Type 3 diabetes
Type 3 diabetes is a proposed term to describe the interlinked association between type 1, type 2 diabetes and Alzheimer’s disease.[1] This term is used to look into the triggers of Alzheimer’s disease in people with diabetes.[1]
| Type 3 diabetes | |
|---|---|
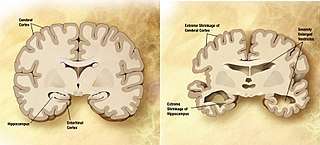 | |
| Diagram showing late stages of Alzheimer's disease in the brain caused by type 3 diabetes | |
| Specialty | Neurology |
| Symptoms | Memory loss, linguistic problems, mood and behavioural swings and motivational loss |
| Usual onset | from early childhood/adolescence onward |
| Duration | Long Term |
| Causes | type 1 diabetes, type 2 diabetes |
| Risk factors | Genetics and Lifestyle |
| Diagnostic method | Based on symptoms and cognitive testing after ruling out other possible causes |
| Prevention | Diet, physical and mental exercise, yoga and meditation and psychological well being |
| Medication | Melatonin or Glucagon-like Peptide 1 Administration (small benefit) |
| Frequency | Unknown |
The symptoms follow the same progression as Alzheimer’s disease, beginning with difficulty remembering recent events and as the disease progresses, linguistic problems, mood and behavioural swings and motivational loss can also be apparent.[2]
The progression from diabetes to Alzheimer’s disease is inadequately understood however there are a number of hypotheses describing the cause, progression and link between the two diseases.[3] The internal mechanism Insulin resistance and other metabolic risk factors such as hyperglycaemia, caused by oxidative stress and lipid peroxidation are common processes thought to be contributors to the development of Alzheimer’s disease in diabetics.[3]
Diagnosis for this disease is different between patients with type 1 and type 2 diabetes. type 1 diabetes is usually discovered in children and adolescence while type 2 diabetic patients are often diagnosed later in life.[3] Formal diagnosis is can be established through observational signs and neuroimaging techniques such as Diffusion Tensor Imaging (DTI) to observe abnormalities in diabetic patient’s brain tissue.[3]
The techniques used to prevent the disease in patients with diabetes are similar to individuals who do not show signs of the disease.[4] The four pillars of Alzheimer’s disease prevention is currently used as a guide for individuals of whom are at risk of developing Alzheimer’s disease.
Research into the effectiveness of Glucagon-like Peptide 1and Melatonin administration to manage the progression of Alzheimer’s disease in diabetic patients is currently being conducted to decrease the rate at which Alzheimer’s disease progresses.[5]
Signs and symptoms
The symptoms of the proposed disease are identical to Alzheimer’s disease.[3] Overtime an individual will show a progressive pattern of cognitive impairment and decline.[6]
The progression of this disease varies from person to person. It’s the prevalence of symptoms is dependent on when the individual is diagnosed with diabetes.[7] Individuals with type 1 diabetes are often diagnosed at a young age, usually between childhood and adolescence.[3] In some cases, brain development in these patients is negatively impacted, therefore showing symptoms of the disease earlier in life.[3] Symptoms of type 2 diabetes is characteristically seen in patients in their mid-sixties, leading to the prevalence of symptoms later in life.[8] The early stages of the disease are often associated with memory loss however other areas such as loss in judgment and reasoning and spatial and visual issues are often early symptoms of the disease.[8] As the individual ages, symptoms characteristically progress to more severe memory loss, poor judgement in making decisions, mood swings and in some cases patients are more susceptible to anxiety and/ or depression.[8] In the final cases of the disease, severe and more prominent symptoms are shown. In these cases the individual has completely lost their independence and will be reliant on others as their body begins to fail.[8] Inability to communicate, Seizures, weight loss and loss of bowel control are the final symptoms.[8] However in most cases, aspiration pneumonia, ulcers or untreated infections are the cause of death for these patients [4]
Cause
There are a number of mechanisms that attempt to explain the cause, progression and the link between type 1 diabetes, type 2 diabetes and Alzheimer’s disease [7][3][1][9]
Insulin resistance
Insulin resistance reduces the body’s sensitivity to insulin. This is a sign an individual has prediabetes or has progressed to develop type 2 diabetes.[7] The result is high glucose levels in the blood which leave the individual feeling tired and weak in most cases.[7] type 3 diabetes is a condition which can follow after initially being diagnosed with type 2 diabetes. In type 3 diabetes, the neurons lack glucose, a key element needed for the neurons to function effectively in body however more specifically the hippocampus and the cerebral cortex.[3][9] This deficiency can lead to a decrease in memory, judgement and the ability to reason, of which are key symptoms of Alzheimer’s disease.[7]
