head Impact Telemetry System" technology is being placed in helmets to study injury mechanisms and may generate knowledge that will potentially help reduce the risk of concussions among American Football players.
Educational interventions, such as handouts, videos, workshops, and lectures, can improve concussion knowledge of diverse groups, particularly youth athletes and coaches.[89] Strong concussion knowledge may be associated with greater recognition of concussion symptoms, higher rates of concussion reporting behaviors, and reduced body checking-related penalties and injuries, thereby lowering risk of mTBI.[89]
Self-reported concussion rates among U-20 and elite rugby union players in Ireland are 45–48%.[34] Half of these injuries go unreported. Changes to the rules or enforcing existing rules in sports, such as those against "head-down tackling", or "spearing", which is associated with a high injury rate, may also prevent concussions.[34]
Treatment
After exclusion of neck or head injury, observation should be continued for several hours. If repeated vomiting, worsening headache, dizziness, seizure activity, excessive drowsiness, double vision, slurred speech, unsteady walk, or weakness or numbness in arms or legs, or signs of basilar skull fracture develop, immediate assessment in an emergency department is needed.[90][11] Observation to monitor for worsening condition is an important part of treatment.[12] People may be released after assessment from hospital or emergency room to the care of a trusted person with instructions to return if they display worsening symptoms or those that might indicate an emergent condition ("red flag symptoms") such as change in consciousness, convulsions, severe headache, extremity weakness, vomiting, new bleeding or deafness in either or both ears.[91][56][12] Education about symptoms, their management, and their normal time course, may lead to an improved outcome.[74]
Rest and return to physical and cognitive activity
Physical and cognitive rest is recommended for the first 24-48 hours following a concussion after which injured persons should gradually start gentle low-risk physical and cognitive activities that do not make current symptoms worse or bring on new symptoms.[10][92] Any activity for which there is a risk of contact, falling, or bumping the head should be avoided.[10] Low-risk activities can be started even while a person has symptoms, as long as the activity does not worsen existing symptoms or bring on new concussion symptoms.[56][13]
Return-to-school
The resumption of low-risk school activities should begin as soon as the student feels well enough. The return to school should be gradual and step-wise.[93] Since students may appear 'normal', continuing education of relevant school personnel may be needed.[11]
Return-to-sport
For persons participating in athletics, the 2016 Berlin Consensus Statement on Concussion in Sport recommends that participants progress through a series of graded steps after an initial 24-48h of relative physical and cognitive rest.[10] These steps include:
- Symptom-limited activity
- Light aerobic activity such as walking or stationary cycling
- Sport-specific activities such as running drills and skating drills
- Non-contact training drills (exercise, coordination, and cognitive load)
- Full-contact practice
- Return to sport (requires medical clearance)
Each step should last at least 24 hours before progression to the next. If symptoms worsen, athletes should drop back to the previous asymptomatic level for at least another 24 hours.[10] Athletes, especially intercollegiate or professional, are typically followed closely by team athletic trainers during this period but others may not have access to this level of health care and may be sent home with minimal monitoring.
Medications
Medications may be prescribed to treat sleep problems and depression.[74] Analgesics such as ibuprofen can be taken for headaches,[37] but paracetamol (acetaminophen) is preferred to minimize the risk of intracranial hemorrhage.[94] Concussed individuals are advised not to use alcohol or other drugs that have not been approved by a doctor as they can impede healing.[95] Activation database-guided EEG biofeedback has been shown to return the memory abilities of the concussed individual to levels better than the control group.[96]
About one percent of people who receive treatment for mTBI need surgery for a brain injury.[61]
Prognosis
People who have had a concussion seem more susceptible to another one, particularly if the new injury occurs before symptoms from the previous concussion have completely gone away.[19] It is also a negative process if smaller impacts cause the same symptom severity.[90] Repeated concussions may increase a person's risk in later life for dementia, Parkinson's disease, and depression.[19]
mTBI has a mortality rate of almost zero.[61] The symptoms of most concussions resolve within weeks, but problems may persist.[37] These are seldom permanent, and the outcome is usually excellent.[46] About 75% of children recover within three months.[97]
The overall prognosis for recovery may be influenced by a variety of factors that include age at the time of injury, intellectual abilities, family environment, social support system, occupational status, coping strategies, and financial circumstances.[98] People over age 55 may take longer to heal from mTBI or may heal incompletely.[99] Similarly, factors such as a previous head injury or a coexisting medical condition have been found to predict longer-lasting post-concussion symptoms.[100] Other factors that may lengthen recovery time after mTBI include psychological problems such as substance abuse or clinical depression, poor health before the injury or additional injuries sustained during it, and life stress.[46] Longer periods of amnesia or loss of consciousness immediately after the injury may indicate longer recovery times from residual symptoms.[101] For unknown reasons, having had one concussion significantly increases a person's risk of having another.[64] Having previously sustained a sports concussion has been found to be a strong factor increasing the likelihood of a concussion in the future. Other strong factors include participation in a contact sport and body mass size.[102] The prognosis may differ between concussed adults and children; little research has been done on concussion in the pediatric population, but concern exists that severe concussions could interfere with brain development in children.[64]
Post-concussion syndrome
In post-concussion syndrome, symptoms do not resolve for weeks, months, or years after a concussion, and may occasionally be permanent.[103] About 10% to 20% of people have post-concussion syndrome for more than a month.[104] Symptoms may include headaches, dizziness, fatigue, anxiety, memory and attention problems, sleep problems, and irritability.[105] There is no established treatment, and rest, a recommended recovery technique, has limited effectiveness.[106] Symptoms usually go away on their own within months[84] but may last for years.[107][108] The question of whether the syndrome is due to structural damage or other factors such as psychological ones, or a combination of these, has long been the subject of debate.[71]
Cumulative effects
Cumulative effects of concussions are poorly understood, especially the effects on children. The severity of concussions and their symptoms may worsen with successive injuries, even if a subsequent injury occurs months or years after an initial one.[109] Symptoms may be more severe and changes in neurophysiology can occur with the third and subsequent concussions.[64] Studies have had conflicting findings on whether athletes have longer recovery times after repeat concussions and whether cumulative effects such as impairment in cognition and memory occur.[34]
