Cancer prevention
Cancer prevention is the practice of taking active measures to decrease the incidence of cancer and mortality.[1][2] The practice of prevention is dependent upon both individual efforts to improve lifestyle and seek preventive screening, and socioeconomic or public policy related to cancer prevention.[3] Globalized cancer prevention is regarded as a critical objective due to its applicability to large populations, reducing long term effects of cancer by promoting proactive health practices and behaviors, and its perceived cost-effectiveness and viability for all socioeconomic classes.[2]
The majority of cancer cases are due to the accumulation of environmental pollution being inherited as epigenetic damage and many, but not all, of these environmental factors are controllable lifestyle choices.[4] Greater than a reported 75% of cancer deaths could be prevented by avoiding risk factors including: tobacco, overweight / obesity, an insufficient diet, physical inactivity, alcohol, sexually transmitted infections, and air pollution.[5][6] Not all environmental causes are controllable, such as naturally occurring background radiation, and other cases of cancer are caused through hereditary genetic disorders. Current gene editing techniques under development may serve as preventive measures in the future.[7] Future preventive screening measures can be additionally improved by minimizing invasiveness and increasing specificity by taking individual biologic make up into account, also known as "population-based personalized cancer screening."[2]
The concerned
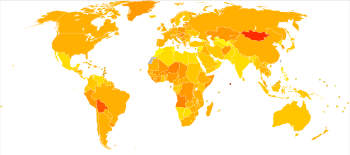
|
no data
≤ 55
55–80
80–105
105–130
130–155
155–180
|
180–205
205–230
230–255
255–280
280–305
≥ 305
|
Anyone can get cancer,[9] the age is one of the biggest factors that can make a person more likely to get cancer: 3 out of 4 cancers are found in people aged 55 or older.
Dietary

While many dietary recommendations have been proposed to reduce the risk of cancer, the evidence to support them is not definitive.[10][11] The primary dietary factors that increase risk are obesity and alcohol consumption; with a diet low in fruits and vegetables and high in red meat being implicated but not confirmed.[12][13] A 2014 meta-analysis did not find a relationship between fruits and vegetables and cancer.[14] Consumption of coffee is associated with a reduced risk of liver cancer.[15] Studies have linked excessive consumption of red or processed meat to an increased risk of breast cancer, colon cancer, and pancreatic cancer, a phenomenon which could be due to the presence of carcinogens in meats cooked at high temperatures.[16][17] Dietary recommendations for cancer prevention typically include an emphasis on vegetables, fruit, whole grains, and fish, and an avoidance of processed and red meat (beef, pork, lamb), animal fats, and refined carbohydrates.[10][11]
Physical activity
Research shows that regular physical activity helps to reduce up to 30%[18][19] the risk of a variety of cancer types, such as colon cancer, breast cancer, lung cancer and endometrium cancer.[20][21] The biological mechanisms underlying this association are still not well understood[21] but different biological pathways involved in cancer have been studied suggesting that physical activity reduces cancer risk by helping weight control, reducing hormones such as estrogen and insulin, reducing inflammation and strengthening the immune system.[21][22]
Medication
The concept that medications can be used to prevent cancer is attractive, and evidence supports their use in a few defined circumstances.[23] In the general population, NSAIDs reduce the risk of colorectal cancer however due to the cardiovascular and gastrointestinal side effects they cause overall harm when used for prevention.[24] Aspirin has been found to reduce the risk of death from cancer by about 7%.[25] COX-2 inhibitor may decrease the rate of polyp formation in people with familial adenomatous polyposis however are associated with the same adverse effects as NSAIDs.[26] Daily use of tamoxifen or raloxifene has been demonstrated to reduce the risk of developing breast cancer in high-risk women.[27] The benefit verses harm for 5-alpha-reductase inhibitor such as finasteride is not clear.[28] A study showing a proof-of-principle has also been done with the human proteins IFNalpha2a and macrophage-CSF, produced by genetically modified hens.[29]
Vitamins have not been found to be effective at preventing cancer,[30] although low blood levels of vitamin D are correlated with increased cancer risk.[31][32] Whether this relationship is causal and vitamin D supplementation is protective is not determined.[33] Beta-Carotene supplementation has been found to increase lung cancer rates in those who are high risk.[34] Folic acid supplementation has not been found effective in preventing colon cancer and may increase colon polyps.[35] A 2018 systematic review concluded that selenium has no beneficial effect in reducing the risk of cancer based on high quality evidence.[36] However, more studies are needed to determine whether individuals with a specific genetic background or nutritional status may benefit, and whether certain formulations of selenium may have an effect on risk.
