Diverticulum
In medicine or biology, a diverticulum is an outpouching of a hollow (or a fluid-filled) structure in the body.[1] Depending upon which layers of the structure are involved, diverticula are described as being either true or false.[2]
| Diverticulum | |
|---|---|
| Other names | Diverticula |
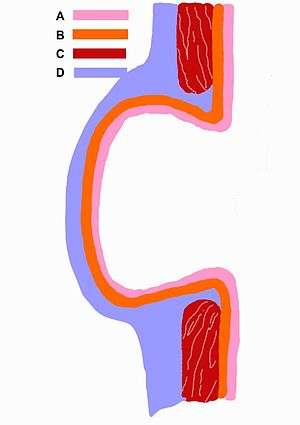 | |
| Schematic drawing of a false diverticulum. A - mucosa; B - submucosa; C - muscularis; D - serosa and subserosa | |
| Specialty | Gastroenterology |
In medicine, the term usually implies the structure is not normally present. However, in embryology the term is used for some normal structures arising from others, as for instance the thyroid diverticulum, which arises from the tongue.[3]
The word comes from Latin dīverticulum, "bypath" or "byway."
Classification
Diverticula are described as being true or false depending upon the layers involved:
- True diverticula involve all layers of the structure, including muscularis propria and adventitia, such as Meckel's diverticulum.[2]
- False diverticula (also known as "pseudodiverticula") do not involve muscular layers or adventitia. False diverticula, in the gastrointestinal tract for instance, involve only the submucosa and mucosa.[2]
Embryological
- The kidneys, originally diverticula in the development of the urinary and reproductive organs.
- The lungs, originally diverticula forming off of the ventral foregut.[3]
- The thymus appears in the form of two flask-shape diverticula, which arise from the third branchial pouch (pharyngeal pouch) of the endoderm.[4]
- The thyroid gland develops as a diverticulum arising from a point on the tongue, demarcated as the foramen cecum.[3]
Human pathology
Gastrointestinal tract diverticula
- Meckel's diverticulum: a persistent portion of the omphalomesenteric duct present in 2% of the population,[5] making it the most common congenital gastrointestinal malformation.[6]
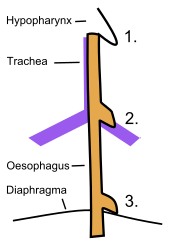
- Esophageal diverticula may occur in one of three areas of the esophagus:
- Killian-Jamieson diverticulum- is very similar to a pharyngeal esophageal diverticulum, differing in the fact that the pouching is below the cricopharyngeal muscle.[8]
- Colonic diverticula: Although found incidentally during colonoscopy, these diverticula may become infected (see diverticulitis) and can perforate, requiring surgery.[9]
- Duodenal divertiula: Such condition can be found incidentally in 23% of the normal people underwent imaging. It can be either congenital or acquired but the acquired form is more common. It is due to the weakness of the duodenal wall which causes protusions. It is usually found at the 2nd or 3rd part of duodenum, around the Ampulla of Vater. Food debris may enter the diverticula outpouchings, causing inflammation or diverticulitis. On CT or MRI imaging, they appear as sac-like outpouchings. If the diverticula are filled with contrast agents, the wall would be thin, which may contain air, fluid, contrast material or food debris. If the food debris is broken down by bacteria, the outpouchings may show "faeces sign". Inflammation of the duodenal wall will show thickening of the wall. Rarely, on barium studies in congenital duodenal diverticula, the contrast material fill-up the true lumen, causing "windsock deformity.[10]
- Jejunal diverticul(um|a): are congenital lesions and may be a source of bacterial overgrowth. They may also perforate or result in abscesses.
- Rokitansky-Aschoff sinuses are diverticula in the gallbladder due to chronic cholecystitis[11]
- Gastric diverticula are very infrequent.[12]
Most of these pathological types of diverticulum are capable of harboring an enterolith. If the enterolith stays in place, it may cause no problems, but a large enterolith expelled from a diverticulum into the lumen can cause obstruction.
Genito-urinary tract diverticula
- Calyceal diverticulum: usually asymptomatic, but if a stone becomes lodged in the outpouching they may present with pain.[13]
- Bladder diverticulum: Balloon-like growths on the bladder commonly associated with a chronic outflow obstruction, such as benign prostatic hyperplasia in older males. Usually found in pairs on opposite sides of the bladder, bladder diverticula are often surgically removed to prevent infection, rupture, or even cancer.
- Urethral diverticulum: Urethral diverticula are usually found in women aged 30 to 70 years old, between 1% to 6% of adult women. Since majority of cases are without any symptoms, the true incidence is unknown. Symptoms may vary from frequent urinary tract infections, painful sexual intercourse (dyspareunia), or symptoms due to cancer. Urethral diverticulum is located on the anterior vaginal wall, 1 to 3 cm inside the vaginal introitus. MRI is preferred as the imaging of choice due to its excellent soft-tissue resolution. On T2 weighted imaging, it will show high signal in the diverticulum due to the presence of fluid inside it. Vaginal ultrasonography is highly sensitive in diagnosing the diverticulum but it is strongly dependent on the skills of the operator.[14]
Other diverticula
- Cardiac diverticulum: A very rare congenital malformation of the heart that is usually benign [15]
- Diverticulum of Kommerell: is an out-pouching(aneurysm) of the aorta where an aberrant right subclavian artery is located.[16] It is unusual nomenclature, in that focal dilatations of a blood vessel are properly referred to as aneurysms.
