High-grade serous carcinoma
High-grade serous carcinoma (HGSC) is a type of tumour that arises from the serous epithelial layer in the abdominopelvic cavity and is mainly found in the ovary. HGSCs make up the majority of ovarian cancer cases[1] and have the lowest survival rates.[2] HGSC is distinct from low-grade serous carcinoma (LGSC) which arises from ovarian tissue, is less aggressive and is present in stage I ovarian cancer where tumours are localised to the ovary.
| High-grade serous carcinoma | |
|---|---|
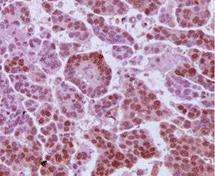 | |
| Immunohistochemistry micrograph of androgen receptors on a HGSC tumour sample |
Although originally thought to arise from the squamous epithelial cell layer covering the ovary, HGSC is now thought to originate in the Fallopian tube epithelium. HGSC is much more invasive than LGSC with a higher fatality rate - although it is more sensitive to platinum-based chemotherapy,[3][4] possibly due to its rapid growth rate. In rare cases, HGSCs can develop from LGSCs,[5][6] but generally the two types arise independently of each other.
Risk factors
Environmental risk factors
The ‘incessant ovulation’ theory is suggested by the strong correlation between the number of ovulatory cycles of an individual and their risk of ovarian cancer.[7]
This trend is reflected in the protective effects of pregnancy, parity and breastfeeding against ovarian cancer,[8][9] and similar findings in epidemiological studies that have indicated a reduction of risk associated with use of oral contraceptive pills.[10][7]
Ovulation is accepted as the cause of ovarian cortical inclusion cysts, the precursor lesions of serous carcinomas, and lower numbers of these cortical inclusion cysts are thought to be the mechanism by which reducing lifetime ovulations can lower the risk of developing HGSC.[11]
Conversely, a temporal association with menopausal hormone therapy and incidence of HGSC was found,[12] and polycystic ovarian syndrome (PCOS) was shown to contribute to a doubling of the risk of ovarian cancer.[13]
Endometriosis can increase risk for other ovarian cancer subtypes, but is not associated with HGSC.[14]
Genetic risk factors
More than 20% of ovarian cancer tumours have hereditary origin. The majority of these feature mutations in the tumour suppressor BRCA genes, which tend to give rise to HGSC.[15] A mutation in BRCA1 or BRCA2 can confer a lifetime ovarian cancer risk of 40-50% and 10-20% respectively,[16] with BRCA2 mutations strongly associated with better clinical outcomes.
A specific tumour protein 53 (TP53) expression pattern in the Fallopian tube epithelium – the ‘p53 signature’ - is thought to be a precursor marker of HGSC. TP53-/- mice (in which the TP53 gene has been deleted) do not develop ovarian carcinomas.[17] However, TP53 mutations were found in 96% of HGSC cases.[18] A local abnormal TP53 expression may thus be indicative of HGSC.[19] In women, pelvic HGSC show either a complete absence of P53 expression, or overexpression, suggesting that any aberration of P53 leads to tumour development.[20] Additionally, overexpression of TP53 is associated with better clinical outcome whereas an absence of the p53 protein is linked to an increased risk of HGSC tumour recurrence.[20]
A recent mouse model suggest that a p53 mutation may induce HGSC arising from the ovary rather than the Fallopian tube.[21]
Pathophysiology
Cell origin
HGSC are further distinguished from LGSC by ‘type I/II’ ovarian tumour nomenclature;[22] type I referring to tumour types (e.g. LGSCs) where precursor lesions within the ovary have been characterised, and type II referring to tumour types (e.g. HGSCs) without association of such lesions, tumours understood to develop de novo from the tubal and/or ovarian surface epithelium. This classification has more relevance to research rather than to clinical practice.[23]
The serous membrane is a particular type of secretory epithelium which covers organs in body cavities and secretes serous fluid to reduce friction from muscle movement. Serous membrane lining the abdominopelvic cavity is called the peritoneum; that lining heart and mediastinum is the pericardium, and that lining the thoracic cavity and lungs is the pleura. Technically a ‘serous carcinoma’ can occur anywhere on these membranes, but high-grade serous carcinoma is generally limited to the peritoneal area.