Vaccination
Anti-cancer vaccines can be preventive / prophylactic or be used as therapeutic treatment.[2] All such vaccines incite adaptive immunity by enhancing cytotoxic T lymphocyte (CTL) recognition and activity against tumor-associated or tumor-specific antigens (TAA and TSAs).
Vaccines have been developed that prevent infection by some carcinogenic viruses.[37] Human papillomavirus vaccine (Gardasil and Cervarix) decreases the risk of developing cervical cancer.[37] The hepatitis B vaccine prevents infection with hepatitis B virus and thus decreases the risk of liver cancer.[37] The administration of human papillomavirus and hepatitis B vaccinations is recommended when resources allow.[38]
Some cancer vaccines are usually immunoglobulin-based and target antigens specific to cancer or abnormal human cells.[2][39] These vaccines may be given to treat cancer during the progression of disease to boost the immune system's ability to recognize and attack cancer antigens as foreign entities. Antibodies for cancer cell vaccines may be taken from the patient's own body (autologous vaccine) or from another patient (allogeneic vaccine).[37] Several autologous vaccines, such as Oncophage for kidney cancer and Vitespen for a variety of cancers, have either been released or are undergoing clinical trial. FDA-approved vaccines, such as Sipuleucel-T for metastasizing prostate cancer or Nivolumab for melanoma and lung cancer can act either by targeting over-expressed or mutated proteins or by temporarily inhibiting immune checkpoints to boost immune activity.[2][40]
Screening
Screening procedures, commonly sought for more prevalent cancers, such as colon, breast, and cervical, have greatly improved in the past few decades from advances in biomarker identification and detection.[2] Early detection of pancreatic cancer biomarkers was accomplished using SERS-based immunoassay approach.[41] A SERS-base multiplex proteinbiomarker detection platform in a microfluidic chip to detect is used to detect several protein biomarkers to predict the type of disease and critical biomarkers and increase the chance of diagnosis between diseases with similar biomarkers (PC, OVC, and pancreatitis).[42]
Cervical Cancer
Cervical cancer is usually screened through in vitro examination of the cells of the cervix (e.g. Pap smear), colposcopy, or direct inspection of the cervix (after application of dilute acetic acid), or testing for HPV, the oncogenic virus that is the necessary cause of cervical cancer.[37] Screening is recommended for women over 21 years, initially women between 21–29 years old are encouraged to receive Pap smear screens every three years, and those over 29 every five years.[2] For women older than the age of 65 and with no history of cervical cancer or abnormality, and with an appropriate precedence of negative Pap test results may cease regular screening.[43]
Still, adherence to recommended screening plans depends on age and may be linked to "educational level, culture, psychosocial issues, and marital status," further emphasizing the importance of addressing these challenges in regards to cancer screening.[2]
Colorectal Cancer
Colorectal cancer is most often screened with the fecal occult blood test (FOBT). Variants of this test include guaiac-based FOBT (gFOBT), the fecal immunochemical test (FIT), and stool DNA (sDNA) testing.[44] Further testing includes flexible sigmoidoscopy (FS), total colonoscopy (TC), or computed tomography (CT) scans if a TC is non-ideal. A recommended age at which to begin screening is 50 years. However, this is highly dependent on medical history and exposure to CRC risk factors. Effective screening has been shown to reduce CRC incidence by 33% and CRC morality by 43%.[2]
Breast Cancer
The estimated number of new breast cancer cases in the US in 2018 is predicted to be more than 1.7 million, with more than six-hundred thousand deaths.[45] Factors such as breast size, reduced physical activity, obesity and overweight status, infertility and never having had children, hormone replacement therapy (HRT), and genetics are risk factors for breast cancer.[2] Mammograms are widely used to screen for breast cancer, and are recommended for women 50–74 years of age by the US Preventive Services Task Force (USPSTF). However, the USPSTF recommended against mammographies for women 40–49 years old due to possibility of overdiagnosis.[2][46]
Preventable causes of cancer
As of 2017, tobacco use, diet and nutrition, physical activity, obesity/overweight status, infectious agents, and chemical and physical carcinogens have been reported to be the leading areas where cancer prevention can be practiced through enacting positive lifestyle changes, getting appropriate regular screening, and getting vaccinated.[47]
The development of many common cancers are incited by such risk factors. For example, consumption of tobacco and alcohol, a medical history of genital warts and STDs, immunosuppression, unprotected sex, and early age of first sexual intercourse and pregnancy all may serve as risk factors for cervical cancer. Obesity, red meat of processed meat consumption, tobacco and alcohol, and a medical history of inflammatory bowel diseases are all risk factors for colorectal cancer (CRC). On the other hand, exercise and consumption of vegetables may help decrease the risk of CRC.[2]
Several preventable causes of cancer were highlighted in Doll and Peto's landmark 1981 study,[5] estimating that 75 – 80% of cancers in the United States could be prevented by avoidance of 11 different factors. A 2013 review of more recent cancer prevention literature by Schottenfeld et al.,[48] summarizing studies reported between 2000 and 2010, points to most of the same avoidable factors identified by Doll and Peto. However, Schottenfeld et al. considered fewer factors (e.g. non inclusion of diet) in their review than Doll and Peto, and indicated that avoidance of these fewer factors would result in prevention of 60% of cancer deaths. The table below indicates the proportions of cancer deaths attributed to different factors, summarizing the observations of Doll and Peto, Shottenfeld et al. and several other authors, and shows the influence of major lifestyle factors on the prevention of cancer, such as tobacco, an unhealthy diet, obesity and infections.