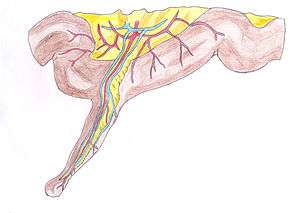 Meckel's diverticulum
Meckel's diverticulum Large bowel (sigmoid colon) showing multiple diverticula. Note how the diverticula appear on either side of the longitudinal muscle bundle (taenium).
Large bowel (sigmoid colon) showing multiple diverticula. Note how the diverticula appear on either side of the longitudinal muscle bundle (taenium). Colonic diverticulum
Colonic diverticulum Diverticulum of urinary bladder of a 59-year-old man, transverse plane
Diverticulum of urinary bladder of a 59-year-old man, transverse plane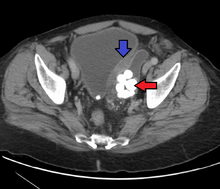 Bladder diverticula containing stones. Also note that the bladder wall is thickened due to possible transitional cell carcinoma.
Bladder diverticula containing stones. Also note that the bladder wall is thickened due to possible transitional cell carcinoma.
See also
Footnotes
- "diverticulum | Definition of diverticulum in English by Lexico Dictionaries". Lexico Dictionaries | English. Retrieved 2019-07-17.
- Townsend, Jr., Courtney M.; Daniel Beauchamp, R.; Mark Evers, B.; Mattox, Kenneth L. (2017). Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice (20th ed.). Philadelphia, PA. ISBN 9780323299879. OCLC 921338900.
- Sadler, Thomas W. (2012). Langman's Medical Embryology (12th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. ISBN 9781451113426. OCLC 732776409.
- Standring, Susan (2016). Gray's Anatomy: The Anatomical Basis of Clinical Practice (41st ed.). [Philadelphia]. ISBN 9780702052309. OCLC 920806541.
- Elsayes, Khaled M.; Menias, Christine O.; Harvin, Howard J.; Francis, Isaac R. (July 2007). "Imaging manifestations of Meckel's diverticulum". AJR. American Journal of Roentgenology. 189 (1): 81–88. doi:10.2214/AJR.06.1257. ISSN 1546-3141. PMID 17579156.
- Sagar, Jayesh; Kumar, Vikas; Shah, D. K. (October 2006). "Meckel's diverticulum: a systematic review". Journal of the Royal Society of Medicine. 99 (10): 501–505. doi:10.1258/jrsm.99.10.501. ISSN 0141-0768. PMC 1592061. PMID 17021300.
- Yam, Julie; Ahmad, Sarah A. (2019), "Esophageal Diverticula", StatPearls, StatPearls Publishing, PMID 30422453, retrieved 2019-07-17
- O'Rourke, Ashli K.; Weinberger, Paul M.; Postma, Gregory N. (May 2012). "Killian-Jamieson diverticulum". Ear, Nose, & Throat Journal. 91 (5): 196. doi:10.1177/014556131209100507. ISSN 1942-7522. PMID 22614553.
- Feuerstein, Joseph D.; Falchuk, Kenneth R. (August 2016). "Diverticulosis and Diverticulitis". Mayo Clinic Proceedings. 91 (8): 1094–1104. doi:10.1016/j.mayocp.2016.03.012. ISSN 1942-5546. PMID 27156370.
- Barat, M.; Dohan, A.; Dautry, R.; Barral, M.; Boudiaf, M.; Hoeffel, C.; Soyer, P. (October 2017). "Mass-forming lesions of the duodenum: A pictorial review". Diagnostic and Interventional Imaging. 98 (10): 663–675. doi:10.1016/j.diii.2017.01.004.
- Stunell, H; Buckley, O; Geoghegan, T; O’Brien, J; Ward, E; Torreggiani, W (2008). "Imaging of adenomyomatosis of the gall bladder". Journal of Medical Imaging and Radiation Oncology. 52 (2): 109–117. doi:10.1111/j.1440-1673.2008.01926.x. ISSN 1754-9477. PMID 18373800.
- Shah, Jamil; Patel, Kalpesh; Sunkara, Tagore; Papafragkakis, Charilaos; Shahidullah, Abul (April 2019). "Gastric Diverticulum: A Comprehensive Review". Inflammatory Intestinal Diseases. 3 (4): 161–166. doi:10.1159/000495463. ISSN 2296-9365. PMC 6501548. PMID 31111031.
- Oxford American Handbook of Urology. Albala, David M. Oxford: Oxford University Press. 2011. ISBN 9780199707720. OCLC 655896560.CS1 maint: others (link)
- Greiman, Alyssa K.; Rolef, Jennifer; Rovner, Eric S. (2019-01-02). "Urethral diverticulum: A systematic review". Arab Journal of Urology. 17 (1): 49–57. doi:10.1080/2090598X.2019.1589748. ISSN 2090-598X. PMC 6583718. PMID 31258943.
- Vazquez-Jimenez, Dr. Jaime (2003). "Cardiac diverticulum" (PDF). Orphanet Encyclopedia. Retrieved 2008-01-14.
- Raymond, Steven L.; Gray, Sarah E.; Peters, Keith R.; Fatima, Javairiah (2019-06-25). "Right-sided aortic arch with aberrant left subclavian artery and Kommerell diverticulum". Journal of Vascular Surgery Cases and Innovative Techniques. 5 (3): 259–260. doi:10.1016/j.jvscit.2019.02.009. ISSN 2468-4287. PMC 6600077. PMID 31304436.
- "UOTW #56 - Ultrasound of the Week". Ultrasound of the Week. 21 August 2015.