While until recently HGSC was thought to arise from simple differentiation of cortical inclusion cysts (CICs) of ovarian surface epithelium (OSE), the cell origin of HGSC is now understood to be much more complex, with evidence for other sites of origin, both intra- and extra-ovarian, having come to light.
| Tissue | Evidence for role as HGSC cell of origin |
|---|---|
| Ovary | Supporting:
Opposing:
|
| Coelomic epithelium | Supporting:
'Coelomic hypothesis' [25]
Opposing:
|
| Fallopian tube | Supporting:
Opposing:
|
| Extra-uterine Müllerian epithelium (EUME) | All epithelia of the female genital tract – Fallopian tubes, endometrium, endocervix, ectocervix, upper vagina - are derived from the embryonal Müllerian ducts. Extra-uterine Müllerian epithelium includes the distal end of the Fallopian tubes (the fimbriae), and instances of endosalpingiosis, endometriosis and endocervicosis.
Supporting:
Opposing:
|
| Border between ovary and Fallopian tube (transition zone) | Supporting:
Opposing:
|
The common Müllerian origin of the Fallopian tubes, uterus, cervix, and upper vagina has resulted in the proposal that peritoneal high-grade serous carcinoma is a spectrum of a single disease.[23]
Relevant animal models of HGSC can only be developed when the cell origin is properly understood. However, as HGSC tends to have the same clinical behaviour, regardless of its primary cell origin, determining cell origin is less important for clinical treatment, but may be of relevance when looking for biomarkers.
The specific process by which a HGSC arises may be related to the BRCA mutation status of the individual,[33][37] as well as the p53 mutation status.[21]
A 2007 paper describes the process of determining cell of origin as “Tumour origin is typically assigned to the organ presenting with the dominant tumour mass. The one exception is the peritoneum, which is classified as a primary site only if a candidate origin is not found in the endometrium, tube or ovary”.[38]
It is recognised that HGSC can have variable and complex primary origins, but understanding and determining this will give insight into its pathogenesis.
Pathogenesis
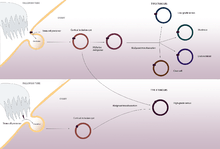
Assuming a fimbrial origin, as observed in the majority of HGSC cases,[29] the current understanding of HGSC genesis suggests a process by which STIC fimbrial cells implant into the ovary as cortical inclusion cysts through the ovulation rupture site.
To account for instances where there is no STIC involvement, endosalpingiosis or de novo metaplasia of ovarian surface epithelium inclusions are also possible. A much rarer occurrence is the differentiation of HGSC from LGSC.[5][6]
Diagnosis
Symptoms include persistent bloating, postmenopausal bleeding, and/or appetite loss.[39]
Transvaginal ultrasonography as well as cancer marker CA125 level analysis is often used to determine potential malignancy of suspect pelvic masses.[40]
Surgical staging is the procedure by which the abdominal cavity and lymph nodes are examined for malignant tissue, usually via laparoscopy. Tissue biopsies may be taken for further analysis. It is not until this histological analysis stage that actual diagnosis of HGSC can be made.[40]
If glands are seen to fuse with intricate, extensive papillae featuring epithelial tufting with solid nests surrounded by a space alongside irregular slit-like spaces, then serous carcinoma is suspected.
Distinguishing between LGSC and HGSC:[41]
- Necrosis is common in HGSC and absent in LGSC, as are giant (multi- or mononucleated) tumour cells.
- Psammoma bodies are more frequent in low-grade serous carcinoma.
- Tp53 expression is assessed for mutations, overexpression or absence – common features of high-grade serous carcinomas.
- LGSCs are generally limited to micropapillary growth patterns, whereas HGSCs can exhibit admixed patterns.
Distinction of HGSC from high-grade endometrioid carcinoma is not always possible.[41]
The progression of HGSC may also be determined from examining the cadherin expression profile.[42]
Screening
As ovarian cancer is rarely symptomatic until an advanced stage,[43] regular pre-emptive screening is a particularly important tool for avoiding the late stage at which most patients present. However, A 2011 US study found that transvaginal ultrasound and cancer marker CA125 screening did not reduce ovarian cancer mortality.[44] In contrast, a more recent UK study found that up to 20% of ovarian cancer deaths could be prevented through annual performance of these procedures.[45]
Prevention
Prevention for an individual deemed at risk of HGSC has, up until recently, been (bilateral or unilateral) removal of both the ovary and the Fallopian tube (salpingo-oophorectomy).
With hormonal and even morbidity issues resulting from ovary removal, and the increased evidence for the role of the Fallopian tubes HGSC pathogenesis, optimisation of this procedure has been to remove just the Fallopian tube(s) (salpingectomy) with the ovaries remaining until age of menopause [46][47] - although critics of this argue that a reduced blood supply to the ovaries may induce premature menopause regardless.[48]
Prophylactic salpingo-oophorectomy is frequently performed in carriers of BRCA1 or BRCA2 mutations,[49] although the benefits conferred by this procedure may vary dependent on the specific mutation.[50]
Tubal ligation is a less invasive prophylactic treatment shown to significantly reduce the risk of HGSC.[51]
Treatment
Cytoreductive “debulking” surgery may be performed prior to chemotherapy treatment in order to decrease the physical mass of the tumour and thus reduce the number of chemotherapy cycles needed.[40] The typical advanced presentation as well as extra-ovarian spread seen in HGSC can require aggressive debulking procedures.[52] In some cases total abdominal hysterectomy will be performed, in other cases where the patient intends to bear children a salpingo-oophorectomy is performed instead.