| Factor | Doll and Peto[5] | Schottenfeld et al.[48] | Other reports |
|---|---|---|---|
| Tobacco | 30% | 30% | 38% men, 23% women,[49] 30%,[50] 25-30%[6] |
| Deleterious diet | 35% | - | 32%,[51] 10%,[52] 30-35%[6] |
| Obesity | * | 10% | 14% women, 20% men, among non-smokers,[53] 10-20%,[6] 19-20% United States, 16-18% Great Britain, 13% Brazil, 11-12% China[54] |
| Infection† | 10% | 5-8% | 7-10%,[55] 8% developed nations, 26% developing nations,[50] 10% high income, 25% African[6] |
| Alcohol | 3% | 3-4% | 3.6%,[50] 8% USA, 20% France[56] |
| Occupational exposures | 4% | 3-5% | 2-10%, may be 15-20% in men[57] |
| Radiation (solar and ionizing) | 3% | 3-4% | up to 10%[6] |
| Physical inactivity | * | <5% | 7%[58] |
| Reproductive and sexual behavior | 1-13% | - | - |
| Pollution | 2% | - | - |
| Medicines and medical procedures | 1% | - | - |
| Industrial products | <1% | - | - |
| Food additives | <1% | - | - |
*Included in diet
†Carcinogenic infections include: for the uterine cervix (human papillomavirus [HPV]), liver (hepatitis B virus [HBV] and hepatitis C virus [HCV]), stomach (Helicobacter pylori [H pylori]), lymphoid tissues (Epstein-Barr virus [EBV]), nasopharynx (EBV), urinary bladder (Schistosoma hematobium), and biliary tract (Opisthorchis viverrini, Clonorchis sinensis)
History of Cancer Prevention
Cancer has been thought to be a preventable disease since the time of Roman physician Galen, who observed that unhealthy diet was correlated with cancer incidence. In 1713, Italian physician Ramazzini hypothesized that abstinence caused lower rates of cervical cancer in nuns. Further observation in the 18th century led to the discovery that certain chemicals, such as tobacco, soot and tar (leading to scrotal cancer in chimney sweepers, as reported by Percivall Pot in 1775), could serve as carcinogens for humans. Although Potts suggested preventive measures for chimney sweeps (wearing clothes to prevent contact bodily contact with soot), his suggestions were only put into practice in Holland, resulting in decreasing rates of scrotal cancer in chimney sweeps. Later, the 19th century brought on the onset of the classification of chemical carcinogens.[59]
In the early 20th century, physical and biological carcinogens, such as X ray radiation or the Rous Sarcoma Virus discovered 1911, were identified. Despite observed correlation of environmental or chemical factors with cancer development, there was a deficit of formal prevention research and lifestyle changes for cancer prevention were not feasible during this time.[59]
Timeline of Cancer Prevention Research [60]
In the 1970s, federally-funded efforts brought the importance of diet and early screening in the prevention of cancer to the public eye.
1971 - Nixon signs NCA, federally-funded cancer research established.
1974 - Disadvantaged women benefit from NCI-funded ovarian screening.
1977 - Senate Select Committee on Nutrition publishes dietary guidelines for cancer prevention.
1978 - Community Hospital Oncology Program (CHOP)
1979 - NCI diet for cancer prevention: low-fat, low alcohol, increased fiber, balanced diet.
