Bloodletting
Bloodletting (or blood-letting) is the withdrawal of blood from a patient to prevent or cure illness and disease. Bloodletting, whether by a physician or by leeches, was based on an ancient system of medicine in which blood and other bodily fluids were regarded as "humours" that had to remain in proper balance to maintain health. It is claimed to have been the most common medical practice performed by surgeons from antiquity until the late 19th century, a span of over 2,000 years.[1] In Europe the practice continued to be relatively common until the end of the 18th century.[2] The practice has now been abandoned by modern-style medicine for all except a few very specific medical conditions.[3] It is conceivable that historically, in the absence of other treatments for hypertension, bloodletting sometimes had a beneficial effect in temporarily reducing blood pressure by reducing blood volume.[4] However, since hypertension is very often asymptomatic and thus undiagnosable without modern methods, this effect was unintentional. In the overwhelming majority of cases, the historical use of bloodletting was harmful to patients.[5]
| Bloodletting | |
|---|---|
.jpg) Bloodletting in 1860, one of only three known photographs of the procedure. | |
| MeSH | D001815 |

Today, the term phlebotomy refers to the drawing of blood for laboratory analysis or blood transfusion.[6] Therapeutic phlebotomy refers to the drawing of a unit of blood in specific cases like hemochromatosis, polycythemia vera, porphyria cutanea tarda, etc., to reduce the number of red blood cells.[7][8] The traditional medical practice of bloodletting is today considered to be a pseudoscience.[9]
In the ancient world
Passages from the Ebers Papyrus may indicate that bloodletting by scarification was an accepted practice in Ancient Egypt.[10][11][12] Egyptian burials have been reported to contain bloodletting instruments.[13] According to some accounts, the Egyptians based the idea on their observations of the Hippopotamus,[14] confusing its red sweat with blood, and believing that it scratched itself to relieve distress.[15][16]
In Greece, bloodletting was in use in the fifth century BC during the lifetime of Hippocrates, who mentions this practice but generally relied on dietary techniques.[17] Erasistratus, however, theorized that many diseases were caused by plethoras, or overabundances, in the blood and advised that these plethoras be treated, initially, by exercise, sweating, reduced food intake, and vomiting.[18] Herophilus advocated bloodletting. Archagathus, one of the first Greek physicians to practice in Rome, also believed in the value of bloodletting.
"Bleeding" a patient to health was modeled on the process of menstruation. Hippocrates believed that menstruation functioned to "purge women of bad humours". During the Roman Empire, the Greek physician Galen, who subscribed to the teachings of Hippocrates, advocated physician-initiated bloodletting.[19]
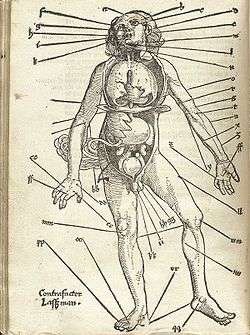
The popularity of bloodletting in the classical Mediterranean world was reinforced by the ideas of Galen, after he discovered that not only veins but also arteries were filled with blood, not air as was commonly believed at the time. There were two key concepts in his system of bloodletting. The first was that blood was created and then used up; it did not circulate, and so it could "stagnate" in the extremities. The second was that humoral balance was the basis of illness or health, the four humours being blood, phlegm, black bile, and yellow bile, relating to the four Greek classical elements of air, water, earth, and fire respectively. Galen believed that blood was the dominant humour and the one in most need of control. In order to balance the humours, a physician would either remove "excess" blood (plethora) from the patient or give them an emetic to induce vomiting, or a diuretic to induce urination.
Galen created a complex system of how much blood should be removed based on the patient's age, constitution, the season, the weather and the place. "Do-it-yourself" bleeding instructions following these systems were developed.[20] Symptoms of plethora were believed to include fever, apoplexy, and headache. The blood to be let was of a specific nature determined by the disease: either arterial or venous, and distant or close to the area of the body affected. He linked different blood vessels with different organs, according to their supposed drainage. For example, the vein in the right hand would be let for liver problems and the vein in the left hand for problems with the spleen. The more severe the disease, the more blood would be let. Fevers required copious amounts of bloodletting.
