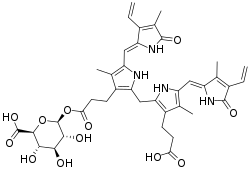
Bilirubin glucuronide
Bilirubin glucuronide is a water-soluble reaction intermediate over the process of conjugation of indirect bilirubin. [1] Bilirubin glucuronide itself belongs to the category of conjugated bilirubin along with bilirubin di-glucuronide.[2] However, only the latter one is primarily excreted into the bile in the normal setting.[2][3][4][5][1][5]
 | |
| Names | |
|---|---|
| IUPAC name
(2S,3S,4S,5R,6S)-6-[3-[2-[[3-(2-Carboxyethyl)-5-[(Z)-(4-ethenyl-3-methyl-5-oxopyrrol-2-ylidene)methyl]-4-methyl-1H-pyrrol-2-yl]methyl]-5-[(Z)-(3-ethenyl-4-methyl-5-oxopyrrol-2-ylidene)methyl]-4-methyl-1H-pyrrol-3-yl]propanoyloxy]-3,4,5-trihydroxyoxane-2-carboxylic acid | |
| Other names
Bilirubin monoglucuronide | |
| Identifiers | |
3D model (JSmol) |
|
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
| KEGG | |
PubChem CID |
|
| |
| |
| Properties | |
| C39H44N4O12 | |
| Molar mass | 760.797 g·mol−1 |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| Infobox references | |
Upon macrophages spot and phagocytize the effete RBC containing hemoglobin[6], unconjugated bilirubin is discharged from macrophages into the blood plasma.[7][8] Most often, the free and water-insoluble unconjugated bilirubin which has an internal hydrodren bonding[9] will bind to albumin and, to a much lesser extent, high density lipoprotein in order to decrease its hydrophobicity and to limit the probability of unnecessary contact with other tissues[1][9] and keep bilirubin in the vascular space from traversing to extravascular space including brain, and from ending up increasing glomerular filtration.[9] Nevertheless, there is still a little portion of indirect bilirubins stays free-of-bound.[9] Free unconjugated bilirubin can poison the cerebrum.[9][10][11][12][13][14][15][16][17][18][19]
Finally, albumin leads the indirect bilirubin to the liver.[1] [9] In the liver sinusoid, albumin disassociates with the indirect bilirubin and returns to the circulation while the hepatocyte transfers the indirect bilirubin to ligandin and glucuronide conjugates the indirect bilirubin in the endoplasmic reticulum by disrupting unconjugated bilirubin's internal hydrogen bonding, which is the thing that makes indirect bilirubin having the property of eternal half-elimination life and insoluble in water[20][9][1][21][22], and by attaching two molecules of glucuronic acid to it in a two step process.[23] The reaction is a transfer of two glucuronic acid groups including UDP glucuronic acid sequentially to the propionic acid groups of the bilirubin, primarily catalyzed by UGT1A1.[23][24][5] In greater detail about this reaction, a glucuronosyl moiety is conjugated to one of the propionic acid side chains, located on the C8 and C12 carbons of the two central pyrrole rings of bilirubin.[25]
When the first step is completely done, the substrate Bilirubin glucuronide (also known as mono-glucuronide[26]) is born at this stage and is water-soluble and readily excreted in bile.[24][9] Thereafter, so long as the second step of attachment of the other glucuronic acid to it succeeds (officially called "re-glucuronidated"[26]), the substrate bilirubin glucuronide will turn into bilirubin di-glucuronide (8,12-diglucuronide[26]) and be excreted into bile canaliculi by way of C-MOAT[note 1] [27][28][29][30] and MRP2[5][31] as normal human bile along with a little amount of unconjugated bilirubin as much as only 1 to 4 percent of total pigments in normal bile.[9][32] That means up to 96%-99% of bilirubin in the bile are conjugated.[9][1]
Normally, there is just a little conjugated bilirubin escapes into the general circulation.[1] Nonetheless, in the setting of severe liver disease, a significantly greater number of conjugated bilirubin will leak into circulation and then dissolve into the blood[note 2] and thereby filtered by the kidney, and only a part of the leaked conjugated bilirubin will be re-absorbed in the renal tubules, the remainder will be present in the urine making it dark-colored.[1][3]
Clinical significance
The clinical significance of bilirubin glucuronide is involved in many conditions. Drugs that inhibit the activities of the components involved in bilirubin metabolism can give rise to accumulation of bilirubin in the blood.[5] In comparison, conjugation of some drugs is also usually impaired if the liver cannot normally metabolite indirect bilirubin.[5]
Renal