In the 1980s, early federally-funded programs and institutions were established to pioneer research in the field of cancer prevention.
1981 - Community Clinical Oncology Program.
1982 - "Chemoprevention:" Nutrients and compounds for cancer prevention. SBIR moves research to private sector. Smoking, Tobacco, and Cancer Program.
1983 - NCI begins chemoprevention and early detection research. Clinical Oncology Program (CCOP) and Division of Cancer Prevention and Control (DCPC) added to NCI.
1984 - DCPC research and clinical trials, meets with Kellogg company to discuss health claims in cereal publicity
1985 - Linxian China Dysplasia trial and ATBC cancer prevention studies
1986 - CCOP expands research to be large scale and include control groups
1987 - NCI guidelines for cervical and breast cancer screenings, cancer prevention fellowship program (CPFP)
1988 - Reagan signs Medicare Catastrophic Coverage Act (mammography screenings)
1989 - MB-CCOP (minority-based community clinical oncology program)
In the 1990s, many chemopreventative clinical trials began recruiting. Often, these studies lasted for more than a decade, so their results would be released in the early 2000s.
1991 - Chemoprevention (synthetic and natural) studies, DCPC + Produce for Better Health Foundation begins 5-A-Day message (fruit and veggie daily servings), ASSIST (smoking) initiative
1992 - Breast Cancer Prevention Trial (BCPT)
1993 - NCI mammography guidelines are dropped (controversy?), prostate lung colorectal, and ovarian cancer screening trial begins (PLCO), FOBT test for CRC mortality, CAPS (colorectal adenoma prevention), enrollment for prostate cancer trial, NCI international breast cancer screening workshop
1994 - ATBC results show causal relationship between beta-carotene and lung cancer incidence in male Fins
1996 - ASCUS/LSIL Triage Study (HPV testing)
1997 - DCP and DCCPS splits from DCPC
1998 - Tamoxifen decreases breast cancer (Fisher?)
1999 - EDRN (early detection research network) and RAPID (access to prevention) established
1999 - Tamoxifen and raloxifene (STAR) clinical trials began, APC (adenoma celecoxib trial)
Due to technological advancements, improved detection of biomarkers, and increased public and governmental support for cancer prevention research, the 21st century brought large improvements in the understanding of cancer genesis and development.
2001 - Selenium and Vitamin E Cancer Prevention Trial (SELECT) Begins Recruiting Men over the age of 55 to test the effectiveness of these two dietary supplements as prostate cancer prevention agents
2002 - Initial Results Released from the ASCUS/LSIL Triage Study (ALTS) on HPV Testing. HPV testing is found not useful for women with low-grade lesions due to the high incidence of HPV in women
2002 - National Lung Screening Trial (NLST) Begins
2002 - Results from the Colorectal Adenoma Prevention Study (CAPS) Released. Results indicate that daily use of aspirin can reduce the development of colorectal tumors by 35% in patients with a pre-existing history of polyps
2003 - Results from the Prostate Cancer Prevention Trial (PCPT) Released
2004 - August: “Decades of Progress 1983 to 2003” Published. The first 20 years of the NCI Community Clinical Oncology Program (CCOP), the precursor to the NCI Community Oncology Research Program (NCORP), are documented
2004 - Adenoma Prevention with Celecoxib (APC) Trial Suspended suspended based on an increased incidence of major cardiovascular events in participants taking celecoxib (Celebrex®)
2005 - Results of the Breast Cancer Prevention Trial (BCPT) Updated. Results show a continued reduction of invasive breast cancer incidence as well as a decrease in some negative side effects, including increased risk of stroke, pulmonary embolism, and deep vein thrombosis
2006 - Initial Results of the Study of Tamoxifen and Raloxifene (STAR) Released. Initial results show that postmenopausal women who are at increased risk of breast cancer can reduce their risk of developing the disease if they take the drug raloxifene
2008 - Initial results from the Selenium and Vitamin E Cancer Prevention Trial (SELECT) Released. Initial results indicate that selenium and vitamin E do not contribute to the prevention of prostate cancer. In fact, test results suggest a slight increase in prostate cancer incidence in subjects taking vitamin E
2009 - Prostate Results from the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial Released. Results show that screening men 55 years of age and older with PSA tests and digital rectal exams was not effective in reducing prostate cancer mortality
2010 - Early Detection Research Network (EDRN) Continues as New Grants Awarded