Cumulative effects may include psychiatric disorders and loss of long-term memory. For example, the risk of developing clinical depression has been found to be significantly greater for retired American football players with a history of three or more concussions than for those with no concussion history.[110] Three or more concussions is also associated with a fivefold greater chance of developing Alzheimer's disease earlier and a threefold greater chance of developing memory deficits.[110]
CTE
Chronic traumatic encephalopathy, or "CTE", is an example of the cumulative damage that can occur as the result of multiple concussions or less severe blows to the head. The condition was previously referred to as "dementia pugilistica", or "punch drunk" syndrome, as it was first noted in boxers. The disease can lead to cognitive and physical handicaps such as parkinsonism, speech and memory problems, slowed mental processing, tremor, depression, and inappropriate behavior.[111] It shares features with Alzheimer's disease.[112]
Second-impact syndrome
Second-impact syndrome, in which the brain swells dangerously after a minor blow, may occur in very rare cases. The condition may develop in people who receive second blow days or weeks after an initial concussion before its symptoms have gone away.[22] No one is certain of the cause of this often fatal complication, but it is commonly thought that the swelling occurs because the brain's arterioles lose the ability to regulate their diameter, causing a loss of control over cerebral blood flow.[64] As the brain swells, intracranial pressure rapidly rises.[57] The brain can herniate, and the brain stem can fail within five minutes.[22] Except in boxing, all cases have occurred in athletes under age 20.[47] Due to the very small number of documented cases, the diagnosis is controversial, and doubt exists about its validity.[113] A 2010 Pediatrics review article stated that there is debate whether the brain swelling is due to two separate hits or to just one hit, but in either case, catastrophic football head injuries are three times more likely in high school athletes than in college athletes.[11]
Epidemiology
Most cases of traumatic brain injury are concussions. A World Health Organization (WHO) study estimated that between 70 and 90% of head injuries that receive treatment are mild.[3] However, due to under reporting and to the widely varying definitions of concussion and mTBI, it is difficult to estimate how common the condition is.[79] Estimates of the incidence of concussion may be artificially low, for example, due to under reporting. At least 25% of mTBI sufferers fail to get assessed by a medical professional.[46] The WHO group reviewed studies on the epidemiology of mTBI and found a hospital treatment rate of 1–3 per 1000 people, but since not all concussions are treated in hospitals, they estimated that the rate per year in the general population is over 6 per 1000 people.[3]
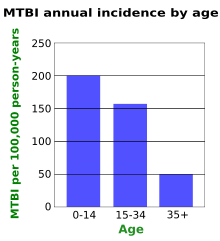
Age
Young children have the highest concussion rate among all age groups.[4] However, most people who suffer a concussion are young adults.[103] A Canadian study found that the yearly incidence of mTBI is lower in older age groups (graph at right).[114] Studies suggest males suffer mTBI at about twice the rate of their female counterparts.[3] However, female athletes may be at a higher risk of suffering a concussion than their male counterparts.[115]
Sports
Up to five percent of sports injuries are concussions.[47] The U.S. Centers for Disease Control and Prevention estimates that 300,000 sports-related concussions occur yearly in the U.S., but that number includes only athletes who lost consciousness.[116] Since loss of consciousness is thought to occur in less than 10% of concussions,[117] the CDC estimate is likely lower than the real number.[116] Sports in which concussion is particularly common include football and boxing (a boxer aims to "knock out", i.e. give a mild traumatic brain injury to, the opponent). The injury is so common in the latter that several medical groups have called for a ban on the sport, including the American Academy of Neurology, the World Medical Association, and the medical associations of the UK, the US, Australia, and Canada.[118]
History
The Hippocratic Corpus, a collection of medical works from ancient Greece, mentions concussion, later translated to commotio cerebri, and discusses loss of speech, hearing and sight that can result from "commotion of the brain".[101] This idea of disruption of mental function by "shaking of the brain" remained the widely accepted understanding of concussion until the 19th century.[101] In the 10th century, the Persian physician Muhammad ibn Zakarīya Rāzi was the first to write about concussion as distinct from other types of head injury.[52] He may have been the first to use the term "cerebral concussion", and his definition of the condition, a transient loss of function with no physical damage, set the stage for the medical understanding of the condition for centuries.[32]
In the 13th century, the physician Lanfranc of Milan's Chiurgia Magna described concussion as brain "commotion", also recognizing a difference between concussion and other types of traumatic brain injury (though many of his contemporaries did not), and discussing the transience of post-concussion symptoms as a result of temporary loss of function from the injury.[52] In the 14th century, the surgeon Guy de Chauliac pointed out the relatively good prognosis of concussion as compared to more severe types of head trauma such as skull fractures and penetrating head trauma.[52] In the 16th-century, the term "concussion" came into use, and symptoms such as confusion, lethargy, and memory problems were described.[52] The 16th century physician Ambroise Paré used the term commotio cerebri,[32] as well as "shaking of the brain", "commotion", and "concussion".[101]

Until the 17th century, a concussion was usually described by its clinical features, but after the invention of the microscope, more physicians began exploring underlying physical and structural mechanisms.[52] However, the prevailing view in the 17th century was that the injury did not result from physical damage, and this view continued to be widely held throughout the 18th century.[52] The word "concussion" was used at the time to describe the state of unconsciousness and other functional problems that resulted from the impact, rather than a physiological condition.[52] In 1839, Guillaume Dupuytren described brain contusions, which involve many small hemorrhages, as contusio cerebri and showed the difference between unconsciousness associated with damage to the brain parenchyma and that due to concussion, without such injury.[101] In 1941, animal experiments showed that no macroscopic damage occurs in concussion.[101][119]
Society and culture
Costs
Due to the lack of a consistent definition, the economic costs of mTBI are not known, but they are estimated to be very high.[120] These high costs are due in part to the large percentage of hospital admissions for head injury that is due to mild head trauma,[81] but indirect costs such as lost work time and early retirement account for the bulk of the costs.[120] These direct and indirect costs cause the expense of mild brain trauma to rival that of moderate and severe head injuries.[121]
Terminology
The terms mild brain injury, mild traumatic brain injury (mTBI), mild head injury (MHI), and concussion may be used interchangeably;[122][79] although the term "concussion" is still used in sports literature as interchangeable with "MHI" or "mTBI", the general clinical medical literature uses "mTBI" instead, since a 2003 CDC report outlined it as an important strategy.[69][32] In this article, "concussion" and "mTBI" are used interchangeably.