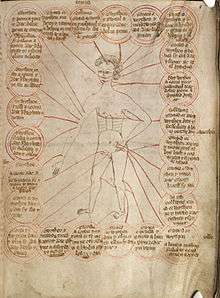
Middle Ages
The Talmud recommended a specific day of the week and days of the month for bloodletting, and similar rules, though less codified, can be found among Christian writings advising which saints' days were favourable for bloodletting. During medieval times bleeding charts were common, showing specific bleeding sites on the body in alignment with the planets and zodiacs.[20] Islamic medical authors also advised bloodletting, particularly for fevers. It was practised according to seasons and certain phases of the moon in the lunar calendar. The practice was probably passed by the Greeks with the translation of ancient texts to Arabic and is different than bloodletting by cupping mentioned in the traditions of Muhammad. When Muslim theories became known in the Latin-speaking countries of Europe, bloodletting became more widespread. Together with cautery, it was central to Arabic surgery; the key texts Kitab al-Qanun and especially Al-Tasrif li-man 'ajaza 'an al-ta'lif both recommended it. It was also known in Ayurvedic medicine, described in the Susruta Samhita.
Use through the 19th century

Even after the humoral system fell into disuse, the practice was continued by surgeons and barber-surgeons. Though the bloodletting was often recommended by physicians, it was carried out by barbers. This led to the distinction between physicians and surgeons. The red-and-white-striped pole of the barbershop, still in use today, is derived from this practice: the red symbolizes blood while the white symbolizes the bandages. Bloodletting was used to "treat" a wide range of diseases, becoming a standard treatment for almost every ailment, and was practiced prophylactically as well as therapeutically.

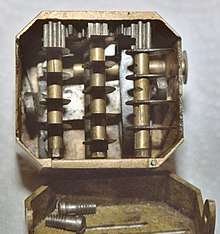

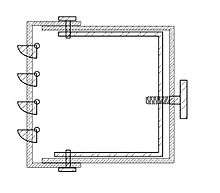
A number of different methods were employed. The most common was phlebotomy, or venesection (often called "breathing a vein"), in which blood was drawn from one or more of the larger external veins, such as those in the forearm or neck. In arteriotomy, an artery was punctured, although generally only in the temples. In scarification (not to be confused with scarification, a method of body modification), the "superficial" vessels were attacked, often using a syringe, a spring-loaded lancet, or a glass cup that contained heated air, producing a vacuum within (see fire cupping). There was also a specific bloodletting tool called a scarificator, used primarily in 19th century medicine. It has a spring-loaded mechanism with gears that snaps the blades out through slits in the front cover and back in, in a circular motion. The case is cast brass, and the mechanism and blades steel. One knife bar gear has slipped teeth, turning the blades in a different direction than those on the other bars. The last photo and the diagram show the depth adjustment bar at the back and sides.
Leeches could also be used. The withdrawal of so much blood as to induce syncope (fainting) was considered beneficial, and many sessions would only end when the patient began to swoon.
William Harvey disproved the basis of the practice in 1628,[2] and the introduction of scientific medicine, la méthode numérique, allowed Pierre Charles Alexandre Louis to demonstrate that phlebotomy was entirely ineffective in the treatment of pneumonia and various fevers in the 1830s. Nevertheless, in 1838, a lecturer at the Royal College of Physicians would still state that "blood-letting is a remedy which, when judiciously employed, it is hardly possible to estimate too highly",[21] and Louis was dogged by the sanguinary Broussais, who could recommend leeches fifty at a time. Some physicians resisted Louis' work because they "were not prepared to discard therapies 'validated by both tradition and their own experience on account of somebody else's numbers'."[22]
Bloodletting was used to treat almost every disease. One British medical text recommended bloodletting for acne, asthma, cancer, cholera, coma, convulsions, diabetes, epilepsy, gangrene, gout, herpes, indigestion, insanity, jaundice, leprosy, ophthalmia, plague, pneumonia, scurvy, smallpox, stroke, tetanus, tuberculosis, and for some one hundred other diseases. Bloodletting was even used to treat most forms of hemorrhaging such as nosebleed, excessive menstruation, or hemorrhoidal bleeding. Before surgery or at the onset of childbirth, blood was removed to prevent inflammation. Before amputation, it was customary to remove a quantity of blood equal to the amount believed to circulate in the limb that was to be removed.[23]
There were also theories that bloodletting would cure "heartsickness" and "heartbreak". A French physician, Jacques Ferrand wrote a book in 1623 on the uses of bloodletting to cure a broken heart. He recommended bloodletting to the point of heart failure (literal).[24]