When excretion of bilirubin glucuronide by the kidney is detected in the urine through urine examination, meaning that a conspicuous amount of conjugated bilirubin is present and circulating in the blood.[3]
Dubin–Johnson syndrome
In Dubin–Johnson syndrome, impaired biliary excretion of bilirubin glucuronide is due to a mutation in the canalicular multiple drug-resistance protein 2 (MRP2). A darkly pigmented liver is due to polymerized epinephrine metabolites, not bilirubin.[33]
Liver failure or hepatitis
If it is the liver that cannot effectively transfer the indirect bilirubin into bilirubin glucuronide and further into bilirubin di-glucuronide, the consequence will be hyperbilirubinemia or intrahepatic (or hepatocellular) jaundice.[3]
Moreover, the unconjugated hyperbilirubinemia arises in case the components of liver transfer the indirect bilirubin into bilirubin glucuronide in the rate slower than they should be.[3] This condition is associated with either decreased uptake of bilirubin into hepatocytes (Rotor syndrome[34]) or defective intracellular protein binding.[3]
In similar fashion, the conjugated hyperbilirubinemia emerges in case the components of the liver have difficulty turning bilirubin glucuronide into bilirubin di-glucuronide.[3] Note that biliary duct blockage can also lead to conjugated hyperbilirubinemia but the pathophysiology is that backflow of bilirubin di-glucuronide with little indirect bilirubin and bilirubin glucuronide from bile duct through liver into blood plasma.[3][35] These conditions are associated with either defective intracellular protein binding (for the second time) or disturbed secretion into the bile canaliculi (Dubin-Johnson syndrome[34]).[3]
Liver failure and hepatitis are the most etiological in liver-genesis hyperbilirubinemia. [3] In case of hyperbilirubinemia due to intrahepatic or extrahepatic bile ducts blockage, e.g. gallstone, the name is given as Post-hepatic (or obstructive) jaundice.[3]
Bilirubin concentration is not a sensitive early indicator of liver diseases as the liver may have reserved its capacity in the removal of bilirubin to save energy and unreserved the previously reserved capacity when encountering a sudden rise of unconjugated bilirubin.[36] In short, there is still a chance for an ill liver to get rid of excessive unconjugated bilirubin in the blood plasma, displaying a total bilirubin level that is within the normal reference range.[36]
Crigler Najjar disease
In Crigler Najjar disease, there is an inherited deficiency of glucuronyl transferase resulting in high concentrations of unconjugated bilirubin appear in the plasma.[3] Furthermore, those affected may develop kernicterus (deposits of pigment in the brain) that can cause nerve degeneration.[3]
Gilbert’s syndrome
In Gilbert’s syndrome, glucuronyl transferase activity is reduced by approximately 70%, leading to mild accumulation of unconjugated bilirubin in the plasma. [3]
Neonate jaundice
At birth, infants don't develop enough ability to conjugate bilirubin.[37] Up to 8% to 11% neonates will develop hyperbilirubinemia in the first week of their lives. [37][19]
Hemolytic jaundice
In jaundice owing to hemolysis (Pre-hepatic (or hemolytic) jaundice), the pathophysiology is that overproduction of bilirubin from the extravascular or intravascular hemolysis overwhelms the capacity of the liver to excrete it.[3] The bilirubin present in the plasma is largely unconjugated in this setting as they haven't been taken up and conjugated by the liver.[3] In this case, total serum bilirubin increases while the ratio of direct bilirubin to indirect bilirubin remains 96 to 4 as up to 96%-99% of bilirubin in the bile are conjugated mentioned above.[9][1]
Brain damage
Although there were some studies showed an inverse correlation between serum bilirubin level and prevalences of ischemic coronary artery disease[38], cancer mortality[39], or colorectal cancer[40] in general population, the potential benefits of the chemopreventive function of bilirubin and their causative relations haven't been proved.[40][9]
Notes
References
- Divers, Thomas J.; Barton, Michelle Henry (2018). "Disorders of the Liver". Equine Internal Medicine. Elsevier. pp. 843–887. doi:10.1016/b978-0-323-44329-6.00013-9. ISBN 978-0-323-44329-6.
then convert biliverdin to bilirubin and release it from the cell as free, insoluble bilirubin. This form of bilirubin also is referred to as indirect-reacting or unconjugated bilirubin.