The term "concussion" is from Latin concutere, "to shake violently"[40] or concussus, "action of striking together".[123]
Research
Minocycline, lithium, and N-acetylcysteine show tentative success in animal models.[124]
Measurement of predictive visual tracking is being studied as a screening technique to identify mild traumatic brain injury. A head-mounted display unit with eye-tracking capability shows a moving object in a predictive pattern for the person to follow with their eyes. People without brain injury will be able to track the moving object with smooth pursuit eye movements and correct trajectory while it is hypothesized that those with mild traumatic brain injury cannot.[125]
Grading systems
At least 41 systems measure the severity, or grade, of a mild head injury,[37] and there is little agreement about which is best.[23] In an effort to simplify, the 2nd International Conference on Concussion in Sport, meeting in Prague in 2004, decided that these systems should be abandoned in favor of a 'simple' or 'complex' classification.[126] However, the 2008 meeting in Zurich abandoned the simple versus complex terminology, although the participants did agree to keep the concept that most (80–90%) concussions resolve in a short period (7–10 days) and although the recovery time frame may be longer in children and adolescents.[90]
In the past, the decision to allow athletes to return to participation was frequently based on the grade of concussion. However, current research and recommendations by professional organizations including the National Athletic Trainers' Association recommend against such use of these grading systems. Currently, injured athletes are prohibited from returning to play before they are symptom-free during both rest and exertion and until results of the neuropsychological tests have returned to pre-injury levels.
Three grading systems have been most widely followed: by Robert Cantu, the Colorado Medical Society, and the American Academy of Neurology.[78] Each employs three grades, as summarized in the following table:[23]
| Guidelines | Grade I | Grade II | Grade III |
|---|---|---|---|
| Cantu | Post-traumatic amnesia <30 minutes, no loss of consciousness | Loss of consciousness <5 minutes or amnesia lasting 30 minutes–24 hours | Loss of consciousness >5 minutes or amnesia >24 hours |
| Colorado Medical Society | Confusion, no loss of consciousness | Confusion, post-traumatic amnesia, no loss of consciousness | Any loss of consciousness |
| American Academy of Neurology | Confusion, symptoms last <15 minutes, no loss of consciousness | Symptoms last >15 minutes, no loss of consciousness | Loss of consciousness (IIIa, coma lasts seconds, IIIb for minutes) |
See also
- Concussions in American football
- Concussion in Rugby Union
- Head injury criterion
- Helmet removal (sports)
References
- "What are common TBI symptoms?". NICHD. Retrieved 18 December 2017.
- Mahooti N (January 2018). "Sports-Related Concussion: Acute Management and Chronic Postconcussive Issues". Child and Adolescent Psychiatric Clinics of North America. 27 (1): 93–108. doi:10.1016/j.chc.2017.08.005. PMID 29157505.
- Cassidy JD, Carroll LJ, Peloso PM, Borg J, von Holst H, Holm L, et al. (February 2004). "Incidence, risk factors and prevention of mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury". Journal of Rehabilitation Medicine. 36 (43 Suppl): 28–60. doi:10.1080/16501960410023732. PMID 15083870.
- Ropper AH, Gorson KC (January 2007). "Clinical practice. Concussion". The New England Journal of Medicine. 356 (2): 166–72. doi:10.1056/NEJMcp064645. PMID 17215534.
- "What causes TBI?". www.nichd.nih.gov. Retrieved 18 December 2017.
- "How do health care providers diagnose traumatic brain injury (TBI)?". www.nichd.nih.gov. Retrieved 18 December 2017.
- "What are the treatments for TBI?". www.nichd.nih.gov. Retrieved 18 December 2017.
- "Traumatic Brain Injury (TBI): Condition Information". NICHD. Retrieved 18 December 2017.
- "Concussion recognition tool 5©". British Journal of Sports Medicine. 51 (11): 872. June 2017. doi:10.1136/bjsports-2017-097508CRT5. PMID 28446447.
- McCrory P, Meeuwisse W, Dvořák J, Aubry M, Bailes J, Broglio S, et al. (June 2017). "th international conference on concussion in sport held in Berlin, October 2016". British Journal of Sports Medicine. 51 (11): 838–847. doi:10.1136/bjsports-2017-097699. PMID 28446457.
- Halstead ME, Walter KD (September 2010). "American Academy of Pediatrics. Clinical report--sport-related concussion in children and adolescents". Pediatrics. 126 (3): 597–615. doi:10.1542/peds.2010-2005. PMID 20805152.
- Marshall S, Bayley M, McCullagh S, Berrigan L, Fischer L, Ouchterlony D, Rockwell C, Velikonja D (2018). "Guideline for Concussion/Mild Traumatic Brain Injury and Persistent Symptoms: 3rd Edition (for Adults 18+ years of age)". Ontario Neurotrauma Foundation.
- "CDC Pediatric mTBI Guideline | Concussion | Traumatic Brain Injury | CDC Injury Center". www.cdc.gov. 2020-07-28. Retrieved 2020-08-05.
