MRI contrast agent
MRI contrast agents are contrast agents used to improve the visibility of internal body structures in magnetic resonance imaging (MRI).[1] The most commonly used compounds for contrast enhancement are gadolinium-based. Such MRI contrast agents shorten the relaxation times of nuclei within body tissues following oral or intravenous administration.
In MRI scanners, sections of the body are exposed to a very strong magnetic field causing primarily the hydrogen nuclei ("spins") of water in tissues to be polarized in the direction of the magnetic field. An intense radiofrequency pulse is applied that tips the magnetization generated by the hydrogen nuclei in the direction of the receiver coil where the spin polarization can be detected. Random molecular rotational oscillations matching the resonance frequency of the nuclear spins provide the "relaxation" mechanisms that bring the net magnetization back to its equilibrium position in alignment with the applied magnetic field. The magnitude of the spin polarization detected by the receiver is used to form the MR image but decays with a characteristic time constant known as the T1 relaxation time. Water protons in different tissues have different T1 values, which is one of the main sources of contrast in MR images. A contrast agent usually shortens, but in some instances increases, the value of T1 of nearby water protons thereby altering the contrast in the image.
Types
Most clinically used MRI contrast agents work by shortening the T1 relaxation time of protons inside tissues via interactions with the nearby contrast agent. Thermally driven motion of the strongly paramagnetic metal ions in the contrast agent generate the oscillating magnetic fields that provide the relaxation mechanisms that enhance the rate of decay of the induced polarization. The systematic sampling of this polarization over the spatial region of the tissue being examined forms the basis for construction of the image.
MRI contrast agents may be administered by injection into the blood stream or orally, depending on the subject of interest. Oral administration is well suited to G.I. tract scans, while intravascular administration proves more useful for most other scans. A variety of agents of both types enhances scans routinely.
MRI contrast agents can be classified in many ways,[2] including by their:
- chemical composition
- administration route
- magnetic properties
- effect on the image
- presence and nature of metal atoms
- biodistribution and applications:
- Extracellular fluid agents (also known as intravenous contrast agents)
- Blood pool agents (also known as intravascular contrast agents)
- Organ specific agents (i.e. gastrointestinal contrast agents and hepatobiliary contrast agents)
- Active targeting/cell labeling agents (i.e. tumor-specific agents)
- Responsive (also known as smart or bioactivated) agents
- pH-sensitive agents
Gadolinium (Gd): paramagnetic
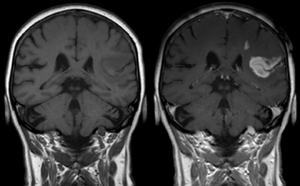
Gadolinium(III) containing MRI contrast agents (often termed simply "gado" or "gad") are the most commonly used for enhancement of vessels in MR angiography or for brain tumor enhancement associated with the degradation of the blood–brain barrier. For large vessels such as the aorta and its branches, the gadolinium(III) dose can be as low as 0.1 mmol per kg body mass. Higher concentrations are often used for finer vasculature.[3] Gd(III) chelates do not pass the intact blood–brain barrier because they are hydrophilic. Thus, these are useful in enhancing lesions and tumors where blood-brain barrier is compromised and the Gd(III) leaks out. In the rest of the body, the Gd(III) initially remains in the circulation but then distributes into the interstitial space or is eliminated by the kidneys.
Types by body compartment
Gadolinium(III) contrast agents can be categorized into:
Extracellular fluid agents
- gadoterate (Dotarem, Clariscan)
- gadodiamide (Omniscan)
- gadobenate (MultiHance)
- gadopentetate (Magnevist)
- gadoteridol (ProHance)
- gadoversetamide (OptiMARK)
- gadobutrol (Gadovist [EU] / Gadavist [US])
- gadopentetic acid dimeglumine (Magnetol)
Blood pool agents
- Albumin-binding gadolinium complexes
- gadofosveset (Ablavar, formerly Vasovist)
- gadocoletic acid
- Polymeric gadolinium complexes
- gadomelitol
- gadomer 17
Hepatobiliary (liver) agents
- gadoxetic acid (Primovist [EU] / Eovist [US]) is used as a hepatobiliary agent as 50% is taken up and excreted by the liver and 50% by the kidneys.