- Dubin-Johnson syndrome is associated with inability of the hepatocytes to secrete conjugated bilirubin after it has been formed.
- Smith, Margaret E.; Morton, Dion G. (2010). "Liver and Biliary System". The Digestive System. Elsevier. pp. 85–105. doi:10.1016/b978-0-7020-3367-4.00006-2. ISBN 978-0-7020-3367-4.
- Nishida, T; Gatmaitan, Z; Roy-Chowdhry, J; Arias, I M (1992-11-01). "Two distinct mechanisms for bilirubin glucuronide transport by rat bile canalicular membrane vesicles. Demonstration of defective ATP-dependent transport in rats (TR-) with inherited conjugated hyperbilirubinemia". Journal of Clinical Investigation. American Society for Clinical Investigation. 90 (5): 2130–2135. doi:10.1172/jci116098. ISSN 0021-9738. PMC 443282. PMID 1430236.
- Zhou, J.; Tracy, T. S.; Remmel, R. P. (2010-07-28). "Bilirubin Glucuronidation Revisited: Proper Assay Conditions to Estimate Enzyme Kinetics with Recombinant UGT1A1". Drug Metabolism and Disposition. 38 (11): 1907–1911. doi:10.1124/dmd.110.033829. ISSN 0090-9556. PMC 2967393. PMID 20668247.
- Berk, Paul D.; Howe, Robert B.; Bloomer, Joseph R.; Berlin, Nathaniel I. (1969-11-01). "Studies of bilirubin kinetics in normal adults". The Journal of Clinical Investigation. 48 (11): 2176–2190. doi:10.1172/jci106184. ISSN 0021-9738. PMC 297471. PMID 5824077.
- "Heme metabolism in macrophages". eClinpath. Archived from the original on 2018-05-17. Retrieved 2019-05-05.
- "Bilirubin and hemolytic anemia". eClinpath. Archived from the original on 2018-08-07. Retrieved 2019-05-05.
- Namita Roy-Chowdhury; Jayanta Roy-Chowdhury. Sanjiv Chopra; Elizabeth B Rand; Shilpa Grover (eds.). "Bilirubin metabolism". UpToDate. Archived from the original on 2017-10-24. Retrieved 2019-05-05.
- Shapiro, Steven M. (January 2005). "Definition of the Clinical Spectrum of Kernicterus and Bilirubin-Induced Neurologic Dysfunction (BIND)". Journal of Perinatology. 25 (1): 54–59. doi:10.1038/sj.jp.7211157. PMID 15578034.
- Brites, Dora (2012-05-29). "The Evolving Landscape of Neurotoxicity by Unconjugated Bilirubin: Role of Glial Cells and Inflammation". Frontiers in Pharmacology. 3: 88. doi:10.3389/fphar.2012.00088. ISSN 1663-9812. PMC 3361682. PMID 22661946.
- Wusthoff, Courtney J.; Loe, Irene M. (2015-01-10). "Impact of bilirubin-induced neurologic dysfunction on neurodevelopmental outcomes". Seminars in Fetal & Neonatal Medicine. 20 (1): 52–57. doi:10.1016/j.siny.2014.12.003. ISSN 1744-165X. PMC 4651619. PMID 25585889.
- Radmacher, Paula G; Groves, Frank D; Owa, Joshua A; Ofovwe, Gabriel E; Amuabunos, Emmanuel A; Olusanya, Bolajoko O; Slusher, Tina M (2015-04-01). "A modified Bilirubin-induced neurologic dysfunction (BIND-M) algorithm is useful in evaluating severity of jaundice in a resource-limited setting". BMC Pediatrics. 15 (1): 28. doi:10.1186/s12887-015-0355-2. ISSN 1471-2431. PMC 4389967. PMID 25884571.
- Johnson, Lois; Bhutani, Vinod K. (2011). "The Clinical Syndrome of Bilirubin-Induced Neurologic Dysfunction". Seminars in Perinatology. 35 (3): 101–113. doi:10.1053/j.semperi.2011.02.003. ISSN 0146-0005. PMID 21641482.