- Halstead ME, Walter KD, Moffatt K (December 2018). "Sport-Related Concussion in Children and Adolescents". Pediatrics. 142 (6): e20183074. doi:10.1542/peds.2018-3074. PMID 30420472.
- Nguyen R, Fiest KM, McChesney J, Kwon CS, Jette N, Frolkis AD, et al. (November 2016). "The International Incidence of Traumatic Brain Injury: A Systematic Review and Meta-Analysis". The Canadian Journal of Neurological Sciences. Le Journal Canadien Des Sciences Neurologiques. 43 (6): 774–785. doi:10.1017/cjn.2016.290. PMID 27670907.
- "Traumatic Brain Injury". Merck Manuals Professional Edition. October 2013. Retrieved 18 December 2017.
- "Sports-Related Concussion". Merck Manuals Consumer Version. Retrieved 18 December 2017.
- Graham R, Rivara FP, Ford MA, Spicer CM, eds. (2014). Sports-related concussions in youth : improving the science, changing the culture. National Academies Press. p. Chapter 5. ISBN 978-0-309-28800-2. Retrieved 18 December 2017.
- Kenneth Maiese (January 2008). "Concussion". The Merck Manual Home Health Handbook.
- "Traumatic Brain Injury (TBI): Condition Information". nichd.nih.gov/. Retrieved 1 June 2018.
- Kushner D (1998). "Mild traumatic brain injury: toward understanding manifestations and treatment". Archives of Internal Medicine. 158 (15): 1617–24. doi:10.1001/archinte.158.15.1617. PMID 9701095.
- Bowen AP (June 2003). "Second impact syndrome: a rare, catastrophic, preventable complication of concussion in young athletes". Journal of Emergency Nursing. 29 (3): 287–9. doi:10.1067/men.2003.90. PMID 12776088.
- Cantu RC (September 2001). "Posttraumatic Retrograde and Anterograde Amnesia: Pathophysiology and Implications in Grading and Safe Return to Play". Journal of Athletic Training. 36 (3): 244–248. PMC 155413. PMID 12937491.
- Rees PM (December 2003). "Contemporary issues in mild traumatic brain injury". Archives of Physical Medicine and Rehabilitation. 84 (12): 1885–94. doi:10.1016/j.apmr.2003.03.001. PMID 14669199.
- Erlanger DM, Kutner KC, Barth JT, Barnes R (May 1999). "Neuropsychology of sports-related head injury: Dementia Pugilistica to Post Concussion Syndrome". The Clinical Neuropsychologist. 13 (2): 193–209. doi:10.1076/clin.13.2.193.1963. PMID 10949160.
- McCrory PR, Berkovic SF (February 1998). "Concussive convulsions. Incidence in sport and treatment recommendations". Sports Medicine. 25 (2): 131–6. doi:10.2165/00007256-199825020-00005. PMID 9519401.
- Perron AD, Brady WJ, Huff JS (March 2001). "Concussive convulsions: emergency department assessment and management of a frequently misunderstood entity". Academic Emergency Medicine. 8 (3): 296–8. doi:10.1111/j.1553-2712.2001.tb01312.x. PMID 11229957.
- Cantu RC, Aubry M, Dvorak J, Graf-Baumann T, Johnston K, Kelly J, et al. (October 2006). "Overview of concussion consensus statements since 2000" (PDF). Neurosurgical Focus. 21 (4): E3. doi:10.3171/foc.2006.21.4.4. PMID 17112193. Archived from the original (PDF) on 2008-02-28.
- Quality Standards Subcommittee of the American Academy of Neurology (1997). "Practice Parameter: The Management of Concussion in Sports (Summary Statement)" (PDF). American Academy of Neurology. pp. 1–7. Archived from the original (PDF) on 2008-02-28. Retrieved 2008-03-05.
- Anderson MK, Hall SJ, Martin M (2004). Foundations of Athletic Training: Prevention, Assessment, and Management. Lippincott Williams & Wilkins. p. 236. ISBN 978-0-7817-5001-1.
- Mayo Clinic Staff (2007). "Concussion". Mayo Clinic. Retrieved 2008-01-10.
- Sivák S, Kurca E, Jancovic D, Petriscák S, Kucera P (2005). "[Contemporary view on mild brain injuries in adult population]" [An outline of the current concepts of mild brain injury with emphasis on the adult population] (PDF). Casopis Lekaru Ceskych (in Slovak). 144 (7): 445–50, discussion 451–4. PMID 16161536. Archived from the original (PDF) on 2008-02-27.
- Heegaard W, Biros M (August 2007). "Traumatic brain injury". Emergency Medicine Clinics of North America. 25 (3): 655–78, viii. doi:10.1016/j.emc.2007.07.001. PMID 17826211.
- Pellman EJ, Viano DC (October 2006). "Concussion in professional football: summary of the research conducted by the National Football League's Committee on Mild Traumatic Brain Injury" (PDF). Neurosurgical Focus. 21 (4): E12. doi:10.3171/foc.2006.21.4.13. PMID 17112190. Archived from the original (PDF) on 2008-02-28.
- Shaw NA (July 2002). "The neurophysiology of concussion". Progress in Neurobiology. 67 (4): 281–344. doi:10.1016/S0301-0082(02)00018-7. PMID 12207973.
- Poirier MP (2003). "Concussions: Assessment, management, and recommendations for return to activity". Clinical Pediatric Emergency Medicine. 4 (3): 179–85. doi:10.1016/S1522-8401(03)00061-2.
- Anderson T, Heitger M, Macleod AD (2006). "Concussion and mild head injury" (PDF). Practical Neurology. 6 (6): 342–57. CiteSeerX 10.1.1.536.9655. doi:10.1136/jnnp.2006.106583. Archived from the original (PDF) on 2007-07-01.