2010 - Alliance of Glycobiologists for Detection of Cancer Identify Key Antitumor Antibodies. They find that cancer patients produce antibodies that target abnormal proteins with sugar molecules attached made by their tumors, suggesting that antitumor antibodies in the blood may be a source of sensitive biomarkers for cancer detection
2010 - Initial Results of the Lung Cancer Screening Trial (NLST) Released. Initial results show that screening with low-dose helical computerized tomography (CT) reduced lung cancer deaths by about 20% among current and former heavy smokers
2011 - Lung Results from the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial Released
2011 - Ovarian Results from the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial Released. PLCO results show that screening for ovarian cancer with transvaginal ultrasound (TVU) and the CA-125 blood test did not result in fewer deaths from the disease compared with usual care
2012 - Colorectal Results from the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial Released. Results confirm that screening people 55 years of age and older for colorectal cancer using flexible sigmoidoscopy reduces colorectal cancer incidence and mortality
2013 - NCI Community Oncology Research Program (NCORP) Approved for Start, opening the way for the program to bring state-of-the art cancer prevention, control, treatment and imaging clinical trials, cancer care delivery research, and disparities studies to individuals in their own communities
2013 - National Lung Screening Trial (NLST) Researchers Issue Finding on Overdiagnosis
2014 - Prevention of Early Menopause Study (POEMS) Clinical Trial Results Announced
2014 - Selenium and Vitamin E Cancer Prevention Trial (SELECT) Findings Updated. Men who had high levels of selenium at the start of the trial, as assessed by measures of selenium in their toenail clippings, had almost double the chance of developing a high-grade prostate cancer if they took the selenium supplement
2015 - Cancer Prevention and Control Central Institutional Review Board (CIRB) Established
2015 - NCORP Sites Participate in Enrolling Patients in the NCI-MATCH (Molecular Analysis for Therapy Choice) Precision Medicine Trial
2015 - Consortium on Imaging and Biomarkers is Created with Grants to Eight Principal Investigators. The consortium focuses on combining imaging methods with biomarkers to improve the accuracy of screening, early cancer detection, and diagnosis of early stage cancers
2015 - NCI Awards Grants to Create the Consortium for Molecular Characterization of Screen-Detected Lesions
2016 - The White House Announces $1 billion in Investments in the National Cancer Moonshot initiative. Prevention, including cancer vaccine development and early cancer detection, are two of the five opportunity areas
2016 - Ovarian Cancer Study Tests Lead Time of Potential Biomarkers
2016 - Largest Ever US Study to Research Causes and Genetics of Blood Diseases
2016 - Data from the Interactive Diet and Activity Tracking in AARP Study (IDATA) Are Made Available to Qualified Investigators
2016 - Olanzapine Helps Prevent Nausea and Vomiting Caused by Chemotherapy
2016 - Study Confirms Benefits of Early Palliative Care for Advanced Cancer
2016 - Think Tank Emphasizes Identifying and Creating the Next Generation of Community-Based Cancer Prevention Studies
2017 - NCI's Cancer Prevention Fellowship Program (CPFP) Celebrates 30 Years
2017 - NCI Joins Leading Groups on Disparities Statement
2017 - TMIST Trial Aims to Provide Clarity on Breast Cancer Screening Approaches
2017 - Pre-Cancer Atlas and Other Human Tumor Atlas Network Funding Opportunity announcements Released
2017 - Experimental Ovarian Cancer Vaccine Shows Promise in Mice
See also
References
- "Cancer prevention: 7 steps to reduce your risk". Mayo Clinic. 27 September 2008. Retrieved 30 January 2010.
- Valle I, Tramalloni D, Bragazzi NL (June 2015). "Cancer prevention: state of the art and future prospects". Journal of Preventive Medicine and Hygiene. 56 (1): E21–7. PMC 4718348. PMID 26789828.
- "Cancer Prevention & Early Detection Facts & Figures 2017-18" (PDF). Cancer.org. April 1, 2017.
- Danaei G, Vander Hoorn S, Lopez AD, Murray CJ, Ezzati M (2005). "Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors". Lancet. 366 (9499): 1784–93. doi:10.1016/S0140-6736(05)67725-2. PMID 16298215.
- Doll R, Peto R (1981). "The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States today". J. Natl. Cancer Inst. 66 (6): 1191–308. doi:10.1093/jnci/66.6.1192. PMID 7017215.
- Anand P, Kunnumakkara AB, Kunnumakara AB, Sundaram C, Harikumar KB, Tharakan ST, Lai OS, Sung B, Aggarwal BB (2008). "Cancer is a preventable disease that requires major lifestyle changes". Pharm. Res. 25 (9): 2097–116. doi:10.1007/s11095-008-9661-9. PMC 2515569. PMID 18626751.
