Intermammary cleft
The intermammary cleft or intermammary sulcus or sulcus intermammarius is a surface feature of males and females that marks the division in the chest of the two breasts.[1] The International Federation of Associations of Anatomists (IFAA) uses the terms "sulcus intermammarius" or "intermammary cleft"[2] when referring to the area between the breasts.[3][4] In the surgical parlance the cleavage or intermammary cleft is also known as medial difinition[5] or medial fold[6] of breasts. In popular usage the area is commonly referred to as a woman's cleavage. An imaginary line between the nipples that crosses the intermammary cleft, serving as a landmark for some CPR procedures, is known as the intermammary line.[7]
| Intermammary cleft | |
|---|---|
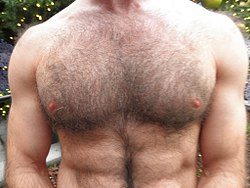 Intermammary cleft dividing the breasts | |
| Details | |
| Identifiers | |
| Latin | sulcus intermammarius |
| TA | A16.0.02.002 |
| FMA | 55264 |
| Anatomical terminology | |
Anatomy
The intermammary cleft is delineated by where each breast sits in relationship to the sternum (or breastbone),[8] dividing the two breasts.[9][10][11] Anatomically the width of a cleavage is determined at the point where the breast tissue attach to the periosteal bone membrane that covers the sternum. It is also defined by the medial attachments of the pectoralis major (chest muscle).[4]
The sternal side (towards the breastbone) of pectoralis major is distinct from the clavicular (towards the collarbone) side, and the two are separated by a fascial interval.[12] The sternal side is usually more robust and has a fiber orientation that best emulates the downward pull of the subscapularis muscle (armpit muscle).[13]
At the midline of the breast – the intermammary cleft – a deep layer of superficial fascia (lowermost layer of the skin) is firmly attached to the pectoral fascia (outer side of chest muscles) and the periosteum (bone membrane) of the sternum. It forms a shelving edge that supports the breasts.[14]
A ligamentous structure of dense Cooper's ligaments is medially inserted into the skin overlying the sternum determining the shape of the breasts and intermammary sulcus.[15] These ligaments are helpful in supporting the breasts in an youthful disposition, and loss of elasticity or attenuation of these ligaments results in ptosis (sagging) of breasts.[16][17]
Lymph vessels originating at the base of the nipples can ventrally extend as far as the intermammary cleft,[18] and to the opposite breast.[1] The intermammary lymphatics begin as a bunch of small channels consisting of a single layer of epithelium supported by stroma. Each mesh of this network surrounds one or more of the ultimate lobules of the glands, and receives its lymph from the interacinous spaces between the acini of glands.[19] The medial breast, along with the inferior breast, is supplied by 2nd–6th branches of intercostal nerves.[20]
Clinical conditions
Poikiloderma of Civatte, a condition of dilated blood vessels and red to red-brown spots, is common to upper part of the cleavage, especially for those who wear sports bras or push-up bras for prolonged periods, and commonly affects fair skinned middle-aged to elderly women.[21][22] It is characterized by hypopigmentation, hyperpigmentation, telangiectasias and superficial skin atrophy (occasional itching is reported), is another condition caused by long exposure to sunlight.[23][24] Poikiloderma and Dermatoheliosis are treated by desquamation (skin peeling).[21][23]
Hidradenitis suppurativa (HS) is a non-contagious chronic skin disease affects intertriginous skin of apocrine sweat gland bearing areas like inframammary fold, and intermammary sulcus. It is characterized by clusters of abscesses, epidermoid cysts, sebaceous cysts, pilonidal cysts.[25][26] There is no single effective treatment for HS. The recommended treatments include antibiotics, antiandrogens, corticosteroids, ciclosporins, and TNF inhibitors.[26]
Tinea versicolor is a condition characterized by pinhead to coin sized eruptions on the body trunk and proximal extremities, often affecting the breast cleavage as a narrow band of lesions.[27][28] The majority of tinea versicolor is caused by the fungus Malassezia globosa, although Malassezia furfur is responsible for a small number of cases.[29][30] Topical antifungal medications containing selenium sulfide are often recommended to treat tinea versicolor.[31]
Intermammary cleft can get attacked by plaque type psoriasis, which can in turn can cause erythematosus.[32] Prurigo pigmentosa is a rare skin condition of unknown cause that affects depressed places on chest and back like the intermammary area. It is characterized by the sudden onset of erythematous papules that leave a reticulated hyperpigmentation when they heal.[33][34] Confluent and reticulated papillomatosis, characterized by asymptomatic, small, red to brown, slightly verrucous papules occurs on upper torso, the cleavage area and back.[35] Granular Parakeratosis, though mostly an ailment of the armpit area, is also found on the cleavage.[36]
See also
References
- Moore, Keith (2018). Clinically oriented anatomy (Eighth ed.). p. 318–321. ISBN 9781496347213.