Agents approved for human use
The following gadolinium chelated contrast agents have been approved for human use by European Medicines Agency (EMA)[4] and/or the U.S. Food and Drug Administration (FDA):[5]
- EMA FDA gadoterate (Dotarem; European: Clariscan)
- EMA FDA gadodiamide (Omniscan)
- EMA FDA gadobenate (MultiHance)
- EMA FDA gadopentetate (Magnevist; European: Magnegita, Gado-MRT ratiopharm)
- EMA FDA gadoteridol (ProHance)
- FDA gadofosveset (Ablavar, formerly Vasovist)
- EMA FDA gadoversetamide (OptiMARK)
- EMA FDA gadoxetate (Eovist; European: Primovist)
- EMA FDA gadobutrol (Gadovist)
Safety of gadolinium contrast agents
Anaphylactoid reactions are rare, occurring in about 0.03–0.1%.[6]
As a free solubilized aqueous ion, gadolinium (III) is somewhat toxic, but was generally regarded as safe when administered as a chelated compound. In animals the free Gd (III) ion exhibits a 100–200 mg/kg 50% lethal dose, but the LD50 is increased by a factor of 100 when Gd (III) is chelated, so that its toxicity becomes comparable to iodinated X-ray contrast compounds.[7] The chelating carrier molecule for Gd for MRI contrast use may be classified by whether they are macro-cyclic or have linear geometry and whether they are ionic or not. Cyclical ionic Gd(III) compounds are considered the least likely to release the Gd(III) ion, and hence the safest.[8]
However, the use of some Gd(III) chelates in persons with kidney disease was linked to a rare but severe complication, nephrogenic fibrosing dermopathy,[9] also known as nephrogenic systemic fibrosis (NSF).[9][10][11] This systemic disease resembles scleromyxedema and to some extent scleroderma. It may occur months after contrast has been injected.[12] Patients with poorer kidney function are more at risk for NSF, with dialysis patients being more at risk than patients with chronic kidney disease.[13][14] At present, NSF has been linked to the use of four gadolinium-containing MRI contrast agents. The World Health Organization issued a restriction on use of several gadolinium contrast agents in November 2009 stating that "High-risk gadolinium-containing contrast agents (Optimark, Omniscan, Magnevist, Magnegita, and Gado-MRT ratiopharm) are contraindicated in patients with severe kidney problems, in patients who are scheduled for or have recently received a liver transplant, and in newborn babies up to four weeks of age."[15]
Gadolinium has been found to remain in the body after multiple MRIs, even after a prolonged period of time. Although gadolinium contrast agents have not been found to be harmful to the body, it is unknown whether these deposits can lead to adverse health effects. The FDA has asked doctors to limit the use of Gadolinium contrast agents to times when necessary information is made available through its use.[16]
Continuing evidence of the retention of gadolinium in brain and other tissues following exposure to gadolinium containing contrast media, has led to a safety review by the European Medicines Agency (EMA and The Committee for Medicinal Products for Human Use (CHMP)). Although not directly linked to adverse health effects in patients with normal kidney function, the possible risk of using intravenous linear chelated media, in which the gadolinium is shown to have a lower binding affinity, has led to a change in the market authorisation for all linear chelated gadolinium-based media.
In the United States, the research has led the FDA (Food and Drug Administration) to revise its class warnings for all gadolinium-based contrast media. It is advised that the use of gadolinium-based media is based on careful consideration of the retention characteristics of the preferred medium. Extra care being taken in patients requiring multiple lifetime doses, pregnant, and paediatric patients, and patients with inflammatory conditions. Minimizing repeated GBCA imaging studies when possible, particularly closely spaced MRI studies. However, do not avoid or defer necessary GBCA MRI scans.[17]
In magnetic resonance imaging in pregnancy, gadolinium contrast agents in the first trimester is associated with a slightly increased risk of a childhood diagnosis of several forms of rheumatism, inflammatory disorders, or infiltrative skin conditions, according to a retrospective study including 397 infants prenatally exposed to gadolinium contrast.[18] In the second and third trimester, gadolinium contrast is associated with a slightly increased risk of stillbirth or neonatal death, by the same study.[18]
In December 2017, the FDA announced in a drug safety communication it is requiring these new warnings to be included on all GBCAs. The FDA also called for increased patient education and requiring gadolinium contrast vendors to conduct additional animal and clinical studies to assess the safety of these agents.[19]