- "CRISPR Gene-Editing Tool May Help Improve Cancer Immunotherapy". National Cancer Institute. 2017-03-20. Retrieved 2018-03-09.
- "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved 11 November 2009.
- "Cancer Prevention". 2014-02-12.
- Kushi LH, Doyle C, McCullough M, et al. (2012). "American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity". CA Cancer J Clin. 62 (1): 30–67. doi:10.3322/caac.20140. PMID 22237782.
- Wicki A, Hagmann J (September 2011). "Diet and cancer". Swiss Medical Weekly. 141: w13250. doi:10.4414/smw.2011.13250. PMID 21904992.
- Cappellani A, Di Vita M, Zanghi A, Cavallaro A, Piccolo G, Veroux M, Berretta M, Malaguarnera M, Canzonieri V, Lo Menzo E (2012). "Diet, obesity and breast cancer: an update". Front Biosci. 4: 90–108. doi:10.2741/253. PMID 22202045.
- Key TJ (January 2011). "Fruit and vegetables and cancer risk". Br. J. Cancer. 104 (1): 6–11. doi:10.1038/sj.bjc.6606032. PMC 3039795. PMID 21119663.
- Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, Hu FB (July 2014). "Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies". BMJ. 349: g4490. doi:10.1136/bmj.g4490. PMC 4115152. PMID 25073782.
- Larsson SC, Wolk A (May 2007). "Coffee consumption and risk of liver cancer: a meta-analysis". Gastroenterology. 132 (5): 1740–5. doi:10.1053/j.gastro.2007.03.044. PMID 17484871.
- Zheng W, Lee SA (2009). "Well-done meat intake, heterocyclic amine exposure, and cancer risk". Nutr Cancer. 61 (4): 437–46. doi:10.1080/01635580802710741. PMC 2769029. PMID 19838915.
- Ferguson LR (February 2010). "Meat and cancer". Meat Sci. 84 (2): 308–13. doi:10.1016/j.meatsci.2009.06.032. PMID 20374790.
- Moore SC, Lee IM, Weiderpass E, Campbell PT, Sampson JN, Kitahara CM, et al. (June 2016). "Association of Leisure-Time Physical Activity With Risk of 26 Types of Cancer in 1.44 Million Adults". JAMA Internal Medicine. 176 (6): 816–25. doi:10.1001/jamainternmed.2016.1548. PMC 5812009. PMID 27183032.
- Kruk J, Czerniak U (2013). "Physical activity and its relation to cancer risk: updating the evidence". Asian Pacific Journal of Cancer Prevention. 14 (7): 3993–4003. doi:10.7314/APJCP.2013.14.7.3993. PMID 23991944.
- "Exercise Linked With Lower Risk of 13 Types of Cancer". www.cancer.org. Retrieved 2018-03-03.
- "Physical Activity and Cancer". National Cancer Institute. Retrieved 2018-03-03.
- Winzer BM, Whiteman DC, Reeves MM, Paratz JD (June 2011). "Physical activity and cancer prevention: a systematic review of clinical trials". Cancer Causes & Control. 22 (6): 811–26. doi:10.1007/s10552-011-9761-4. PMID 21461921.
- Holland Chp.33
- Rostom A, Dubé C, Lewin G, Tsertsvadze A, Barrowman N, Code C, Sampson M, Moher D (March 2007). "Nonsteroidal anti-inflammatory drugs and cyclooxygenase-2 inhibitors for primary prevention of colorectal cancer: a systematic review prepared for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 146 (5): 376–89. doi:10.7326/0003-4819-146-5-200703060-00010. PMID 17339623.
- Rothwell PM, Fowkes FG, Belch JF, Ogawa H, Warlow CP, Meade TW (January 2011). "Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials". Lancet. 377 (9759): 31–41. doi:10.1016/S0140-6736(10)62110-1. PMID 21144578.
- Cooper K, Squires H, Carroll C, Papaioannou D, Booth A, Logan RF, Maguire C, Hind D, Tappenden P (June 2010). "Chemoprevention of colorectal cancer: systematic review and economic evaluation". Health Technol Assess. 14 (32): 1–206. doi:10.3310/hta14320. PMID 20594533.
- Thomsen A, Kolesar JM (December 2008). "Chemoprevention of breast cancer". Am J Health Syst Pharm. 65 (23): 2221–8. doi:10.2146/ajhp070663. PMID 19020189.
