Nociception
Nociception (also nocioception, from Latin nocere 'to harm or hurt') is the sensory nervous system's process of encoding noxious stimuli. In nociception, intense chemical (e.g., cayenne powder), mechanical (e.g., cutting, crushing), or thermal (heat and cold) stimulation of sensory nerve cells called nociceptors produces a signal that travels along a chain of nerve fibers via the spinal cord to the brain.[1] Nociception triggers a variety of physiological and behavioral responses and usually results in a subjective experience, or perception, of pain in sentient beings.[2]
Detection of noxious stimuli
Potentially damaging mechanical, thermal, and chemical stimuli are detected by nerve endings called nociceptors, which are found in the skin, on internal surfaces such as the periosteum, joint surfaces, and in some internal organs. Some nociceptors are unspecialized free nerve endings that have their cell bodies outside the spinal column in the dorsal root ganglia.[3] Other nociceptors rely on specialised structures in the skin to transduce noxious information such as nociceptive schwann cells.[4] Nociceptors are categorized according to the axons which travel from the receptors to the spinal cord or brain. After nerve injury it is possible for touch fibres that normally carry non-noxious stimuli to be perceived as noxious.[5]
Nociceptors have a certain threshold; that is, they require a minimum intensity of stimulation before they trigger a signal. Once this threshold is reached a signal is passed along the axon of the neuron into the spinal cord.
Nociceptive threshold testing deliberately applies a noxious stimulus to a human or animal subject in order to study pain. In animals, the technique is often used to study the efficacy of analgesic drugs and to establish dosing levels and period of effect. After establishing a baseline, the drug under test is given and the elevation in threshold recorded at specified time points. When the drug wears off, the threshold should return to the baseline (pre-treatment) value.
In some conditions, excitation of pain fibers becomes greater as the pain stimulus continues, leading to a condition called hyperalgesia.
Theory
Consequences
Nociception can also cause generalized autonomic responses before or without reaching consciousness to cause pallor, sweating, tachycardia, hypertension, lightheadedness, nausea and fainting.[6]
System overview
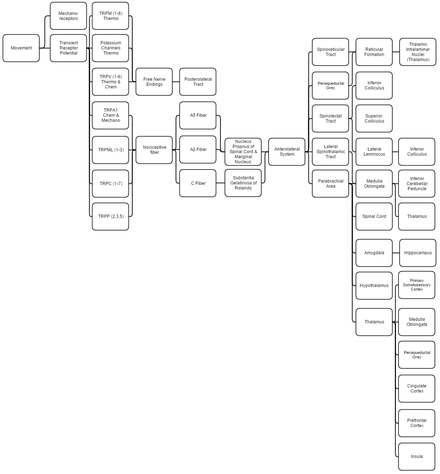
This overview discusses proprioception, thermoception, chemoception and nociception as they are all integrally connected.
Mechanical
Proprioception is determined by using standard mechanoreceptors (especially ruffini corpuscles (stretch) and transient receptor potential (TRP) channels). Proprioception is completely covered within the somatosensory system as the brain processes them together.
Thermoception refers to stimuli of moderate temperatures 24–28 °C (75–82 °F), as anything beyond that range is considered pain and moderated by nociceptors. TRP and potassium channels [TRPM (1-8), TRPV (1-6), TRAAK, and TREK] each respond to different temperatures (among other stimuli) which create action potentials in nerves which join the mechano (touch) system in the posterolateral tract. Thermoception, like proprioception, is then covered by the somatosensory system.[7][8][9][10][11]
TRP channels that detect noxious stimuli (mechanical, thermal, and chemical pain) relay that info to nociceptors that generate an action potential. Mechanical TRP channels react to depression of their cells (like touch), thermal TRP change shape in different temperatures, and chemical TRP act like taste buds, signalling if their receptors bond to certain elements/chemicals.
Neural
- Laminae 3-5 make up nucleus proprius in spinal grey matter.