Typical chemotherapy is six cycles of intraperitoneally-delivered platinum-base adjuvant chemotherapy with agents such as carboplatin.[40] Measurements of blood CA125 levels are used to determine patient response to the treatment.
Between 20% and 30% of patients relapse within six months of treatment.[53]
Poly ADP ribose polymerase (PARP) inhibitors are another possible treatment, with carriers of BRCA1/2 mutations being the most responsive [54][55]
Epidemiology
A study of incidence rates in the US between 1992 and 1999 found that the age-specific incidence rate for HGSC doubles every 10 years up until age 55, where it plateaus at approximately 20 cases per 100,000 women - before dropping dramatically after age 75.[56]
Ovarian cancer incidence rates are low in East Asia[57] and highest in Europe, the United States, and Australia/New Zealand.[58]
Since 1975, survival rates for ovarian cancer have steadily improved with a mean decrease of 51% by 2006 of risk of death from ovarian cancer for an advanced stage tumour.[59] The increase has mainly been due to successful extended life expectancy of affected patients rather than an improvement in cure rates.
A racial disparity exists between black and white women in the US, where black women experience a higher mortality risk from ovarian cancer.[59][60]
References
- Shih, Ie-Ming; Kurman, Robert J. (2004-05-01). "Ovarian Tumorigenesis: A Proposed Model Based on Morphological and Molecular Genetic Analysis". The American Journal of Pathology. 164 (5): 1511–1518. doi:10.1016/S0002-9440(10)63708-X. PMC 1615664. PMID 15111296.
- Olivier, R. I.; van Beurden, M.; Lubsen, M. a. C.; Rookus, M. A.; Mooij, T. M.; van de Vijver, M. J.; van't Veer, L. J. (2004-03-16). "Clinical outcome of prophylactic oophorectomy in BRCA1/BRCA2 mutation carriers and events during follow-up". British Journal of Cancer. 90 (8): 1492–1497. doi:10.1038/sj.bjc.6601692. ISSN 0007-0920. PMC 2409718. PMID 15083174.
- Santillan, A.; Kim, Y.w.; Zahurak, M.l.; Gardner, G.j.; Giuntoli, R.l.; Shih, I.m.; Bristow, R.e. (2007-05-01). "Differences of chemoresistance assay between invasive micropapillary/low-grade serous ovarian carcinoma and high-grade serous ovarian carcinoma". International Journal of Gynecological Cancer. 17 (3): 601–606. doi:10.1111/j.1525-1438.2007.00820.x. ISSN 1525-1438. PMID 17504374.
- Schmeler, Kathleen M.; Sun, Charlotte C.; Bodurka, Diane C.; Deavers, Michael T.; Malpica, Anais; Coleman, Robert L.; Ramirez, Pedro T.; Gershenson, David M. (2008-03-01). "Neoadjuvant chemotherapy for low-grade serous carcinoma of the ovary or peritoneum". Gynecologic Oncology. 108 (3): 510–514. doi:10.1016/j.ygyno.2007.11.013. ISSN 1095-6859. PMID 18155273.
- Dehari, Reiko; Kurman, Robert J.; Logani, Sanjay; Shih, Ie-Ming (2007-07-01). "The development of high-grade serous carcinoma from atypical proliferative (borderline) serous tumors and low-grade micropapillary serous carcinoma: a morphologic and molecular genetic analysis". The American Journal of Surgical Pathology. 31 (7): 1007–1012. doi:10.1097/PAS.0b013e31802cbbe9. ISSN 0147-5185. PMID 17592266.
- Dehari, Reiko; Kurman, Robert J.; Logani, Sanjay; Shih, Ie-Ming (2007-07-01). "The development of high-grade serous carcinoma from atypical proliferative (borderline) serous tumors and low-grade micropapillary serous carcinoma: a morphologic and molecular genetic analysis". The American Journal of Surgical Pathology. 31 (7): 1007–1012. doi:10.1097/PAS.0b013e31802cbbe9. ISSN 0147-5185. PMID 17592266.
- Fathalla, M. F. (2013-01-01). "Incessant ovulation and ovarian cancer - a hypothesis re-visited". Facts, Views & Vision in ObGyn. 5 (4): 292–297. ISSN 2032-0418. PMC 3987381. PMID 24753957.