Iron oxide: superparamagnetic
Two types of iron oxide contrast agents exist: superparamagnetic iron oxide (SPIO) and ultrasmall superparamagnetic iron oxide (USPIO). These contrast agents consist of suspended colloids of iron oxide nanoparticles and when injected during imaging reduce the T2 signals of absorbing tissues. SPIO and USPIO contrast agents have been used successfully in some instances for liver tumor enhancement.[20]
- Feridex I.V. (also known as Endorem and ferumoxides). This product was discontinued by AMAG Pharma in November 2008.[21]
- Resovist (also known as Cliavist). This was approved for the European market in 2001, but production was abandoned in 2009.[22]
- Sinerem (also known as Combidex). Guerbet withdrew the marketing authorization application for this product in 2007.[23]
- Lumirem (also known as Gastromark). Gastromark was approved by the FDA in 1996[24] and was discontinued by its manufacturer in 2012.[25][26]
- Clariscan (also known as PEG-fero, Feruglose, and NC100150). This iron based contrast agent was never commercially launched and its development was discontinued in early 2000s due to safety concerns.[27] In 2017 GE Healthcare launched a macrocyclic extracellular gadolinium based contrast agent containing gadoteric acid as gadoterate meglumine under the trade name Clariscan.[28]
Iron platinum: superparamagnetic
Superparamagnetic iron–platinum particles (SIPPs) have been reported and had significantly better T2 relaxivities compared with the more common iron oxide nanoparticles. SIPPs were also encapsulated with phospholipids to create multifunctional SIPP stealth immunomicelles that specifically targeted human prostate cancer cells.[29] These are, however, investigational agents which have not yet been tried in humans. In a recent study, multifunctional SIPP micelles were synthesized and conjugated to a monoclonal antibody against prostate-specific membrane antigen.[29] The complex specifically targeted human prostate cancer cells in vitro, and these results suggest that SIPPs may have a role in the future as tumor-specific contrast agents.
Manganese: paramagnetic
Unlike the other well-studied iron oxide-based nanoparticles, research on Mn-based nanoparticles is at a relatively early stage.[30] Manganese chelates such as Mn-DPDP enhance the T1 signal and have been used for the detection of liver lesions. The chelate dissociates in vivo into manganese and DPDP where the former is absorbed intra-cellularly and excreted in bile, while the latter is eliminated via the kidney filtration.[31]
Manganese ions (Mn2+) are often used as a contrast agent in animal studies, usually referred to as MEMRI (Manganese Enhanced MRI).[32] Due to the ability of Mn2+ to enter cells through Calcium Ca2+ channels Mn2+ can e.g. be used for functional brain imaging.[33]
Oral administration of contrast agents
A wide variety of oral contrast agents can enhance images of the gastrointestinal tract. They include gadolinium and manganese chelates, or iron salts for T1 signal enhancement. SPIO, barium sulfate, air and clay have been used to lower T2 signal. Natural products with high manganese concentration such as blueberry and green tea can also be used for T1 increasing contrast enhancement.[34]
Perflubron, a type of perfluorocarbon, has been used as a gastrointestinal MRI contrast agent for pediatric imaging.[35] This contrast agent works by reducing the number of hydrogen ions in a body cavity, thus causing it to appear dark in the images.
Protein-based MRI contrast agents
Newer research suggests the possibility of protein based contrast agents, based on the abilities of some amino acids to bind with gadolinium.[36][37][38][39]
See also
References
| Wikimedia Commons has media related to Contrast agents used in magnetic resonance imaging. |
- Rinck, Peter A. (2017). "Chapter 13 – Contrast Agents". Magnetic Resonance in Medicine (11th ed.). European Magnetic Resonance Forum. Retrieved 2020-07-31.
- Geraldes, Carlos F.G.C.; Laurent, Sophie (2009). "Classification and basic properties of contrast agents for magnetic resonance imaging". Contrast Media & Molecular Imaging. 4 (1): 1–23. doi:10.1002/cmmi.265. PMID 19156706.
- Lentschig, M.G.; Reimer, P.; Rausch-Lentschig, U.L.; Allkemper, T.; Oelerich, M.; Laub, G. (1998). "Breath-hold gadolinium-enhanced MR angiography of the major vessels at 1.0 T: Dose-response findings and angiographic correlation". Radiology. 208 (2): 353–57. doi:10.1148/radiology.208.2.9680558. PMID 9680558.
- "EMA recommendations on Gadolinium-containing contrast agents". ema.europa.eu. Retrieved 2018-07-12.
- "Information on Gadolinium-Containing Contrast Agents". Fda.gov. Retrieved 2018-07-12.