- Lamina 2 makes up substantia gelatinosa of Rolando, unmyelinated spinal grey matter. Substantia receives input from nucleus proprius and conveys intense, poorly localized pain.
- Lamina 1 primarily project to the parabrachial area and periaqueductal grey, which begins the suppression of pain via neural and hormonal inhibition. Lamina 1 receive input from thermoreceptors via the posterolateral tract. Marginal nucleus of the spinal cord are the only unsuppressible pain signals.
- The parabrachial area integrates taste and pain info, then relays it. Parabrachial checks if the pain is being received in normal temperatures and if the gustatory system is active; if both are so the pain is assumed to be due to poison.
- Ao fibers synapse on laminae 1 and 5 while Ab synapses on 1, 3, 5, and C. C fibers exclusively synapse on lamina 2.[12][13]
- The amygdala and hippocampus create and encode the memory and emotion due to pain stimuli.
- The hypothalamus signals for the release of hormones that make pain suppression more effective; some of these are sex hormones.
- Periaqueductal grey (with hypothalamic hormone aid) hormonally signals reticular formation’s raphe nuclei to produce serotonin that inhibits laminae pain nuclei.[14]
- Lateral spinothalamic tract aids in localization of pain.
- Spinoreticular and spinotectal tracts are merely relay tracts to the thalamus that aid in the perception of pain and alertness towards it. Fibers cross over (left becomes right) via the spinal anterior white commissure.
- Lateral lemniscus is the first point of integration of sound and pain information.[15]
- Inferior colliculus (IC) aids in sound orienting to pain stimuli.[16]
- Superior colliculus receives IC’s input, integrates visual orienting info, and uses the balance topographical map to orient the body to the pain stimuli.[17][18]
- Inferior cerebellar peduncle integrates proprioceptive info and outputs to the vestibulocerebellum. The peduncle is not part of the lateral-spinothalamic-tract-pathway; the medulla receives the info and passes it onto the peduncle from elsewhere (see somatosensory system).
- The thalamus is where pain is thought to be brought into perception; it also aids in pain suppression and modulation, acting like a bouncer, allowing certain intensities through to the cerebrum and rejecting others.[19]
- The somatosensory cortex decodes nociceptor info to determine the exact location of pain and is where proprioception is brought into consciousness; inferior cerebellar peduncle is all unconscious proprioception.
- Insula judges the intensity of the pain and provides the ability to imagine pain.[20][21]
- Cingulate cortex is presumed to be the memory hub for pain.[22]
In non-mammalian animals
Nociception has been documented in non-mammalian animals, including fish[23] and a wide range of invertebrates,[24] including leeches,[25] nematode worms,[26] sea slugs,[27] and fruit flies.[28] As in mammals, nociceptive neurons in these species are typically characterized by responding preferentially to high temperature (40° Celsius or more), low pH, capsaicin, and tissue damage.
History of term
The term "nociception" was coined by Charles Scott Sherrington to distinguish the physiological process (nervous activity) from pain (a subjective experience).[29] It is derived from the Latin verb "nocēre", which means "to harm".
References
- Portenoy, Russell K.; Brennan, Michael J. (1994). "Chronic Pain Management". In Good, David C.; Couch, James R. (eds.). Handbook of Neurorehabilitation. Informa Healthcare. ISBN 978-0-8247-8822-3.
- Bayne, Kathryn (2000). "Assessing Pain and Distress: A Veterinary Behaviorist's Perspective". Definition of Pain and Distress and Reporting Requirements for Laboratory Animals: Proceedings of the Workshop Held June 22, 2000. National Academies Press. pp. 13–21. ISBN 978-0-309-17128-1.
- Purves, D. (2001). "Nociceptors". In Sunderland, MA. (ed.). Neuroscience. Sinauer Associates.
- Doan, Ryan A.; Monk, Kelly R. (16 August 2019). "Glia in the skin activate pain responses". Science. 365 (6454): 641–642. doi:10.1126/science.aay6144. ISSN 1095-9203. PMID 31416950.