- Risch, H. A.; Marrett, L. D.; Howe, G. R. (1994-10-01). "Parity, contraception, infertility, and the risk of epithelial ovarian cancer". American Journal of Epidemiology. 140 (7): 585–597. doi:10.1093/oxfordjournals.aje.a117296. ISSN 0002-9262. PMID 7942759.
- Gwinn, M. L.; Lee, N. C.; Rhodes, P. H.; Layde, P. M.; Rubin, G. L. (1990-01-01). "Pregnancy, breast feeding, and oral contraceptives and the risk of epithelial ovarian cancer". Journal of Clinical Epidemiology. 43 (6): 559–568. doi:10.1016/0895-4356(90)90160-q. ISSN 0895-4356. PMID 2348208.
- Kurman, R. J. (2013-12-01). "Origin and molecular pathogenesis of ovarian high-grade serous carcinoma". Annals of Oncology. 24 Suppl 10: x16–21. doi:10.1093/annonc/mdt463. ISSN 1569-8041. PMID 24265397.
- DastranjTabrizi, Ali; MostafaGharabaghi, Parvin; SheikhzadehHesari, Farzam; Sadeghi, Liela; Zamanvandi, Sharareh; Sarbakhsh, Parvin; Ghojazadeh, Morteza (2016-01-01). "Impact and mechanistic role of oral contraceptive pills on the number and epithelial type of ovarian cortical inclusion cysts; a clinicopathology and immunohistochemical study". Diagnostic Pathology. 11: 30. doi:10.1186/s13000-016-0482-6. ISSN 1746-1596. PMC 4802821. PMID 27000861.
- Yang, Hannah P.; Anderson, William F.; Rosenberg, Philip S.; Trabert, Britton; Gierach, Gretchen L.; Wentzensen, Nicolas; Cronin, Kathleen A.; Sherman, Mark E. (2013-06-10). "Ovarian cancer incidence trends in relation to changing patterns of menopausal hormone therapy use in the United States". Journal of Clinical Oncology. 31 (17): 2146–2151. doi:10.1200/JCO.2012.45.5758. ISSN 1527-7755. PMC 3731982. PMID 23650423.
- Schildkraut, J. M.; Schwingl, P. J.; Bastos, E.; Evanoff, A.; Hughes, C. (1996-10-01). "Epithelial ovarian cancer risk among women with polycystic ovary syndrome". Obstetrics and Gynecology. 88 (4 Pt 1): 554–559. doi:10.1016/0029-7844(96)00226-8. ISSN 0029-7844. PMID 8841217.
- Pearce, Celeste Leigh; Templeman, Claire; Rossing, Mary Anne; Lee, Alice; Near, Aimee M.; Webb, Penelope M.; Nagle, Christina M.; Doherty, Jennifer A.; Cushing-Haugen, Kara L. (2012-04-01). "Association between endometriosis and risk of histological subtypes of ovarian cancer: a pooled analysis of case-control studies". The Lancet. Oncology. 13 (4): 385–394. doi:10.1016/S1470-2045(11)70404-1. ISSN 1474-5488. PMC 3664011. PMID 22361336.
- Toss, Angela; Tomasello, Chiara; Razzaboni, Elisabetta; Contu, Giannina; Grandi, Giovanni; Cagnacci, Angelo; Schilder, Russell J.; Cortesi, Laura (2015-01-01). "Hereditary ovarian cancer: not only BRCA 1 and 2 genes". BioMed Research International. 2015: 341723. doi:10.1155/2015/341723. ISSN 2314-6141. PMC 4449870. PMID 26075229.
- Liu, Guoyan; Yang, Da; Sun, Yan; Shmulevich, Ilya; Xue, Fengxia; Sood, Anil K.; Zhang, Wei (2012-10-01). "Differing clinical impact of BRCA1 and BRCA2 mutations in serous ovarian cancer". Pharmacogenomics. 13 (13): 1523–1535. doi:10.2217/pgs.12.137. ISSN 1744-8042. PMC 3603383. PMID 23057551.
- Liu, Ying; Yen, Hai-Yun; Austria, Theresa; Pettersson, Jonas; Peti-Peterdi, Janos; Maxson, Robert; Widschwendter, Martin; Dubeau, Louis (2015-10-01). "A Mouse Model That Reproduces the Developmental Pathways and Site Specificity of the Cancers Associated With the Human BRCA1 Mutation Carrier State". EBioMedicine. 2 (10): 1318–1330. doi:10.1016/j.ebiom.2015.08.034. ISSN 2352-3964. PMC 4634618. PMID 26629527.