Leeches became especially popular in the early nineteenth century. In the 1830s, the French imported about forty million leeches a year for medical purposes, and in the next decade, England imported six million leeches a year from France alone. Through the early decades of the century, hundreds of millions of leeches were used by physicians throughout Europe.[25]
Bloodletting was also popular in the young United States of America, where Benjamin Rush (a signatory of the Declaration of Independence) saw the state of the arteries as the key to disease, recommending levels of bloodletting that were high even for the time. George Washington asked to be bled heavily after he developed a throat infection from weather exposure. Within a ten-hour period, a total of 124–126 ounces (3.75 liters) of blood was withdrawn prior to his death from a throat infection in 1799.[27]

One reason for the continued popularity of bloodletting (and purging) was that, while anatomical knowledge, surgical and diagnostic skills increased tremendously in Europe from the 17th century, the key to curing disease remained elusive, and the underlying belief was that it was better to give any treatment than nothing at all. The psychological benefit of bloodletting to the patient (a placebo effect) may sometimes have outweighed the physiological problems it caused. Bloodletting slowly lost favour during the 19th century, after French physician Dr. Pierre Louis conducted an experiment in which he studied the effect of bloodletting on pneumonia patients.[28] A number of other ineffective or harmful treatments were available as placebos—mesmerism, various processes involving the new technology of electricity, many potions, tonics, and elixirs. Yet, bloodletting persisted during the 19th century partly because it was readily available to people of any socioeconomic status.[29]
Controversy and use into the 20th century
Bloodletting gradually declined in popularity over the course of the 19th century, becoming rather uncommon in most places, before its validity was thoroughly debated. In the medical community of Edinburgh, bloodletting was abandoned in practice before it was challenged in theory, a contradiction highlighted by physician-physiologist John Hughes Bennett.[30] Authorities such as Austin Flint I, Hiram Corson, and William Osler became prominent supporters of bloodletting in the 1880s and onwards, disputing Bennett's premise that bloodletting had fallen into disuse because it did not work. These advocates framed bloodletting as an orthodox medical practice, to be used in spite of its general unpopularity.[31] Some physicians considered bloodletting useful for a more limited range of purposes, such as to "clear out" infected or weakened blood or its ability to "cause hæmorrhages to cease"—as evidenced in a call for a "fair trial for blood-letting as a remedy" in 1871.[32]
Some researchers used statistical methods for evaluating treatment effectiveness to discourage bloodletting.[28] But at the same time, publications by Philip Pye-Smith and others defended bloodletting on scientific grounds.[31]
Bloodletting persisted into the 20th century and was recommended in the 1923 edition of the textbook The Principles and Practice of Medicine.[33] The textbook was originally written by Sir William Osler and continued to be published in new editions under new authors following Osler's death in 1919.[34]
Phlebotomy
Bloodletting is used today in the treatment of a few diseases, including hemochromatosis and polycythemia;[35] however, these rare diseases were unknown and undiagnosable before the advent of scientific medicine. It is practiced by specifically trained practitioners in hospitals, using modern techniques, and is also known as a therapeutic phlebotomy. In most cases, phlebotomy now refers to the removal of small quantities of blood for diagnostic purposes. However, in the case of hemochromatosis, bloodletting (by venipuncture) has become the mainstay treatment option.[36][37] In the U.S., according to an academic article posted in the Journal of Infusion Nursing with data published in 2010, the primary use of phlebotomy was to take blood that would one day be reinfused back into a person.[38]
In alternative medicine
Though bloodletting as a general health measure has been shown to be pseudoscience, it is still commonly indicated for a wide variety of conditions in the Ayurvedic, Unani, and traditional Chinese systems of alternative medicine.[39][40][41][42][43][44][45] Unani is based on a form of humorism, and so in that system, bloodletting is used to correct supposed humoral imbalance.
See also
- Hijama
- Fire cupping
- Alternative medicine
- Bloodstopping
- Blood donation
- Hematology
- History of medicine
- Trepanation
- Humorism
- Fleams
- Barber's Pole
- Panacea
References
- "Bloodletting". British Science Museum. 2009. Archived from the original on 2009-04-15. Retrieved 2009-07-12.
- B.) Anderson, Julie, Emm Barnes, and Enna Shackleton. "The Art of Medicine: Over 2,000 Years of Images and Imagination [Hardcover]." The Art of Medicine: Over 2, 000 Years of Images and Imagination: Julie Anderson, Emm Barnes, Emma Shackleton: ISBN 978-0226749365: The Ilex Press Limited, 2013.