- Bhutani, Vinod K.; Wong, Ronald (2015). "Bilirubin-induced neurologic dysfunction (BIND)". Seminars in Fetal and Neonatal Medicine. 20 (1): 1. doi:10.1016/j.siny.2014.12.010. ISSN 1744-165X. PMID 25577656.
- Press, Dove (2018-03-07). "Acute bilirubin encephalopathy and its progression to kernicterus: cur - RRN". Research and Reports in Neonatology. 8: 33–44. doi:10.2147/RRN.S125758. Archived from the original on 2019-05-06. Retrieved 2019-05-06.
- Smith, Margaret E.; Morton, Dion G. (2010). "Liver and Biliary System". The Digestive System. Elsevier. pp. 85–105. doi:10.1016/b978-0-7020-3367-4.00006-2. ISBN 978-0-7020-3367-4.
However, when jaundice is present it is likely that many other potentially toxic materials have also accumulated in the blood as a consequence of their reflux from the bile or impaired secretion from the hepatocyte. This can lead to impaired mental function and malaise.
- Watchko, Jon F.; Tiribelli, Claudio (2013-11-21). Ingelfinger, Julie R. (ed.). "Bilirubin-Induced Neurologic Damage — Mechanisms and Management Approaches". The New England Journal of Medicine. 369 (21): 2021–2030. doi:10.1056/nejmra1308124. ISSN 0028-4793. PMID 24256380.
- Shapiro, Steven M.; Bhutani, Vinod K.; Johnson, Lois (2006). "Hyperbilirubinemia and Kernicterus". Clinics in Perinatology. 33 (2): 387–410. doi:10.1016/j.clp.2006.03.010. ISSN 0095-5108. PMID 16765731.
- Structure of bilirubin Bonnet RJ, Davis E, Hursthouse MB Nature. 1976; 262:326.
- The Liver: Biology and Pathobiology. Hoboken, N.J: Wiley. 2013. ISBN 978-1-119-96422-3. OCLC 899743347.
- "Hereditary Jaundice and Disorders of Bilirubin Metabolism - The Online Metabolic and Molecular Bases of Inherited Disease - McGraw-Hill Medical". OMMBID. 2019-05-06. Retrieved 2019-05-06.
- "Bilirubin". Spencer S. Eccles Health Sciences Library Home Page. 2019-05-06. Archived from the original on 2019-05-06. Retrieved 2019-05-06.
- Bilirubin must be conjugated to a water-soluble substance
- Kadakol, A; Ghosh, SS; Sappal, BS; Sharma, G; Chowdhury, JR; Chowdhury, NR (2000). "Genetic lesions of bilirubin uridine-diphosphoglucuronate glucuronosyltransferase (UGT1A1) causing Crigler-Najjar and Gilbert syndromes: correlation of genotype to phenotype". Human Mutation. 16 (4): 297–306. doi:10.1002/1098-1004(200010)16:4<297::AID-HUMU2>3.0.CO;2-Z. ISSN 1059-7794. PMID 11013440.
- Crawford, JM; Ransil, BJ; Narciso, JP; Gollan, JL (1992-08-25). "Hepatic microsomal bilirubin UDP-glucuronosyltransferase. The kinetics of bilirubin mono- and diglucuronide synthesis". The Journal of Biological Chemistry. 267 (24): 16943–50. ISSN 0021-9258. PMID 1512236.
- Cashore, William J. (2017). "Neonatal Bilirubin Metabolism". Fetal and Neonatal Physiology. Elsevier. pp. 929–933. doi:10.1016/b978-0-323-35214-7.00096-2. ISBN 978-0-323-35214-7.
Conjugated bilirubin is excreted into canalicular bile by way of the canalicular multispecific organic anion transport (C-MOAT) system located in the canalicular membrane within the apical region of the hepatocyte.
- Koike, K; Kawabe, T; Tanaka, T; Toh, S; Uchiumi, T; Wada, M; Akiyama, S; Ono, M; Kuwano, M (1997-12-15). "A canalicular multispecific organic anion transporter (cMOAT) antisense cDNA enhances drug sensitivity in human hepatic cancer cells". Cancer Research. 57 (24): 5475–9. ISSN 0008-5472. PMID 9407953.