- Guskiewicz KM, Mihalik JP, Shankar V, Marshall SW, Crowell DH, Oliaro SM, et al. (December 2007). "Measurement of head impacts in collegiate football players: relationship between head impact biomechanics and acute clinical outcome after concussion". Neurosurgery. 61 (6): 1244–52, discussion 1252–3. doi:10.1227/01.neu.0000306103.68635.1a. PMID 18162904.
- Gever D (December 7, 2007). "Any football helmet hit can cause potential concussion". MedPage Today. Retrieved 2008-02-27.
- Pearce JM (2007). "Observations on concussion. A review". European Neurology. 59 (3–4): 113–9. doi:10.1159/000111872. PMID 18057896.
- Bigler ED (January 2008). "Neuropsychology and clinical neuroscience of persistent post-concussive syndrome". Journal of the International Neuropsychological Society. 14 (1): 1–22. doi:10.1017/S135561770808017X. PMID 18078527.
- Rousseau P, Post A, Hoshizaki TB (2009). "The effects of impact management materials in ice hockey helmets on head injury criteria". Proceedings of the Institution of Mechanical Engineers, Part P: Journal of Sports Engineering and Technology. 223 (4): 159–65. doi:10.1243/17543371JSET36. ISSN 1754-3371.
- Mouzon BC, Bachmeier C, Ferro A, Ojo JO, Crynen G, Acker CM, et al. (February 2014). "Chronic neuropathological and neurobehavioral changes in a repetitive mild traumatic brain injury model". Annals of Neurology. 75 (2): 241–54. doi:10.1002/ana.24064. PMID 24243523.
- Smith DH, Johnson VE, Stewart W (April 2013). "Chronic neuropathologies of single and repetitive TBI: substrates of dementia?". Nature Reviews. Neurology. 9 (4): 211–21. doi:10.1038/nrneurol.2013.29. PMC 4513655. PMID 23458973.
- McAllister TW, Sparling MB, Flashman LA, Saykin AJ (December 2001). "Neuroimaging findings in mild traumatic brain injury". Journal of Clinical and Experimental Neuropsychology. 23 (6): 775–91. doi:10.1076/jcen.23.6.775.1026. PMID 11910544.
- Iverson GL (May 2005). "Outcome from mild traumatic brain injury". Current Opinion in Psychiatry. 18 (3): 301–17. doi:10.1097/01.yco.0000165601.29047.ae. PMID 16639155.
- "Concussion (mild traumatic brain injury) and the team physician: a consensus statement" (PDF). Medicine and Science in Sports and Exercise. 37 (11): 2012–6. November 2005. doi:10.1249/01.mss.0000186726.18341.70. PMID 16286874. Archived from the original (PDF) on 2008-02-28.
- Giza CC, Hovda DA (September 2001). "The Neurometabolic Cascade of Concussion". Journal of Athletic Training. 36 (3): 228–235. PMC 155411. PMID 12937489.
- Hardman JM, Manoukian A (May 2002). "Pathology of head trauma". Neuroimaging Clinics of North America. 12 (2): 175–87, vii. doi:10.1016/S1052-5149(02)00009-6. PMID 12391630.
- Mouzon BC, Bachmeier C, Ojo JO, Acker CM, Ferguson S, Paris D, et al. (January 2018). "Lifelong behavioral and neuropathological consequences of repetitive mild traumatic brain injury". Annals of Clinical and Translational Neurology. 5 (1): 64–80. doi:10.1002/acn3.510. PMC 5771321. PMID 29376093.
- CNN (2009-01-27). "Dead Athletes Brains Show Damage From Concussions". Boston University: Center for the Study of Traumatic Encephalopathy. Retrieved 2009-01-28.
- McCrory PR, Berkovic SF (December 2001). "Concussion: the history of clinical and pathophysiological concepts and misconceptions". Neurology. 57 (12): 2283–9. doi:10.1212/WNL.57.12.2283. PMID 11756611.
- Aubry M, Cantu R, Dvorak J, Graf-Baumann T, Johnston K, Kelly J, et al. (February 2002). "Summary and agreement statement of the First International Conference on Concussion in Sport, Vienna 2001. Recommendations for the improvement of safety and health of athletes who may suffer concussive injuries". British Journal of Sports Medicine. 36 (1): 6–10. doi:10.1136/bjsm.36.1.6. PMC 1724447. PMID 11867482.
- Romeu-Mejia R, Giza CC, Goldman JT (June 2019). "Concussion Pathophysiology and Injury Biomechanics". Current Reviews in Musculoskeletal Medicine. 12 (2): 105–116. doi:10.1007/s12178-019-09536-8. PMC 6542913. PMID 30820754.
- Barkhoudarian G, Hovda DA, Giza CC (May 2016). "The Molecular Pathophysiology of Concussive Brain Injury - an Update". Physical Medicine and Rehabilitation Clinics of North America. 27 (2): 373–93. doi:10.1016/j.pmr.2016.01.003. PMID 27154851.
- Ontario Neurotrauma Foundation (2019). "Living Guideline for Diagnosing and Managing Pediatric Concussion". Retrieved 2 August 2014.
- Cook RS, Schweer L, Shebesta KF, Hartjes K, Falcone RA (2006). "Mild traumatic brain injury in children: just another bump on the head?". Journal of Trauma Nursing. 13 (2): 58–65. doi:10.1097/00043860-200604000-00007. PMID 16884134.
- Kay A, Teasdale G (September 2001). "Head injury in the United Kingdom". World Journal of Surgery. 25 (9): 1210–20. doi:10.1007/s00268-001-0084-6. PMID 11571960.
- "Facts About Concussion and Brain Injury". Centers for Disease Control and Prevention. 2006. Retrieved 2008-01-13.
- American Medical Society for Sports Medicine (24 April 2014), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American Medical Society for Sports Medicine, retrieved 29 July 2014
- Borg J, Holm L, Cassidy JD, Peloso PM, Carroll LJ, von Holst H, Ericson K (February 2004). "Diagnostic procedures in mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury". Journal of Rehabilitation Medicine. 36 (43 Suppl): 61–75. doi:10.1080/16501960410023822. PMID 15083871.