- Mestel, Rosie (6 August 2001). "Modern Bloodletting and Leeches". Los Angeles Times. Retrieved 2009-07-12.
- Seigworth, Gilbert R. (1980). "Bloodletting Over the Centuries". New York State Journal of Medicine. PBS. 80 (13): 2022–8. PMID 7010241. Archived from the original on July 5, 2007. Retrieved July 12, 2009.
- "Why fair tests are needed". jameslindlibrary.org. 2009. Archived from the original on January 2, 2007. Retrieved January 8, 2017.
- Phlebotomy (book). Bonnie K. Davis. 2001. ISBN 978-0-7668-2518-5. Retrieved 2009-07-12.
- "The Basis of Therapeutic Phlebotomy". James C. Barton, M.D. 2009. Retrieved 2009-07-12.
- "Therapeutic Phlebotomy". Carteret General Hospital. 2009. Archived from the original on 2009-07-07. Retrieved 2009-07-12.
- Williams, William F. (2013). Encyclopedia of Pseudoscience: From Alien Abductions to Zone Therapy. Routledge. ISBN 978-1135955298.
- Papavramidou, Niki; Thomaidis, Vassilios; Fiska, Aliki (December 2011). "The ancient surgical bloodletting method of arteriotomy". Journal of Vascular Surgery. 54 (6): 1842–44. doi:10.1016/j.jvs.2011.05.100. PMID 21908152.
- Parapia, Liakat Ali (September 2008). "History of bloodletting by phlebotomy". British Journal of Haematology. 143 (4): 490–95. doi:10.1111/j.1365-2141.2008.07361.x. PMID 18783398.
- Schneeberg, NG (December 2002). "A twenty-first century perspective on the ancient art of bloodletting". Transactions & Studies of the College of Physicians of Philadelphia. 24: 157–85. PMID 12800324.
- Stern, Heinrich (1915). Theory and Practice of Bloodletting. New York: Rebman Company. p. 9. Retrieved 20 August 2018.
- Davis, Audrey; Appel, Toby (1979). Bloodletting Instruments in the National Museum of History and Technology. Washington, DC: Smithsonian Institution Press. p. 1. hdl:10088/2440.
- Kean, Sam (2018). "Sweating blood". Distillations. 4 (2): 5. Retrieved August 20, 2018.
- Mikhail, Alan (2014). The Animal in Ottoman Egypt. Oxford: Oxford University Press. p. 169. ISBN 978-0190655228. Retrieved 20 August 2018.
- "Degeneration of Medicine and the Grisly Art of Slicing Open Arms". BBC. 29 November 2002. Retrieved 2009-07-12.
- Encyclopedia of ancient Greece. Nigel Guy Wilson. 2006. ISBN 978-0-415-97334-2. Retrieved 2009-07-12.
- Coutinho, Elsimar M. (1999). Is Menstruation Obsolete?. Oxford University Press. ISBN 0-19-513021-9.
- Conrad, Lawrence I. (1995). The Western Medical Tradition: 800 B.C.–1800 A.D. Cambridge, Eng.: Cambridge UP. ISBN 0-521-38135-5.
- Clutterbuck, Henry (1838). Dr Clutterbuck's Lectures On Bloodletting: Lecture 1. The London Medical Gazette.
- Rangachari, P. K. (1997). "Evidence-based medicine: old French wine with a new Canadian label?". J R Soc Med. 90 (5): 280–84. PMC 1296268.
- Carter (2005) p. 6
- Lydia Kang MD & Nate Pederson, Quackery: A Brief History of the Worst Ways to Cure Everything "Bleed Yourself to Bliss" (Workman Publishing Company; 2017)
- Carter (2005) p. 7
- During the Yellow Fever this practice was also used by Dr. Rush. Read the book Fever 1793 for more info of look up Yellow Fever or Dr. Ben Rush Delpech, M (1825). "Case of a Wound of the Right Carotid Artery". Lancet. 6 (73): 210–13. doi:10.1016/S0140-6736(02)83521-8. quoted in Carter (2005):7–8
- The Permanente Journal Volume 8 No. 2: The asphyxiating and exsanguinating death of president george washington, p. 79, Spring, 2004, retrieved on November 11, 2012
- Greenstone, Gerry (January–February 2010). "The history of bloodletting". British Columbia Medical Journal. 52 (1). Retrieved 2017-02-17.
- Upshaw, John (2000). "The medicinal leech: Past and present". The American Surgeon. 66 (3): 313–14. PMID 10759207.