- Wilt TJ, MacDonald R, Hagerty K, Schellhammer P, Kramer BS (2008). Wilt TJ (ed.). "Five-alpha-reductase Inhibitors for prostate cancer prevention". Cochrane Database Syst Rev (2): CD007091. doi:10.1002/14651858.CD007091. PMID 18425978.
- Hen eggs with human proteins offer drug hope
- "Vitamins and minerals: not for cancer or cardiovascular prevention". Prescrire Int. 19 (108): 182. August 2010. PMID 20939459.
- Giovannucci E, Liu Y, Rimm EB, Hollis BW, Fuchs CS, Stampfer MJ, Willett WC (April 2006). "Prospective study of predictors of vitamin D status and cancer incidence and mortality in men". J. Natl. Cancer Inst. 98 (7): 451–9. CiteSeerX 10.1.1.594.1654. doi:10.1093/jnci/djj101. PMID 16595781.
- "Vitamin D Has Role in Colon Cancer Prevention". Archived from the original on 4 December 2006. Retrieved 27 July 2007.
- Schwartz GG, Blot WJ (April 2006). "Vitamin D status and cancer incidence and mortality: something new under the sun". J. Natl. Cancer Inst. 98 (7): 428–30. doi:10.1093/jnci/djj127. PMID 16595770.
- Fritz H, Kennedy D, Fergusson D, Fernandes R, Doucette S, Cooley K, Seely A, Sagar S, Wong R, Seely D (2011). Minna JD (ed.). "Vitamin A and retinoid derivatives for lung cancer: a systematic review and meta analysis". PLoS ONE. 6 (6): e21107. Bibcode:2011PLoSO...6E1107F. doi:10.1371/journal.pone.0021107. PMC 3124481. PMID 21738614.
- Cole BF, Baron JA, Sandler RS, Haile RW, Ahnen DJ, Bresalier RS, McKeown-Eyssen G, Summers RW, Rothstein RI, Burke CA, Snover DC, Church TR, Allen JI, Robertson DJ, Beck GJ, Bond JH, Byers T, Mandel JS, Mott LA, Pearson LH, Barry EL, Rees JR, Marcon N, Saibil F, Ueland PM, Greenberg ER (June 2007). "Folic acid for the prevention of colorectal adenomas: a randomized clinical trial". JAMA. 297 (21): 2351–9. doi:10.1001/jama.297.21.2351. PMID 17551129.
- Vinceti, Marco; Filippini, Tommaso; Del Giovane, Cinzia; Dennert, Gabriele; Zwahlen, Marcel; Brinkman, Maree; Zeegers, Maurice Pa; Horneber, Markus; D'Amico, Roberto (January 2018). "Selenium for preventing cancer". The Cochrane Database of Systematic Reviews. 1: CD005195. doi:10.1002/14651858.CD005195.pub4. ISSN 1469-493X. PMC 6491296. PMID 29376219.
- "Cancer Vaccine Fact Sheet". NCI. 8 June 2006. Archived from the original on 25 October 2008. Retrieved 15 November 2008.
- Lertkhachonsuk AA, Yip CH, Khuhaprema T, Chen DS, Plummer M, Jee SH, Toi M, Wilailak S (2013). "Cancer prevention in Asia: resource-stratified guidelines from the Asian Oncology Summit 2013". Lancet Oncology. 14 (12): e497–507. doi:10.1016/S1470-2045(13)70350-4. PMID 24176569.
- "What's new in cancer immunotherapy research?". www.cancer.org. Retrieved 2018-03-09.
- Pardoll DM (March 2012). "The blockade of immune checkpoints in cancer immunotherapy". Nature Reviews. Cancer. 12 (4): 252–64. doi:10.1038/nrc3239. PMC 4856023. PMID 22437870.
- Banaei, N; et al. (September 2017). "Multiplex detection of pancreatic cancer biomarkers using a SERS-based immunoassay". Nanotechnology. 28 (45): 455101. Bibcode:2017Nanot..28S5101B. doi:10.1088/1361-6528/aa8e8c. PMID 28937361.
- Banaei, N; et al. (January 2019). "Machine learning algorithms enhance the specificity of cancer biomarker detection using SERS-based immunoassays in microfluidic chips". RSC Advances. 9 (4): 1859–1868. doi:10.1039/c8ra08930b.
- "Ages 65 Years and Older: Exams and Screening Tests - ACOG". www.acog.org. Retrieved 2018-04-21.