- Sulcus Intermammarius, Université de Fribourg/IFAA
- Keith L. Moore, Anne M.R. Agur and Arthur F. Daley, Essential Clinical Anatomy (4th edition), page 49, Lippincott Williams and Wilkins, 2010, ISBN 9780781799157
- Muhammad Adil Abbas Khan, Ammar Asrar Javed and Nigel Mercer, Cleavage classification: categorizing a vital feminine aesthetic landmark, Plastic and Aesthetic Research (PAR), 016-01-15
- John Bostwick, Plastic and Reconstructive Breast Surgery (volume 1), page 21, Quality Medical Pub, 2000, ISBN 9781576261040
- Sylvia H. Heywang-Koebrunner, Ingrid Schreer and Susan Barter, Diagnostic Breast Imaging, page 62, Thieme, 2019, ISBN 9783131504111
- King, Christopher; Henretig, Fred M. (2008). "Textbook of Pediatric Emergency Procedures". Lippincott Williams & Wilkins. Retrieved 19 July 2020.
- Dr. Ted Eisenberg and Joyce K. Eisenberg, The Scoop on Breasts: A Plastic Surgeon Busts the Myths, Incompra Press, 2012, ISBN 978-0-9857249-3-1
- Heide Schatten and Gheorghe M. Constantinescu, Comparative Reproductive Biology, page 17, John Wiley & Sons, 2008, ISBN 978-0-470-39025-2
- Genaro Andres Contreras, The Use of Tylosin to Treat Intramammary Infections , page 22, ProQuest, 2008, ISBN 978-0-549-60762-5
- Olufunmilayo I. Olopade and Carla I. Falkson, Breast Cancer in Women of African Descent, page 125, Springer Science & Business Media, 2010, ISBN 9781402036644
- William C. Wood, Charles Staley and John E. Skandalakis, Anatomic Basis of Tumor Surgery, page 140, Springer Science & Business Media, 2010, ISBN 9783540741770
- Neal S. Elattrache, Surgical Techniques in Sports Medicine, page 139, Lippincott Williams & Wilkins, 2007, ISBN 9780781754279
- John Blair Deaver, The Breast: its anomalies, its diseases, and their treatment, page 30, P. Blakiston's Son & Company, 1917, ISBN 9780266616542
- Elizabeth Hall-Findlay and Gregory Evans, Aesthetic and Reconstructive Surgery of the Breast, Elsevier Health Sciences, 2010, ISBN 9780702050091
- Maurice Y Nahabedian and Peter C. Neligan, Plastic Surgery (Volume 5), page 89, Elsevier Health Sciences, 2017, ISBN 9780323357104
- Jeffrey Weinzweig, Plastic Surgery Secrets, page 453, Elsevier Health Sciences, 2010, ISBN 9780323085908
- Charles Wesley Turner, The mammary gland (vol. 1), page 80, Lucas Bros., 1952
- Albert Henry Buck and Thomas Lathrop Stedman, A Reference Handbook of the Medical Sciences (volume 2), W. Wood, 1901
- Heinz Bohmert, Christian J. Gabka and John Bostwick, Plastic and Reconstructive Surgery of the Breast: A Surgical Atlas, page 4, Thieme, 1997, ISBN 9780865776289
- Daphne Merkin, "The Great Divide", New York Times, August 28, 2005
- Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.CS1 maint: multiple names: authors list (link)
- Alam, Murad; Pongprutthipan, Marisa (2010). Body Rejuvenation. Springer Science+Business Media. p. 39. ISBN 9781441910936.
- American Osteopathic College of Dermatology "Dermatologic Disease Database", aocd.org, referenced July 22, 2011.
- Alikhan, Ali; Lynch, Eisen (2009). "Hidradenitis suppurativa: a comprehensive review". J Am Acad Derm. 60 (4): 539–561. doi:10.1016/j.jaad.2008.11.911. PMID 19293006.
- Faye Lyons, Dermatology for the Advanced Practice Nurse, pages 118-121, Springer Publishing Company, 2014, ISBN 9780826136435
- Rapini, Ronald P; Bolognia, Jean L.; Jorizzo, Joseph L (2007). Dermatology: 2-Volume Set. St Louis: Mosby. pp. Chapter 76. ISBN 1-4160-2999-0.
- James Nevins Hyde, A Practical treatise on diseases of the skin, pages 625-626, Lea Bros. & Company, 1888
- Morishita N; Sei Y. (December 2006). "Microreview of pityriasis versicolor and Malassezia species". Mycopathologia. 162 (6): 373–76. doi:10.1007/s11046-006-0081-2.
- Prohic A; Ozegovic L. (January 2007). "Malassezia species isolated from lesional and non-lesional skin in patients with pityriasis versicolor". Mycoses. 50 (1): 58–63. doi:10.1111/j.1439-0507.2006.01310.x. PMID 17302750.
- Likness, LP (June 2011). "Common dermatologic infections in athletes and return-to-play guidelines". The Journal of the American Osteopathic Association. 111 (6): 373–379. doi:10.7556/jaoa.2011.111.6.373. PMID 21771922.
- Alan Menter and Benjamin Stoff, Psoriasis, page 25, CRC Press, 2010, ISBN 9781840765908
- James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). page 57, Saunders. ISBN 0-7216-2921-0.
- Q Ashton Acton, Issues in Dermatology and Cosmetic Medicine (2013 Edition), page 432, Scholarly Editions, 2013, ISBN 9781490109114
- David Weedon, Weedon's Skin Pathology, page 505, Elsevier Health Sciences, 2009, ISBN 9780702047749
- J Lazar and Phillip H. McKee, Pathology of the Skin, page 96, Elsevier Health Sciences, 2011, ISBN 9780723437185
.png)