- Cancer Genome Atlas Research Network (2011-06-30). "Integrated genomic analyses of ovarian carcinoma". Nature. 474 (7353): 609–615. doi:10.1038/nature10166. ISSN 1476-4687. PMC 3163504. PMID 21720365.
- Ahmed, Ahmed Ashour; Etemadmoghadam, Dariush; Temple, Jillian; Lynch, Andy G.; Riad, Mohamed; Sharma, Raghwa; Stewart, Colin; Fereday, Sian; Caldas, Carlos (2010-05-01). "Driver mutations in TP53 are ubiquitous in high grade serous carcinoma of the ovary". The Journal of Pathology. 221 (1): 49–56. doi:10.1002/path.2696. ISSN 1096-9896. PMC 3262968. PMID 20229506.
- Köbel, Martin; Reuss, Alexander; du Bois, Andreas; Kommoss, Stefan; Kommoss, Friedrich; Gao, Dongxia; Kalloger, Steve E.; Huntsman, David G.; Gilks, C. Blake (2010-10-01). "The biological and clinical value of p53 expression in pelvic high-grade serous carcinomas". The Journal of Pathology. 222 (2): 191–198. doi:10.1002/path.2744. ISSN 1096-9896. PMID 20629008.
- Kim, Jaeyeon; Coffey, Donna M.; Ma, Lang; Matzuk, Martin M. (2015-06-01). "The ovary is an alternative site of origin for high-grade serous ovarian cancer in mice". Endocrinology. 156 (6): 1975–1981. doi:10.1210/en.2014-1977. ISSN 1945-7170. PMC 5393339. PMID 25815421.
- Koshiyama, Masafumi; Matsumura, Noriomi; Konishi, Ikuo (2014-01-01). "Recent concepts of ovarian carcinogenesis: type I and type II". BioMed Research International. 2014: 934261. doi:10.1155/2014/934261. ISSN 2314-6141. PMC 4017729. PMID 24868556.
- Cobb, Lauren Patterson; Gaillard, Stephanie; Wang, Yihong; Shih, Ie-Ming; Secord, Angeles Alvarez (2015-01-01). "Adenocarcinoma of Mullerian origin: review of pathogenesis, molecular biology, and emerging treatment paradigms". Gynecologic Oncology Research and Practice. 2: 1. doi:10.1186/s40661-015-0008-z. ISSN 2053-6844. PMC 4880836. PMID 27231561.
- Flesken-Nikitin, Andrea; Hwang, Chang-Il; Cheng, Chieh-Yang; Michurina, Tatyana V.; Enikolopov, Grigori; Nikitin, Alexander Yu (2013-03-14). "Ovarian surface epithelium at the junction area contains a cancer-prone stem cell niche". Nature. 495 (7440): 241–245. Bibcode:2013Natur.495..241F. doi:10.1038/nature11979. ISSN 1476-4687. PMC 3982379. PMID 23467088.
- Dubeau, L.; Drapkin, R. (2013-11-01). "Coming into focus: the nonovarian origins of ovarian cancer". Annals of Oncology. 24 Suppl 8: viii28–viii35. doi:10.1093/annonc/mdt308. ISSN 1569-8041. PMC 3805308. PMID 24131966.
- Folkins, Ann K.; Jarboe, Elke A.; Saleemuddin, Aasia; Lee, Yonghee; Callahan, Michael J.; Drapkin, Ronny; Garber, Judy E.; Muto, Michael G.; Tworoger, Shelley (2008-05-01). "A candidate precursor to pelvic serous cancer (p53 signature) and its prevalence in ovaries and fallopian tubes from women with BRCA mutations". Gynecologic Oncology. 109 (2): 168–173. doi:10.1016/j.ygyno.2008.01.012. ISSN 1095-6859. PMC 2746001. PMID 18342932.
- Ng, Annie; Barker, Nick (2015-10-01). "Ovary and fimbrial stem cells: biology, niche and cancer origins". Nature Reviews Molecular Cell Biology. 16 (10): 625–638. doi:10.1038/nrm4056. ISSN 1471-0080. PMID 26350076.
- Kuhn, Elisabetta; Kurman, Robert J.; Vang, Russell; Sehdev, Ann Smith; Han, Guangming; Soslow, Robert; Wang, Tian-Li; Shih, Ie-Ming (2012-02-01). "TP53 mutations in serous tubal intraepithelial carcinoma and concurrent pelvic high-grade serous carcinoma--evidence supporting the clonal relationship of the two lesions". The Journal of Pathology. 226 (3): 421–426. doi:10.1002/path.3023. ISSN 1096-9896. PMC 4782784. PMID 21990067.