- Dhandapani, Rahul; Arokiaraj, Cynthia Mary; Taberner, Francisco J.; Pacifico, Paola; Raja, Sruthi; Nocchi, Linda; Portulano, Carla; Franciosa, Federica; Maffei, Mariano; Hussain, Ahmad Fawzi; de Castro Reis, Fernanda (2018-04-24). "Control of mechanical pain hypersensitivity in mice through ligand-targeted photoablation of TrkB-positive sensory neurons". Nature Communications. 9 (1): 1–14. doi:10.1038/s41467-018-04049-3. ISSN 2041-1723.
- Feinstein, B.; Langton, J. N. K.; Jameson, R. M.; Schiller, F. (October 1954). "Experiments on pain referred from deep somatic tissues". The Journal of Bone & Joint Surgery. 36 (5): 981–997. doi:10.2106/00004623-195436050-00007. PMID 13211692.
- McCann, Stephanie (2017). Kaplan Medical Anatomy Flashcards: Clearly Labeled, Full-Color Cards. KAPLAN. ISBN 978-1-5062-2353-7.
- Albertine, Kurt. Barron’s Anatomy Flash Cards
- Hofmann, Thomas; Schaefer, Michael; Schultz, Günter; Gudermann, Thomas (28 May 2002). "Subunit composition of mammalian transient receptor potential channels in living cells". Proceedings of the National Academy of Sciences. 99 (11): 7461–7466. Bibcode:2002PNAS...99.7461H. doi:10.1073/pnas.102596199. PMC 124253. PMID 12032305.
- Noël, Jacques; Zimmermann, Katharina; Busserolles, Jérome; Deval, Emanuel; Alloui, Abdelkrim; Diochot, Sylvie; Guy, Nicolas; Borsotto, Marc; Reeh, Peter; Eschalier, Alain; Lazdunski, Michel (12 March 2009). "The mechano-activated K+ channels TRAAK and TREK-1 control both warm and cold perception". The EMBO Journal. 28 (9): 1308–1318. doi:10.1038/emboj.2009.57. PMC 2683043. PMID 19279663.
- Scholz, Joachim; Woolf, Clifford J. (November 2002). "Can we conquer pain?". Nature Neuroscience. 5 (11): 1062–1067. doi:10.1038/nn942. PMID 12403987.
- Braz, Joao M.; Nassar, Mohammed A.; Wood, John N.; Basbaum, Allan I. (September 2005). "Parallel 'Pain' Pathways Arise from Subpopulations of Primary Afferent Nociceptor". Neuron. 47 (6): 787–793. doi:10.1016/j.neuron.2005.08.015. PMID 16157274.
- Brown, A. G. (2012). Organization in the Spinal Cord: The Anatomy and Physiology of Identified Neurones. Springer Science & Business Media. ISBN 978-1-4471-1305-8.
- van den Pol, Anthony N. (15 April 1999). "Hypothalamic Hypocretin (Orexin): Robust Innervation of the Spinal Cord". The Journal of Neuroscience. 19 (8): 3171–3182. doi:10.1523/JNEUROSCI.19-08-03171.1999.
- Bajo, Victoria M.; Merchán, Miguel A.; Malmierca, Manuel S.; Nodal, Fernando R.; Bjaalie, Jan G. (10 May 1999). "Topographic organization of the dorsal nucleus of the lateral lemniscus in the cat". The Journal of Comparative Neurology. 407 (3): 349–366. doi:10.1002/(SICI)1096-9861(19990510)407:3<349::AID-CNE4>3.0.CO;2-5. PMID 10320216.
- Oliver, Douglas L. (2005). "Neuronal Organization in the Inferior Colliculus". The Inferior Colliculus. pp. 69–114. doi:10.1007/0-387-27083-3_2. ISBN 0-387-22038-0.