- "Sport concussion assessment tool - 5th edition". British Journal of Sports Medicine: bjsports–2017–097506SCAT5. 2017-04-26. doi:10.1136/bjsports-2017-097506SCAT5. ISSN 0306-3674.
- Medicine, BMJ Publishing Group Ltd and British Association of Sport and Exercise (2017-06-01). "Sport concussion assessment tool for childrens ages 5 to 12 years". British Journal of Sports Medicine. 51 (11): 862–869. doi:10.1136/bjsports-2017-097492childscat5. ISSN 0306-3674. PMID 28446448.
- Moser RS, Iverson GL, Echemendia RJ, Lovell MR, Schatz P, Webbe FM, et al. (November 2007). "Neuropsychological evaluation in the diagnosis and management of sports-related concussion". Archives of Clinical Neuropsychology. 22 (8): 909–16. doi:10.1016/j.acn.2007.09.004. PMID 17988831.
- Randolph C (2011). "Baseline neuropsychological testing in managing sport-related concussion: does it modify risk?". Current Sports Medicine Reports. 10 (1): 21–6. doi:10.1249/JSR.0b013e318207831d. PMID 21228656.
- Parachute (November 2018). "Statement on Concussion Baseline Testing in Canada" (PDF). Retrieved August 12, 2020.
- Binder LM (August 1986). "Persisting symptoms after mild head injury: a review of the postconcussive syndrome". Journal of Clinical and Experimental Neuropsychology. 8 (4): 323–46. doi:10.1080/01688638608401325. PMID 3091631.
- "Press Announcements – FDA authorizes marketing of first blood test to aid in the evaluation of concussion in adults". www.fda.gov. Retrieved 24 February 2018.
- Barth JT, Varney NR, Ruchinskas RA, Francis JP (1999). "Mild head injury: The new frontier in sports medicine". In Varney NR, Roberts RJ (eds.). The Evaluation and Treatment of Mild Traumatic Brain Injury. Hillsdale, New Jersey: Lawrence Erlbaum Associates. pp. 85–86. ISBN 978-0-8058-2394-3.
- Delaney JS, Abuzeyad F, Correa JA, Foxford R (August 2005). "Recognition and characteristics of concussions in the emergency department population". The Journal of Emergency Medicine. 29 (2): 189–97. doi:10.1016/j.jemermed.2005.01.020. PMID 16029831.
- Bryant RA (January 2008). "Disentangling mild traumatic brain injury and stress reactions". The New England Journal of Medicine. 358 (5): 525–7. doi:10.1056/NEJMe078235. PMID 18234757.
- Mannix R, Levy R, Zemek R, Yeates KO, Arbogast K, Meehan WP, et al. (June 2020). "Fluid Biomarkers of Pediatric Mild Traumatic Brain Injury: A Systematic Review". Journal of Neurotrauma. doi:10.1089/neu.2019.6956. PMID 32303159.
- Satz P, Zaucha K, McCleary C, Light R, Asarnow R, Becker D (September 1997). "Mild head injury in children and adolescents: a review of studies (1970-1995)". Psychological Bulletin. 122 (2): 107–31. doi:10.1037/0033-2909.122.2.107. PMID 9283296.
- Comper P, Bisschop SM, Carnide N, Tricco A (October 2005). "A systematic review of treatments for mild traumatic brain injury". Brain Injury. 19 (11): 863–80. doi:10.1080/02699050400025042. PMID 16296570.
- Parkinson D (1999). "Concussion confusion". Critical Reviews in Neurosurgery. 9 (6): 335–39. doi:10.1007/s003290050153. ISSN 1433-0377.
- Head Injury: Triage, Assessment, Investigation and Early Management of Head Injury in Infants, Children and Adults (PDF). National Institute for Health and Clinical Excellence. September 2007. ISBN 978-0-9549760-5-7. Retrieved 2008-01-26.
- Ruff RM, Grant I (1999). "Postconcussional disorder: Background to DSM-IV and future considerations". In Varney NR, Roberts RJ (eds.). The Evaluation and Treatment of Mild Traumatic Brain Injury. Hillsdale, New Jersey: Lawrence Erlbaum Associates. p. 320. ISBN 978-0-8058-2394-3.
- Cobb S, Battin B (October 2004). "Second-impact syndrome". The Journal of School Nursing. 20 (5): 262–7. doi:10.1177/10598405040200050401. PMID 15469376.
- Petchprapai N, Winkelman C (October 2007). "Mild traumatic brain injury: determinants and subsequent quality of life. A review of the literature". The Journal of Neuroscience Nursing. 39 (5): 260–72. doi:10.1097/01376517-200710000-00002. PMID 17966292.
- Lee LK (August 2007). "Controversies in the sequelae of pediatric mild traumatic brain injury". Pediatric Emergency Care. 23 (8): 580–3, quiz 584–6. doi:10.1097/PEC.0b013e31813444ea. PMID 17726422.
- Benton AL, Levin HS, Eisenberg HM (1989). Mild Head Injury. Oxford [Oxfordshire]: Oxford University Press. pp. v. ISBN 978-0-19-505301-2.
- van der Naalt J (December 2001). "Prediction of outcome in mild to moderate head injury: a review". Journal of Clinical and Experimental Neuropsychology. 23 (6): 837–51. doi:10.1076/jcen.23.6.837.1018. PMID 11910548.
- Savitsky EA, Votey SR (January 2000). "Current controversies in the management of minor pediatric head injuries". The American Journal of Emergency Medicine. 18 (1): 96–101. doi:10.1016/S0735-6757(00)90060-3. PMID 10674544.
- Parikh S, Koch M, Narayan RK (2007). "Traumatic brain injury". International Anesthesiology Clinics. 45 (3): 119–35. doi:10.1097/AIA.0b013e318078cfe7. PMID 17622833.