- Warner, John Harley (July 1980). "Therapeutic explanation and the Edinburgh bloodletting controversy: Two perspectives on the medical meaning of science in the mid-nineteenth century". Medical History. 24 (3): 241–258. doi:10.1017/s0025727300040308. PMC 1082653.
- Anders, Eli Osterweil (2016). "'A Plea for the Lancet': Bloodletting, Therapeutic Epistemology, and Professional Identity in Late Nineteenth-century American Medicine". Social History of Medicine. 29 (4). doi:10.1093/shm/hkw026.
Arguing that it was the physician’s obligation to be active and to intervene when necessary, bloodletting proponents explicitly contrasted themselves with advocates of expectant treatment, whom they portrayed as passive, timid, and unwilling to do what was necessary to save their patients.
- "Bloodletting". British Medical Journal. 1 (533): 283–291. 18 March 1871. doi:10.1136/bmj.1.533.283. PMC 2260507.
- "Bloodletting". UCLA Library: Biomedical Library History and Special Collections for the Sciences. January 12, 2012. Archived from the original on March 13, 2012. Retrieved January 5, 2012.
- Ryan, Terence J (2015). "Osler and his teaching: relevant today". Postgraduate Medical Journal. 91 (1080): 540–41. doi:10.1136/postgradmedj-2015-133677. PMID 26404786.
- Tuttle, Kelly (2012). "Let it bleed". Science History Magazine. 30 (2): 17. Retrieved August 20, 2018.
- Merryweather-Clarke, Alison T.; Worwood, Mark; Parkinson, Lisa; Mattock, Chris; Pointon, Jennifer J.; Shearman, Jeremy D.; Robson, Kathryn J. H. (May 1998). "The effect of HFE mutations on serum ferritin and transferrin saturation in the Jersey population". British Journal of Haematology. 101 (2): 369–73. doi:10.1046/j.1365-2141.1998.00736.x. PMID 9609537.
- Powell, Lawrie W; Seckington, Rebecca C; Deugnier, Yves (2016). "Haemochromatosis". The Lancet. 388 (10045): 706–16. doi:10.1016/s0140-6736(15)01315-x. PMID 26975792.
- Cook, Lynda S. (2010). "Therapeutic Phlebotomy". Journal of Infusion Nursing. 33 (2): 81–88. doi:10.1097/nan.0b013e3181d00010. PMID 20228645.
- Lone AH; Ahmad T; Anwar M; Habib S; Sofi G; Imam H (2011). "Leech therapy – a holistic approach of treatment in unani (greeko-arab) medicine". Anc Sci Life. 31 (1): 31–35. PMC 3377041. PMID 22736888.
- Unani System of Medicine Practice, Globinmed.com.
- Ayurveda – Panchakarma Archived March 30, 2013, at the Wayback Machine, holistic-online.com.
- Ayurveda, Cancer.org.
- Bleeding Peripheral Points: An Acupuncture Technique
- Treating Herpes Zoster (Shingles) with Bloodletting Therapy: Acupuncture and Chinese Medicine Archived 2013-06-04 at the Wayback Machine
- Chen PD, Chen GZ, Xu YX (2011). "Study strategies for bloodletting therapy in treatment of acute soft tissue injuries". Zhong Xi Yi Jie He Xue Bao. 9 (3): 237–41. doi:10.3736/jcim20110302. PMID 21419074.
Books cited
- Carter, K. Codell; Barbara R. Carter (2005). Childbed fever. A scientific biography of Ignaz Semmelweis. Transaction Publishers. ISBN 978-1-4128-0467-7.
- Carter, K. Codell (2012). The Decline of Therapeutic Bloodletting and the Collapse of Traditional Medicine. New Brunswick & London: Transaction Publishers. ISBN 978-1-4128-4604-2.
- Kang, Lydia; Nate Pederson (2017). Quackery: A Brief History of the Worst Ways to Cure Everything. Workman Publishing Company.
Further reading
- McGrew, Roderick. Encyclopedia of Medical History (1985), brief history pp 32–34
External links
| Wikimedia Commons has media related to Bloodletting. |
- Bloodletting Artifacts from the collection of the Waring Historical Library, MUSC
- The History and Progression of Bloodletting
- Medical Antiques: Scarification and Bleeding
- Pictures of antique bloodletting instruments
- PBS's Red Gold: The Story of Blood
- Huge collection of antique bloodletting instruments
- "Breathing a Vein" phisick.com 14 Nov 2011