- Murphy KJ, Brunberg JA, Cohan RH; Brunberg; Cohan (1 October 1996). "Adverse reactions to gadolinium contrast media: A 1996 review of 36 cases". AJR Am J Roentgenol. 167 (4): 847–49. doi:10.2214/ajr.167.4.8819369. PMID 8819369.CS1 maint: multiple names: authors list (link)
- Penfield, Jeffrey G.; Reilly, Robert F. (2007). "What nephrologists need to know about gadolinium". Nature Clinical Practice Nephrology. 3 (12): 654–68. doi:10.1038/ncpneph0660. PMID 18033225.
- "Questions and Answers" (PDF). International Society for Magnetic Resonance in Medicine.
- Grobner, T. (2005). "Gadolinium – a specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis?". Nephrology Dialysis Transplantation. 21 (4): 1104–08. doi:10.1093/ndt/gfk062. PMID 16431890.
- Marckmann, P.; Skov, L.; Rossen, K.; Dupont, A.; Damholt, M.B.; Heaf, J.G.; Thomsen, H.S. (2006). "Nephrogenic Systemic Fibrosis: Suspected Causative Role of Gadodiamide Used for Contrast-Enhanced Magnetic Resonance Imaging". Journal of the American Society of Nephrology. 17 (9): 2359–62. doi:10.1681/ASN.2006060601. PMID 16885403.
- Centers for Disease Control and Prevention (CDC) (2007). "Nephrogenic fibrosing dermopathy associated with exposure to gadolinium-containing contrast agents". MMWR. Morbidity and Mortality Weekly Report. 56 (7): 137–41. PMID 17318112.
- Thomsen, H.S.; Morcos, S.K.; Dawson, P. (2006). "Is there a causal relation between the administration of gadolinium based contrast media and the development of nephrogenic systemic fibrosis (NSF)?". Clinical Radiology. 61 (11): 905–06. doi:10.1016/j.crad.2006.09.003. PMID 17018301.
- Kanal, E.; Barkovich, A.J.; Bell, C.; Borgstede, J.P.; Bradley, W.G.; Froelich, J.W.; Gilk, T.; Gimbel, J.R.; et al. (2007). "ACR Guidance Document for Safe MR Practices: 2007". American Journal of Roentgenology. 188 (6): 1447–74. doi:10.2214/AJR.06.1616. PMID 17515363.
- "Gadolinium and NSF What is fact and what is theory?". 2008.
- "Pharmaceuticals: Restrictions in Use and Availability" (PDF). World Health Organization. 2010. p. 14.
- https://www.fda.gov/Drugs/DrugSafety/ucm455386.htm
- "FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body; requires new class warnings" (PDF). United States Food and Drug Administration. 2017-12-19.

- Mervak, Benjamin M.; Altun, Ersan; McGinty, Katrina A.; Hyslop, W. Brian; Semelka, Richard C.; Burke, Lauren M. (2019). "MRI in pregnancy: Indications and practical considerations". Journal of Magnetic Resonance Imaging. 49 (3): 621–31. doi:10.1002/jmri.26317. ISSN 1053-1807. PMID 30701610.
- "fda-drug-safety-communication-fda-warns-gadolinium-based-contrast-agents-gbcas-are-retained-body; requires new class warnings". USA FDA. 2018-05-16.
- Nakamura, Hiroshi; Ito, Naoki; Kotake, Fumio; Mizokami, Yuji; Matsuoka, Takeshi (2000). "Tumor-detecting capacity and clinical usefulness of SPIO-MRI in patients with hepatocellular carcinoma". Journal of Gastroenterology. 35 (11): 849–55. doi:10.1007/s005350070022. PMID 11085494.
- "Feridex". Amagpharma.com. Archived from the original on 2012-06-15. Retrieved 2012-06-20.
- Softways. "Magnetic Resonance TIP – MRI Database : Resovist". Mr-tip.com. Retrieved 2012-06-20.
- "Update on Sinerem (TM) in Europe". AMAG Pharmaceuticals. 2007-12-13. Retrieved 2012-06-20 – via Thefreelibrary.com.
- "Newly Approved Drug Therapies (105) GastroMARK, Advanced Magnetics". CenterWatch. Archived from the original on 2011-12-29. Retrieved 2012-06-20.
- "AMAG Form 10-K For the Fiscal Year Ended December 31, 2013". SEC Edgar.
- "NDA 020410 for GastroMark". FDA. Retrieved 12 February 2017.