- Paulusma, CC; van Geer, MA; Evers, R; Heijn, M; Ottenhoff, R; Borst, P; Oude Elferink, RP (1999-03-01). "Canalicular multispecific organic anion transporter/multidrug resistance protein 2 mediates low-affinity transport of reduced glutathione". Biochemical Journal. 338 (Pt 2): 393–401. doi:10.1042/bj3380393. PMC 1220065. PMID 10024515.
- "Diseases Associated with Hyperbilirubinemia". library.med.utah.edu. 1995-01-05. Archived from the original on 2019-05-06.
- Kamisako, T; Kobayashi, Y; Takeuchi, K; Ishihara, T; Higuchi, K; Tanaka, Y; Gabazza, EC; Adachi, Y (2000). "Recent advances in bilirubin metabolism research: the molecular mechanism of hepatocyte bilirubin transport and its clinical relevance". Journal of Gastroenterology. 35 (9): 659–64. doi:10.1007/s005350070044. ISSN 0944-1174. PMID 11023036. S2CID 25491462.
- Erlinger, Serge; Arias, Irwin M.; Dhumeaux, Daniel (2014). "Inherited Disorders of Bilirubin Transport and Conjugation: New Insights Into Molecular Mechanisms and Consequences". Gastroenterology. 146 (7): 1625–1638. doi:10.1053/j.gastro.2014.03.047. ISSN 0016-5085. PMID 24704527.
- Kumar, Vinay (2007). Robbins Basic Pathology. Elsevier. p. 639.
- van de Steeg, Evita; Stránecký, Viktor; Hartmannová, Hana; Nosková, Lenka; Hřebíček, Martin; Wagenaar, Els; van Esch, Anita; de Waart, Dirk R.; Oude Elferink, Ronald P.J.; Kenworthy, Kathryn E.; Sticová, Eva; al-Edreesi, Mohammad; Knisely, A.S.; Kmoch, Stanislav; Jirsa, Milan; Schinkel, Alfred H. (2012-02-01). "Complete OATP1B1 and OATP1B3 deficiency causes human Rotor syndrome by interrupting conjugated bilirubin reuptake into the liver". The Journal of Clinical Investigation. 122 (2): 519–528. doi:10.1172/jci59526. ISSN 0021-9738. PMC 3266790. PMID 22232210.
- Weiss, Janet S.; Gautam, Anil; Lauff, John J.; Sundberg, Michael W.; Jatlow, Peter; Boyer, James L.; Seligson, David (1983-07-21). "The Clinical Importance of a Protein-Bound Fraction of Serum Bilirubin in Patients with Hyperbilirubinemia". The New England Journal of Medicine. 309 (3): 147–150. doi:10.1056/nejm198307213090305. ISSN 0028-4793. PMID 6866015.
- Raymond, GD; Galambos, JT (1971). "Hepatic storage and excretion of bilirubin in man". The American Journal of Gastroenterology. 55 (2): 135–44. ISSN 0002-9270. PMID 5580257.
- Ullah, S; Rahman, K; Hedayati, M (2016). "Hyperbilirubinemia in Neonates: Types, Causes, Clinical Examinations, Preventive Measures and Treatments: A Narrative Review Article". Iranian Journal of Public Health. 45 (5): 558–568. PMC 4935699. PMID 27398328.
- Breimer, LH; Wannamethee, G; Ebrahim, S; Shaper, AG (1995). "Serum bilirubin and risk of ischemic heart disease in middle-aged British men". Clinical Chemistry. 41 (10): 1504–8. doi:10.1093/clinchem/41.10.1504. ISSN 0009-9147. PMID 7586525.
- Temme, EH; Zhang, J; Schouten, EG; Kesteloot, H (2001). "Serum bilirubin and 10-year mortality risk in a Belgian population". Cancer Causes & Control. 12 (10): 887–94. doi:10.1023/A:1013794407325. ISSN 0957-5243. PMID 11808707.
- Zucker, Stephen D.; Horn, Paul S.; Sherman, Kenneth E. (2004). "Serum bilirubin levels in the U.S. population: Gender effect and inverse correlation with colorectal cancer". Hepatology. 40 (4): 827–835. doi:10.1002/hep.20407. ISSN 0270-9139. PMID 15382174.