- Gilbert, Lucy; Basso, Olga; Sampalis, John; Karp, Igor; Martins, Claudia; Feng, Jing; Piedimonte, Sabrina; Quintal, Louise; Ramanakumar, Agnihotram V. (2012-03-01). "Assessment of symptomatic women for early diagnosis of ovarian cancer: results from the prospective DOvE pilot project". The Lancet. Oncology. 13 (3): 285–291. doi:10.1016/S1470-2045(11)70333-3. ISSN 1474-5488. PMID 22257524.
- Jazaeri, Amir A.; Bryant, Jennifer L.; Park, Hong; Li, Hui; Dahiya, Neetu; Stoler, Mark H.; Ferriss, James Stuart; Dutta, Anindya (2011-10-01). "Molecular requirements for transformation of fallopian tube epithelial cells into serous carcinoma". Neoplasia (New York, N.Y.). 13 (10): 899–911. doi:10.1593/neo.11138. ISSN 1476-5586. PMC 3201567. PMID 22028616.
- Saleemuddin, Aasia; Folkins, Ann K.; Garrett, Leslie; Garber, Judy; Muto, Michael G.; Crum, Christopher P.; Tworoger, Shelley (2008-11-01). "Risk factors for a serous cancer precursor ("p53 signature") in women with inherited BRCA mutations". Gynecologic Oncology. 111 (2): 226–232. doi:10.1016/j.ygyno.2008.07.018. ISSN 1095-6859. PMC 2613977. PMID 18718648.
- Levanon, K.; Ng, V.; Piao, H. Y.; Zhang, Yi; Chang, M. C.; Roh, M. H.; Kindelberger, D. W.; Hirsch, M. S.; Crum, C. P. (2010-02-25). "Primary ex vivo cultures of human fallopian tube epithelium as a model for serous ovarian carcinogenesis". Oncogene. 29 (8): 1103–1113. doi:10.1038/onc.2009.402. ISSN 1476-5594. PMC 2829112. PMID 19935705.
- Perets, Ruth; Wyant, Gregory A.; Muto, Katherine W.; Bijron, Jonathan G.; Poole, Barish B.; Chin, Kenneth T.; Chen, Jin Yun H.; Ohman, Anders W.; Stepule, Corey D. (2013-12-09). "Transformation of the fallopian tube secretory epithelium leads to high-grade serous ovarian cancer in Brca;Tp53;Pten models". Cancer Cell. 24 (6): 751–765. doi:10.1016/j.ccr.2013.10.013. ISSN 1878-3686. PMC 3917315. PMID 24332043.
- Dubeau, Louis (2015-02-01). "Pathogenesis of serous, extra-uterine Müllerian epithelial cancer and therapeutic implications". Translational Cancer Research. 4 (1): 3–13. doi:10.3978/j.issn.2218-676X.2015.01.06. ISSN 2218-676X. PMC 4643277. PMID 26568913.
- Esselen, Katharine; Terry, Kathryn (2016). "Endosalpingiosis: More than just an incidental finding at the time of gynecologic surgery?". Gynecologic Oncology. 142 (2): 255–260. doi:10.1016/j.ygyno.2016.05.036. PMID 27261327. Retrieved 24 June 2020.
- Mcnairn, AJ; Guasch, G (2011). "Epithelial transition zones: merging microenvironments, niches, and cellular transformation". European Journal of Dermatology. 21 (S1): 21–8. doi:10.1684/ejd.2011.1267. PMID 21628126.
- Howitt, Brooke E.; Hanamornroongruang, Suchanan; Lin, Douglas I.; Conner, James E.; Schulte, Stephanie; Horowitz, Neil; Crum, Christopher P.; Meserve, Emily E. (2015-03-01). "Evidence for a dualistic model of high-grade serous carcinoma: BRCA mutation status, histology, and tubal intraepithelial carcinoma". The American Journal of Surgical Pathology. 39 (3): 287–293. doi:10.1097/PAS.0000000000000369. ISSN 1532-0979. PMID 25581732.
- Crum, Christopher P.; Drapkin, Ronny; Miron, Alexander; Ince, Tan A.; Muto, Michael; Kindelberger, David W.; Lee, Yonghee (2007-02-01). "The distal fallopian tube: a new model for pelvic serous carcinogenesis". Current Opinion in Obstetrics and Gynecology. 19 (1): 3–9. doi:10.1097/GCO.0b013e328011a21f. ISSN 1040-872X. PMID 17218844.