Hyperglycemia caused by oxidative stress
The consumption of carbohydrates, fatty (unsaturated) acids, small antioxidant consumption and little exercise are diabetic factors that contribute to oxidative stress within the brain.[1] Oxidative stress is an imbalance of free radicals such as superoxide, hydroxyl radical and nitric oxide radical which can create damage to the cells and tissue in the body.[10][1] This resulting imbalance leads to a slow decrease in cognition which can be severe in patients in type 2 diabetes.[1]
Lipid peroxidation
type 2 diabetes causes change in patient’s blood profile which increases the likelihood of the patient’s cells to experience damage through lipid peroxidation.[11] Lipid peroxidation involves free radicals taking electrons from lipids in the cell membrane, causing cell destruction.[1] This process has been observed in patients with Alzheimer’s disease.[1] One of the main biomarkers of oxidative stress is lipid peroxidation as acids including polyunsaturated fatty acids are known to characteristically associate with free radicals.[11] Therefore lipid peroxidation can cause enhancements in oxidative stress, a main process in type 2 diabetes and Alzheimer’s disease.
Diagnosis
A minor to medium decline in cognitive function is found to be linked with both type 1 diabetes and type 2 diabetes.[1] However substantial variances in the cognitive pathophysiology of both type 1 diabetes and type 2 diabetes, leading to impairment.[12] type 2 diabetes is characteristically diagnosed from within the late fifties to mid-sixties age range however it is possible to be diagnosed younger.[12] This form of diabetes is typically related to insulin resistance, dyslipidemia, hypertension and obesity. These mechanisms have a harmful influence on brain development.[8]
type 1 diabetes is typically detected at a from a young age and may have negative impacts on cognitive growth. In both forms of diabetes, microvascular complications and hyperglycaemia are mutual risk factors that are found to contribute to the cognitive decline in patients.[8]
Prevention
There is no evidence today supporting a definitive method for preventing the onset of Alzheimer’s disease in diabetic patients. However the four pillars of Alzheimer’s prevention which outlines diet, physical and mental exercise, yoga and meditation and psychological well being is recommended to patients whom are at risk.[6][13]
Diet
People who alter their ways of eating from a meat and fat heavy diet to a primarily plant based one can decrease the progression of early signs of Alzheimer’s disease.[6] Mediterranean diet, a diet based around fruit, vegetables, olive oil, nuts and seafood has been shown to lower the risks of Alzheimer’s disease in patients.[6] Specifically, patients who followed this diet which is modeled on particular Mediterranean nations presented decreasing amounts of amyloid-beta plaques between their nerve cells in the brain,[13] signifying the cell connections within the brain were firing correctly. This diet also presented increases in the thickness in the memory division of the brain cortex in the formal and parietal lobes and areas of cognition such as language and memory.[13] Updated versions of the Mediterranean diet such as the DASH diet have been recommended for patients, adding juicing and supplements to the recommendation for patients.[13]
Physical and mental exercise
.jpg)
Physical exercise increases the amount of blood flow through the brain while simultaneously causing the growth of brain cells known as neurogenesis.[6][14] One hundred and twenty minutes of aerobic exercise and multiple strength sessions a week are suggested to maintain and increase memory function in the patient.[15] Mental stimulation is also recommended for patients.[15] Brain aerobic activities such as reading and puzzles are endorsed to test and stimulate cognitive functioning while creative activities like painting and viewing art also activate the conditioning of the brain [6][13]
Yoga and meditation
Mediation and yoga have been found to reduce stress, which is major element in the cause of Alzheimer’s disease.[6] Stress has a negative impact on a patient’s genes such as producing inflammation in the brain, a key component of Alzheimer’s Disease.[16] Simple twelve minute meditation each day reduces levels of stress in patients and extends the flow of blood to key areas of the brain responsible for memory performance.[6][16] Yoga also stimulates the Anterior Cingulate Gyrus, a key area in the brain which manages memory recall, stress, emotive and cognitive stability.