- Wang, Yi-Xiang J. (2011). "Superparamagnetic iron oxide based MRI contrast agents: Current status of clinical application". Quantitative Imaging in Medicine and Surgery. 1 (1): 35–40. doi:10.3978/j.issn.2223-4292.2011.08.03. PMC 3496483. PMID 23256052.
- "Archived copy" (PDF). Archived from the original (PDF) on 2017-03-01. Retrieved 2017-02-28.CS1 maint: archived copy as title (link)
- Taylor, Robert M.; Huber, Dale L.; Monson, Todd C.; Ali, Abdul-Mehdi S.; Bisoffi, Marco; Sillerud, Laurel O. (2011). "Multifunctional iron platinum stealth immunomicelles: Targeted detection of human prostate cancer cells using both fluorescence and magnetic resonance imaging". Journal of Nanoparticle Research. 13 (10): 4717–29. doi:10.1007/s11051-011-0439-3. PMC 3223933. PMID 22121333.
- Zhen, Zipeng; Xie, J (2012). "Development of Manganese-Based Nanoparticles as Contrast Probes for Magnetic Resonance Imaging". Theranostics. 2 (1): 45–54. doi:10.7150/thno.3448. PMC 3263515. PMID 22272218.
- Harisinghani, Mukesh G.; Jhaveri, Kartik S.; Weissleder, Ralph; Schima, Wolfgang; Saini, Sanjay; Hahn, Peter F.; Mueller, Peter R. (2001). "MRI Contrast Agents for Evaluating Focal Hepatic Lesions". Clinical Radiology. 56 (9): 714–25. doi:10.1053/crad.2001.0764. PMID 11585393.
- Koretsky, Alan P.; Silva, Afonso C. (2004). "Manganese-enhanced magnetic resonance imaging (MEMRI)". NMR in Biomedicine. 17 (8): 527–31. doi:10.1002/nbm.940. PMID 15617051.
- Lin, Yi-Jen; Koretsky, Alan P. (1997). "Manganese ion enhances T1-weighted MRI during brain activation: An approach to direct imaging of brain function". Magnetic Resonance in Medicine. 38 (3): 378–88. doi:10.1002/mrm.1910380305. PMID 9339438.
- Lee, Joseph K.T. (2006). Computed Body Tomography with MRI Correlation. ISBN 978-0-7817-4526-0.
- Bisset, G.S.; Emery, K.H.; Meza, M.P.; Rollins, N.K.; Don, S.; Shorr, J.S. (1996). "Perflubron as a gastrointestinal MR imaging contrast agent in the pediatric population". Pediatric Radiology. 26 (6): 409–15. doi:10.1007/BF01387316. PMID 8657479.
- Xue, Shenghui; Qiao, Jingjuan; Pu, Fan; Cameron, Mathew; Yang, Jenny J. (2013). "Design of a novel class of protein-based magnetic resonance imaging contrast agents for the molecular imaging of cancer biomarkers". Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology. 5 (2): 163–79. doi:10.1002/wnan.1205. PMC 4011496. PMID 23335551.
- Li, Shunyi; Jiang, Jie; Zou, Jin; Qiao, Jingjuan; Xue, Shenghui; Wei, Lixia; Long, Robert; Wang, Liya; et al. (2012). "PEGylation of protein-based MRI contrast agents improves relaxivities and biocompatibilities". Journal of Inorganic Biochemistry. 107 (1): 111–18. doi:10.1016/j.jinorgbio.2011.11.004. PMC 3273044. PMID 22178673.
- Xue, Shenghui; Qiao, Jingjuan; Hubbard, Kendra; White, Natalie; Wei, Lixia; Li, Shunyi; Liu, Zhi-Reb; Yang, Jenny J; Yang, J.J. (2014). "Design of ProCAs (Protein-Based Gd3+ MRI Contrast Agents) with High Dose Efficiency and Capability for Molecular Imaging of Cancer Biomarkers". Medicinal Research Reviews. 34 (5): 1070–99. doi:10.1002/med.21313. PMID 24615853.
- Qiao, Jingjuan; Xue, Shenghui; Pu, Fan; White, Natalie; Liu, Zhi-Ren; Yang, Jenny J. (2014). "Molecular imaging of EGFR/HER2 cancer biomarkers by protein MRI contrast agents". J Biol Inorg Chem. 19 (2): 259–70. doi:10.1007/s00775-013-1076-3. PMC 3931309. PMID 24366655.