- Corneil, Brian D.; Olivier, Etienne; Munoz, Douglas P. (1 October 2002). "Neck Muscle Responses to Stimulation of Monkey Superior Colliculus. I. Topography and Manipulation of Stimulation Parameters". Journal of Neurophysiology. 88 (4): 1980–1999. doi:10.1152/jn.2002.88.4.1980. PMID 12364523.
- May, Paul J. (2006). "The mammalian superior colliculus: Laminar structure and connections". Neuroanatomy of the Oculomotor System. Progress in Brain Research. 151. pp. 321–378. doi:10.1016/S0079-6123(05)51011-2. ISBN 9780444516961. PMID 16221594.
- Benevento, Louis A.; Standage, Gregg P. (1 July 1983). "The organization of projections of the retinorecipient and nonretinorecipient nuclei of the pretectal complex and layers of the superior colliculus to the lateral pulvinar and medial pulvinar in the macaque monkey". The Journal of Comparative Neurology. 217 (3): 307–336. doi:10.1002/cne.902170307. PMID 6886056.
- Sawamoto, Nobukatsu; Honda, Manabu; Okada, Tomohisa; Hanakawa, Takashi; Kanda, Masutaro; Fukuyama, Hidenao; Konishi, Junji; Shibasaki, Hiroshi (1 October 2000). "Expectation of Pain Enhances Responses to Nonpainful Somatosensory Stimulation in the Anterior Cingulate Cortex and Parietal Operculum/Posterior Insula: an Event-Related Functional Magnetic Resonance Imaging Study". The Journal of Neuroscience. 20 (19): 7438–7445. doi:10.1523/JNEUROSCI.20-19-07438.2000.
- Menon, Vinod; Uddin, Lucina Q. (29 May 2010). "Saliency, switching, attention and control: a network model of insula function". Brain Structure and Function. 214 (5–6): 655–667. doi:10.1007/s00429-010-0262-0. PMC 2899886. PMID 20512370.
- Shackman, Alexander J.; Salomons, Tim V.; Slagter, Heleen A.; Fox, Andrew S.; Winter, Jameel J.; Davidson, Richard J. (March 2011). "The integration of negative affect, pain and cognitive control in the cingulate cortex". Nature Reviews Neuroscience. 12 (3): 154–167. doi:10.1038/nrn2994. PMC 3044650. PMID 21331082.
- Sneddon, L. U.; Braithwaite, V. A.; Gentle, M. J. (2003). "Do fishes have nociceptors? Evidence for the evolution of a vertebrate sensory system". Proceedings of the Royal Society B. 270 (1520): 1115–1121. doi:10.1098/rspb.2003.2349. PMC 1691351. PMID 12816648.
- Jane A. Smith (1991). "A Question of Pain in Invertebrates". Institute for Laboratory Animals Journal. 33 (1–2).
- Pastor, J.; Soria, B.; Belmonte, C. (1996). "Properties of the nociceptive neurons of the leech segmental ganglion". Journal of Neurophysiology. 75 (6): 2268–2279. doi:10.1152/jn.1996.75.6.2268. PMID 8793740.
- Wittenburg, N.; Baumeister, R. (1999). "Thermal avoidance in Caenorhabditis elegans: an approach to the study of nociception". PNAS. 96 (18): 10477–10482. Bibcode:1999PNAS...9610477W. doi:10.1073/pnas.96.18.10477. PMC 17914. PMID 10468634.
- Illich, P. A.; Walters, E. T. (1997). "Mechanosensory neurons innervating Aplysia siphon encode noxious stimuli and display nociceptive sensitization". Journal of Neuroscience. 17 (1): 459–469. doi:10.1523/JNEUROSCI.17-01-00459.1997. PMC 6793714. PMID 8987770.
- Tracey, W.Daniel; Wilson, Rachel I; Laurent, Gilles; Benzer, Seymour (April 2003). "painless, a Drosophila Gene Essential for Nociception". Cell. 113 (2): 261–273. doi:10.1016/s0092-8674(03)00272-1. PMID 12705873.
- Sherrington, C. (1906). The Integrative Action of the Nervous System. Oxford: Oxford University Press.