- Larner AJ, Barker RJ, Scolding N, Rowe D (2005). The A–Z of Neurological Practice: a Guide to Clinical Neurology. Cambridge, UK: Cambridge University Press. p. 199. ISBN 978-0-521-62960-7.
- Enniss TM, Basiouny K, Brewer B, Bugaev N, Cheng J, Danner OK, et al. (2018). "Primary prevention of contact sports-related concussions in amateur athletes: a systematic review from the Eastern Association for the Surgery of Trauma". Trauma Surgery & Acute Care Open. 3 (1): e000153. doi:10.1136/tsaco-2017-000153. PMC 6018851. PMID 30023433.
- Emery CA, Black AM, Kolstad A, Martinez G, Nettel-Aguirre A, Engebretsen L, et al. (June 2017). "What strategies can be used to effectively reduce the risk of concussion in sport? A systematic review". British Journal of Sports Medicine. 51 (12): 978–984. doi:10.1136/bjsports-2016-097452. PMID 28254746.
- Harmon KG, Drezner JA, Gammons M, Guskiewicz KM, Halstead M, Herring SA, et al. (January 2013). "American Medical Society for Sports Medicine position statement: concussion in sport". British Journal of Sports Medicine. 47 (1): 15–26. doi:10.1136/bjsports-2012-091941. PMID 23243113.
- Schneider DK, Grandhi RK, Bansal P, Kuntz GE, Webster KE, Logan K, et al. (October 2017). "Current state of concussion prevention strategies: a systematic review and meta-analysis of prospective, controlled studies". British Journal of Sports Medicine. 51 (20): 1473–1482. doi:10.1136/bjsports-2015-095645. PMID 27251896.
- McCrory P, Meeuwisse W, Johnston K, Dvorak J, Aubry M, Molloy M, Cantu R (Jul–Aug 2009). "Consensus statement on concussion in sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008". Journal of Athletic Training. 44 (4): 434–48. doi:10.4085/1062-6050-44.4.434. PMC 2707064. PMID 19593427.
- "Information about NICE clinical guideline" (PDF). National Institute for Health and Clinical Excellence. September 2007. Retrieved 2008-01-26.
- DeMatteo C, Bednar ED, Randall S, Falla K (February 2020). "Effectiveness of return to activity and return to school protocols for children postconcussion: a systematic review". BMJ Open Sport & Exercise Medicine. 6 (1): e000667. doi:10.1136/bmjsem-2019-000667. PMC 7047486. PMID 32153982.
- DeMatteo C, Bednar ED, Randall S, Falla K (2020-02-24). "Effectiveness of return to activity and return to school protocols for children postconcussion: a systematic review". BMJ Open Sport & Exercise Medicine. 6 (1): e000667. doi:10.1136/bmjsem-2019-000667. PMC 7047486. PMID 32153982.
- Reymond MA, Marbet G, Radü EW, Gratzl O (1992). "Aspirin as a risk factor for hemorrhage in patients with head injuries". Neurosurgical Review. 15 (1): 21–5. doi:10.1007/BF02352062. PMID 1584433.
- "What Can I Do to Help Feel Better After a Concussion?". Atlanta, GA: Center of Disease Control. March 8, 2010.
- Thornton KE, Carmody DP (June 2008). "Efficacy of traumatic brain injury rehabilitation: interventions of QEEG-guided biofeedback, computers, strategies, and medications" (PDF). Applied Psychophysiology and Biofeedback. 33 (2): 101–24. doi:10.1007/s10484-008-9056-z. PMID 18551365.
- Lumba-Brown A, Yeates KO, Sarmiento K, Breiding MJ, Haegerich TM, Gioia GA, et al. (November 2018). "Centers for Disease Control and Prevention Guideline on the Diagnosis and Management of Mild Traumatic Brain Injury Among Children". JAMA Pediatrics. 172 (11): e182853. doi:10.1001/jamapediatrics.2018.2853. PMC 7006878. PMID 30193284.
- Murray ED, Buttner N, Price BH (2012). "Depression and Psychosis in Neurological Practice". In Bradley WG, Daroff RB, Fenichel GM, Jankovic J (eds.). Bradley's neurology in clinical practice. 1 (6th ed.). Philadelphia, PA: Elsevier/Saunders. p. 111. ISBN 978-1-4377-0434-1.
- Alexander MP (July 1995). "Mild traumatic brain injury: pathophysiology, natural history, and clinical management". Neurology. 45 (7): 1253–60. doi:10.1212/WNL.45.7.1253. PMID 7617178.
- Hall RC, Hall RC, Chapman MJ (2005). "Definition, diagnosis, and forensic implications of postconcussional syndrome". Psychosomatics. 46 (3): 195–202. doi:10.1176/appi.psy.46.3.195. PMID 15883140.
- Masferrer R, Masferrer M, Prendergast V, Harrington TR (2000). "Grading scale for cerebral concussions". BNI Quarterly. 16 (1). ISSN 0894-5799.
- Schulz MR, Marshall SW, Mueller FO, Yang J, Weaver NL, Kalsbeek WD, Bowling JM (November 2004). "Incidence and risk factors for concussion in high school athletes, North Carolina, 1996-1999". American Journal of Epidemiology. 160 (10): 937–44. doi:10.1093/aje/kwh304. PMID 15522850.
- Ryan LM, Warden DL (November 2003). "Post concussion syndrome". International Review of Psychiatry. 15 (4): 310–6. doi:10.1080/09540260310001606692. PMID 15276952.
- Zemek RL, Farion KJ, Sampson M, McGahern C (March 2013). "Prognosticators of persistent symptoms following pediatric concussion: a systematic review". JAMA Pediatrics. 167 (3): 259–65. doi:10.1001/2013.jamapediatrics.216. PMID 23303474.