- Bankhead, C. R.; Collins, C.; Stokes-Lampard, H.; Rose, P.; Wilson, S.; Clements, A.; Mant, D.; Kehoe, S. T.; Austoker, J. (2008-07-01). "Identifying symptoms of ovarian cancer: a qualitative and quantitative study". BJOG: An International Journal of Obstetrics and Gynaecology. 115 (8): 1008–1014. doi:10.1111/j.1471-0528.2008.01772.x. ISSN 1471-0528. PMC 2607526. PMID 18651882.
- Colombo, N.; Peiretti, M.; Parma, G.; Lapresa, M.; Mancari, R.; Carinelli, S.; Sessa, C.; Castiglione, M.; ESMO Guidelines Working Group (2010-05-01). "Newly diagnosed and relapsed epithelial ovarian carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up". Annals of Oncology. 21 Suppl 5: v23–30. doi:10.1093/annonc/mdq244. ISSN 1569-8041. PMID 20555088.
- Vang, Russell; Shih, Ie-Ming; Kurman, Robert J. (2009-09-01). "Ovarian low-grade and high-grade serous carcinoma: pathogenesis, clinicopathologic and molecular biologic features, and diagnostic problems". Advances in Anatomic Pathology. 16 (5): 267–282. doi:10.1097/PAP.0b013e3181b4fffa. ISSN 1533-4031. PMC 2745605. PMID 19700937.
- Quattrocchi, Livia; Green, Andrew R.; Martin, Stewart; Durrant, Lindy; Deen, Suha (2011-07-01). "The cadherin switch in ovarian high-grade serous carcinoma is associated with disease progression". Virchows Archiv. 459 (1): 21–29. doi:10.1007/s00428-011-1082-1. ISSN 1432-2307. PMID 21509572.
- Nagle, Christina M.; Francis, Jane E.; Nelson, Anne E.; Zorbas, Helen; Luxford, Karen; de Fazio, Anna; Fereday, Sian; Bowtell, David D.; Green, Adèle C. (2011-06-01). "Reducing time to diagnosis does not improve outcomes for women with symptomatic ovarian cancer: a report from the Australian Ovarian Cancer Study Group". Journal of Clinical Oncology. 29 (16): 2253–2258. doi:10.1200/JCO.2010.32.2164. ISSN 1527-7755. PMID 21537035.
- Buys, Saundra S.; Partridge, Edward; Black, Amanda; Johnson, Christine C.; Lamerato, Lois; Isaacs, Claudine; Reding, Douglas J.; Greenlee, Robert T.; Yokochi, Lance A. (2011-06-08). "Effect of screening on ovarian cancer mortality: the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Randomized Controlled Trial". JAMA. 305 (22): 2295–2303. doi:10.1001/jama.2011.766. ISSN 1538-3598. PMID 21642681.
- Jacobs, Ian J.; Menon, Usha; Ryan, Andy; Gentry-Maharaj, Aleksandra; Burnell, Matthew; Kalsi, Jatinderpal K.; Amso, Nazar N.; Apostolidou, Sophia; Benjamin, Elizabeth (2016-03-05). "Ovarian cancer screening and mortality in the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS): a randomised controlled trial". Lancet. 387 (10022): 945–956. doi:10.1016/S0140-6736(15)01224-6. ISSN 1474-547X. PMC 4779792. PMID 26707054.
- Oliver Perez, M. Reyes; Magriñá, Javier; García, Alvaro Tejerizo; Jiménez Lopez, Jesus Salvador (2015-12-01). "Prophylactic salpingectomy and prophylactic salpingoophorectomy for adnexal high-grade serous epithelial carcinoma: A reappraisal". Surgical Oncology. 24 (4): 335–344. doi:10.1016/j.suronc.2015.09.008. ISSN 1879-3320. PMID 26690823.
- Daly, Mary B.; Dresher, Charles W.; Yates, Melinda S.; Jeter, Joanne M.; Karlan, Beth Y.; Alberts, David S.; Lu, Karen H. (2015-05-01). "Salpingectomy as a means to reduce ovarian cancer risk". Cancer Prevention Research (Philadelphia, Pa.). 8 (5): 342–348. doi:10.1158/1940-6207.CAPR-14-0293. ISSN 1940-6215. PMC 4417454. PMID 25586903.
- Pölcher, Martin; Hauptmann, Steffen; Fotopoulou, Christina; Schmalfeldt, Barbara; Meinhold-Heerlein, Ivo; Mustea, Alexander; Runnebaum, Ingo; Sehouli, Jalid (2015-07-01). "Opportunistic salpingectomies for the prevention of a high-grade serous carcinoma: a statement by the Kommission Ovar of the AGO". Archives of Gynecology and Obstetrics. 292 (1): 231–234. doi:10.1007/s00404-015-3697-y. ISSN 1432-0711. PMID 25914073.