- Janz T, Lu K, Povlow MR, Urso B (December 2016). "A Review of Colorectal Cancer Detection Modalities, Stool DNA, and Fecal Immunochemistry Testing in Adults Over the Age of 50". Cureus. 8 (12): e931. doi:10.7759/cureus.931. PMC 5235652. PMID 28097082.
- "Cancer Facts & Figures 2018" (PDF).
- "Final Update Summary: Breast Cancer: Screening - US Preventive Services Task Force". www.uspreventiveservicestaskforce.org. Retrieved 2018-04-21.
- "Cancer Prevention & Early Detection Facts & Figures 2017-18" (PDF). Cancer.org. April 1, 2017.
- Schottenfeld D, Beebe-Dimmer JL, Buffler PA, Omenn GS (2013). "Current perspective on the global and United States cancer burden attributable to lifestyle and environmental risk factors". Annu Rev Public Health. 34: 97–117. doi:10.1146/annurev-publhealth-031912-114350. PMID 23514316.
- Shopland DR (1995). "Tobacco use and its contribution to early cancer mortality with a special emphasis on cigarette smoking". Environ. Health Perspect. 103 Suppl 8: 131–42. doi:10.1289/ehp.95103s8131. PMC 1518977. PMID 8741773.
- Parsa N (2012). "Environmental factors inducing human cancers". Iran. J. Public Health. 41 (11): 1–9. PMC 3521879. PMID 23304670.
- Willett WC (1995). "Diet, nutrition, and avoidable cancer". Environ. Health Perspect. 103 Suppl 8: 165–70. doi:10.1289/ehp.95103s8165. PMC 1518978. PMID 8741778.
- Trichopoulou A, Lagiou P, Kuper H, Trichopoulos D (2000). "Cancer and Mediterranean dietary traditions". Cancer Epidemiol. Biomarkers Prev. 9 (9): 869–73. PMID 11008902.
- Song M, Giovannucci E (2016). "Estimating the Influence of Obesity on Cancer Risk: Stratification by Smoking Is Critical". J. Clin. Oncol. 34 (27): 3237–9. doi:10.1200/JCO.2016.67.6916. PMID 27458311.
- World Cancer Research Fund/American Institute for Cancer Research (2009). Policy and Action for Cancer Prevention. Food, Nutrition, and Physical Activity: a Global Perspective. Washington DC, USA: AICR. 2.7.1 Body fatness and foods and drinks that promote weight gain, p. 22. ISBN 978-0-9722522-4-9.CS1 maint: uses authors parameter (link)
- Schottenfeld D, Beebe-Dimmer J (2006). "Chronic inflammation: a common and important factor in the pathogenesis of neoplasia". CA Cancer J Clin. 56 (2): 69–83. doi:10.3322/canjclin.56.2.69. PMID 16514135.
- Tuyns AJ (1979). "Epidemiology of alcohol and cancer". Cancer Res. 39 (7 Pt 2): 2840–3. PMID 445490.
- Irigaray P, Newby JA, Clapp R, Hardell L, Howard V, Montagnier L, Epstein S, Belpomme D (2007). "Lifestyle-related factors and environmental agents causing cancer: an overview". Biomed. Pharmacother. 61 (10): 640–58. doi:10.1016/j.biopha.2007.10.006. PMID 18055160.
- Moore SC, Lee IM, Weiderpass E, Campbell PT, Sampson JN, Kitahara CM, Keadle SK, Arem H, Berrington de Gonzalez A, Hartge P, Adami HO, Blair CK, Borch KB, Boyd E, Check DP, Fournier A, Freedman ND, Gunter M, Johannson M, Khaw KT, Linet MS, Orsini N, Park Y, Riboli E, Robien K, Schairer C, Sesso H, Spriggs M, Van Dusen R, Wolk A, Matthews CE, Patel AV (2016). "Association of Leisure-Time Physical Activity With Risk of 26 Types of Cancer in 1.44 Million Adults". JAMA Intern Med. 176 (6): 816–25. doi:10.1001/jamainternmed.2016.1548. PMC 5812009. PMID 27183032.
- Bode AM, Dong Z (July 2009). "Cancer prevention research - then and now". Nature Reviews. Cancer. 9 (7): 508–16. doi:10.1038/nrc2646. PMC 2838238. PMID 19536108.
- "History/Timeline". Division of Cancer Prevention. 2014-05-09. Archived from the original on 2018-04-28. Retrieved 2018-03-05.
External links
| Wikimedia Commons has media related to Cancer prevention. |