- Boake C, McCauley SR, Levin HS, Pedroza C, Contant CF, Song JX, et al. (2005). "Diagnostic criteria for postconcussional syndrome after mild to moderate traumatic brain injury". The Journal of Neuropsychiatry and Clinical Neurosciences. 17 (3): 350–6. doi:10.1176/appi.neuropsych.17.3.350. PMID 16179657. Archived from the original on 2006-10-06.
- Willer B, Leddy JJ (September 2006). "Management of concussion and post-concussion syndrome". Current Treatment Options in Neurology. 8 (5): 415–26. doi:10.1007/s11940-006-0031-9. PMID 16901381.
- Klein A (Nov 11, 2017). "Pure oxygen can help concussion". New Scientist. 236 (3151): 10. Bibcode:2017NewSc.236...10K. doi:10.1016/S0262-4079(17)32192-9.
- Mouzon BC, Bachmeier C, Ojo JO, Acker CM, Ferguson S, Paris D, Ait-Ghezala G, Crynen G, Davies P, Mullan M, Stewart W, Crawford F (January 2018). "Lifelong behavioral and neuropathological consequences of repetitive mild traumatic brain injury". Annals of Clinical and Translational Neurology. 5 (1): 64–80. doi:10.1002/acn3.510. PMC 5771321. PMID 29376093. Lay summary – ScienceDaily.
- Harmon KG (September 1999). "Assessment and management of concussion in sports". American Family Physician. 60 (3): 887–92, 894. PMID 10498114.
- Cantu RC (August 2007). "Chronic traumatic encephalopathy in the National Football League". Neurosurgery. 61 (2): 223–5. doi:10.1227/01.NEU.0000255514.73967.90. PMID 17762733.
- Mendez MF (1995). "The neuropsychiatric aspects of boxing". International Journal of Psychiatry in Medicine. 25 (3): 249–62. doi:10.2190/CUMK-THT1-X98M-WB4C. PMID 8567192.
- Jordan BD (2000). "Chronic traumatic brain injury associated with boxing". Seminars in Neurology. 20 (2): 179–85. doi:10.1055/s-2000-9826. PMID 10946737.
- McCrory P (July 2001). "Does second impact syndrome exist?". Clinical Journal of Sport Medicine. 11 (3): 144–9. doi:10.1097/00042752-200107000-00004. PMID 11495318.
- Gordon KE, Dooley JM, Wood EP (May 2006). "Descriptive epidemiology of concussion". Pediatric Neurology. 34 (5): 376–8. doi:10.1016/j.pediatrneurol.2005.09.007. PMID 16647998.
- McKeever CK, Schatz P (2003). "Current issues in the identification, assessment, and management of concussions in sports-related injuries". Applied Neuropsychology. 10 (1): 4–11. doi:10.1207/S15324826AN1001_2. PMID 12734070.
- Langlois JA, Rutland-Brown W, Wald MM (2006). "The epidemiology and impact of traumatic brain injury: a brief overview". The Journal of Head Trauma Rehabilitation. 21 (5): 375–8. doi:10.1097/00001199-200609000-00001. PMID 16983222.
- Cantu RC (January 1998). "Second-impact syndrome". Clinics in Sports Medicine. 17 (1): 37–44. doi:10.1016/S0278-5919(05)70059-4. PMID 9475969.
- Solomon GS, Johnston KM, Lovell MR (2006). The Heads-up on Sport Concussion. Champaign, IL: Human Kinetics Pub. p. 77. ISBN 978-0-7360-6008-0.
- Denny-Brown D, Russell WR (December 1940). "Experimental cerebral concussion". The Journal of Physiology. 99 (1): 153. doi:10.1113/jphysiol.1940.sp003887. PMC 1394062. PMID 16995229.
- Borg J, Holm L, Peloso PM, Cassidy JD, Carroll LJ, von Holst H, et al. (February 2004). "Non-surgical intervention and cost for mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury". Journal of Rehabilitation Medicine. 36 (43 Suppl): 76–83. doi:10.1080/16501960410023840. PMID 15083872.
- Kraus JF, Chu LD (2005). "Epidemiology". In Silver JM, McAllister TW, Yudofsky SC (eds.). Textbook of Traumatic Brain Injury. American Psychiatric Pub., Inc. p. 23. ISBN 978-1-58562-105-7.
- National Center for Injury Prevention and Control (2003). "Report to congress on mild traumatic brain injury in the United States: Steps to prevent a serious public health problem" (PDF). Atlanta, GA: Centers for Disease Control and Prevention. Archived from the original (PDF) on 2008-02-28. Retrieved 2008-01-19.
- Brooks D, Hunt B (2006). "Current concepts in concussion diagnosis and management in sports: A clinical review". BC Medical Journal. 48 (9): 453–59.
- Toledo E, Lebel A, Becerra L, Minster A, Linnman C, Maleki N, et al. (July 2012). "The young brain and concussion: imaging as a biomarker for diagnosis and prognosis". Neuroscience and Biobehavioral Reviews. 36 (6): 1510–31. doi:10.1016/j.neubiorev.2012.03.007. PMC 3372677. PMID 22476089.
- Maruta J, Lee SW, Jacobs EF, Ghajar J (October 2010). "A unified science of concussion". Annals of the New York Academy of Sciences. 1208 (1): 58–66. Bibcode:2010NYASA1208...58M. doi:10.1111/j.1749-6632.2010.05695.x. PMC 3021720. PMID 20955326.
- McCrory P, Johnston K, Meeuwisse W, Aubry M, Cantu R, Dvorak J, et al. (April 2005). "Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004". British Journal of Sports Medicine. 39 (4): 196–204. doi:10.1136/bjsm.2005.018614. PMC 1725173. PMID 15793085.
External links
| Classification | |
|---|---|
| External resources |
- "Facts about Concussion and Brain Injury and Where to Get Help" US Centers for Disease Control and Prevention
- "Concussion in High School Sports" US Centers for Disease Control and Prevention
- 2018 CDC Guideline on MTBI in children