- Kauff, Noah D.; Satagopan, Jaya M.; Robson, Mark E.; Scheuer, Lauren; Hensley, Martee; Hudis, Clifford A.; Ellis, Nathan A.; Boyd, Jeff; Borgen, Patrick I. (2002-05-23). "Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation". The New England Journal of Medicine. 346 (21): 1609–1615. doi:10.1056/NEJMoa020119. ISSN 1533-4406. PMID 12023992.
- Kauff, Noah D.; Domchek, Susan M.; Friebel, Tara M.; Robson, Mark E.; Lee, Johanna; Garber, Judy E.; Isaacs, Claudine; Evans, D. Gareth; Lynch, Henry (2008-03-10). "Risk-reducing salpingo-oophorectomy for the prevention of BRCA1- and BRCA2-associated breast and gynecologic cancer: a multicenter, prospective study". Journal of Clinical Oncology. 26 (8): 1331–1337. doi:10.1200/JCO.2007.13.9626. ISSN 1527-7755. PMC 3306809. PMID 18268356.
- Sieh, Weiva; Salvador, Shannon; McGuire, Valerie; Weber, Rachel Palmieri; Terry, Kathryn L.; Rossing, Mary Anne; Risch, Harvey; Wu, Anna H.; Webb, Penelope M. (2013-04-01). "Tubal ligation and risk of ovarian cancer subtypes: a pooled analysis of case-control studies". International Journal of Epidemiology. 42 (2): 579–589. doi:10.1093/ije/dyt042. ISSN 1464-3685. PMC 3619957. PMID 23569193.
- Ferguson, Donna; Han, Lucy (2015). "The role of the fallopian tube in ovarian serous carcinogenesis: biologic mechanisms and clinical impacts" (PDF). American Journal of Clinical and Experimental Obstetrics and Gynecology. 2 (1).
- Berns, Els M. J. J.; Bowtell, David D. (2012-06-01). "The changing view of high-grade serous ovarian cancer". Cancer Research. 72 (11): 2701–2704. doi:10.1158/0008-5472.CAN-11-3911. ISSN 1538-7445. PMID 22593197.
- Ivy, S. Percy; Liu, Joyce F.; Lee, Jung-Min; Matulonis, Ursula A.; Kohn, Elise C. (2016-05-01). "Cediranib, a pan-VEGFR inhibitor, and olaparib, a PARP inhibitor, in combination therapy for high grade serous ovarian cancer". Expert Opinion on Investigational Drugs. 25 (5): 597–611. doi:10.1517/13543784.2016.1156857. ISSN 1744-7658. PMID 26899229.
- Parkes, Eileen E.; Kennedy, Richard D. (2016-05-01). "Clinical Application of Poly(ADP-Ribose) Polymerase Inhibitors in High-Grade Serous Ovarian Cancer". The Oncologist. 21 (5): 586–593. doi:10.1634/theoncologist.2015-0438. ISSN 1549-490X. PMC 4861365. PMID 27022037.
- Quirk, Jeffrey T.; Natarajan, Nachimuthu; Mettlin, Curtis J. (2005-10-01). "Age-specific ovarian cancer incidence rate patterns in the United States". Gynecologic Oncology. 99 (1): 248–250. doi:10.1016/j.ygyno.2005.06.052. ISSN 0090-8258. PMID 16095676.
- Liede, Alexander; Narod, Steven A. (2002-12-01). "Hereditary breast and ovarian cancer in Asia: genetic epidemiology of BRCA1 and BRCA2". Human Mutation. 20 (6): 413–424. doi:10.1002/humu.10154. ISSN 1098-1004. PMID 12442265.
- Ferlay, Jacques; Shin, Hai-Rim; Bray, Freddie; Forman, David; Mathers, Colin; Parkin, Donald Maxwell (2010-12-15). "Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008". International Journal of Cancer. 127 (12): 2893–2917. doi:10.1002/ijc.25516. ISSN 1097-0215. PMID 21351269.
- Temkin, Sarah M.; Terplan, Mishka (2015-10-01). "Trends in Relative Survival for Ovarian Cancer From 1975-2011". Obstetrics and Gynecology. 126 (4): 898. doi:10.1097/AOG.0000000000001073. ISSN 1873-233X. PMID 26393445.
- Terplan, Mishka; Schluterman, Nicholas; McNamara, Erica J.; Tracy, J. Kathleen; Temkin, Sarah M. (2012-04-01). "Have racial disparities in ovarian cancer increased over time? An analysis of SEER data". Gynecologic Oncology. 125 (1): 19–24. doi:10.1016/j.ygyno.2011.11.025. ISSN 1095-6859. PMID 22108636.