Psychological well being
Psychological well-being factors such as self-acceptance and confidence, personal growth, regular socialization and independence decrease the probability of mental decline and reduce inflammation within the brain.[17] Purpose in Life is now considered to increase the physiological health of patients with Alzheimer’s disease.[6] Optimistic emotions such as love, appreciation and kindness are known to lessen the stress response and maintain a healthy cognition throughout the rest of the patient's life [17]
Management
Melatonin administration

Melatonin is discharged by the Pineal Gland as a neurohormone.[5] Melatonin is a central hormone in the treatment of patients with Alzheimer’s disease as it adjusts sleep patterns that are abnormal, which occurs in over forty five percent of patients.[5][18] Melatonin affects type 3 diabetes by reducing harm caused by beta amyloid, regulating hyperglycaemia and insulin resistance in patients with diabetes and stopping blood brain barrier disruption caused by hyperglycaemia.[18] Through these processes, melatonin has been shown to lessen the progression of type 3 diabetes.
Glucagon-like Peptide 1 administration
The administration of the hormone Glucagon-like Peptide 1 has shown to control the deregulation of glucose metabolism in patients with Alzheimer’s disease.[19] This hormone can recover cerebral dysfunction in diabetes induced Alzheimer’s disease. The hormone Glucagon-like Peptide 1 can lessen the brain’s inflamed reaction caused by amyloid beta oxidative stress.[9][19] Glucagon-like Peptide 1 can also increase the rate of neurogenesis within the brains of Alzheimer’s patients.[9] Glucagon-like Peptide 1 has the possibility to increase the production of neurons to substitute impaired neurons within the brain.[9] This hormone can also decrease the brain’s insulin resistance in Alzheimer’s patients.[19]
References
- Kandimalla, Ramesh; Thirumala, Vani; Reddy, P. Hemachandra (2017-05-01). "Is Alzheimer's disease a Type 3 Diabetes? A critical appraisal". Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. Oxidative Stress and Mitochondrial Quality in Diabetes/Obesity and Critical Illness Spectrum of Diseases. 1863 (5): 1078–1089. doi:10.1016/j.bbadis.2016.08.018. ISSN 0925-4439. PMC 5344773. PMID 27567931.
- Burns, Alistair; Iliffe, Steve (2009-02-05). "Alzheimer's disease". BMJ. 338. doi:10.1136/bmj.b158. ISSN 0959-8138. PMID 19196745.
- Moheet, Amir; Mangia, Silvia; Seaquist, Elizabeth R. (2015). "Impact of diabetes on cognitive function and brain structure". Annals of the New York Academy of Sciences. 1353 (1): 60–71. doi:10.1111/nyas.12807. ISSN 1749-6632. PMC 4837888. PMID 26132277.
- Förstl, H.; Kurz, A. (1999-12-01). "Clinical features of Alzheimer's disease". European Archives of Psychiatry and Clinical Neuroscience. 249 (6): 288–290. doi:10.1007/s004060050101. ISSN 1433-8491.
- "Signing into eresources, The University of Sydney Library". login.ezproxy2.library.usyd.edu.au. doi:10.1186/s13041-017-0315-x. PMC 5539639. PMID 28764741. Retrieved 2020-05-29.
- Khalsa, Dharma Singh; Perry, George (2017-03-01). "The Four Pillars of Alzheimer's Prevention". Cerebrum: the Dana Forum on Brain Science. 2017. ISSN 1524-6205. PMC 5501038. PMID 28698774.
- "What is type 3 diabetes?". Diabetes NSW & ACT. 2019-08-30. Retrieved 2020-05-29.
- "What Are the Signs of Alzheimer's Disease?". National Institute on Aging. Retrieved 2020-05-29.
- Bae, Choon Sang; Song, Juhyun (November 2017). "The Role of Glucagon-Like Peptide 1 (GLP1) in Type 3 Diabetes: GLP-1 Controls Insulin Resistance, Neuroinflammation and Neurogenesis in the Brain". International Journal of Molecular Sciences. 18 (11): 2493. doi:10.3390/ijms18112493.
- Gemma, Carmelina; Vila, Jennifer; Bachstetter, Adam; Bickford, Paula C. (2007), Riddle, David R. (ed.), "Oxidative Stress and the Aging Brain: From Theory to Prevention", Brain Aging: Models, Methods, and Mechanisms, Frontiers in Neuroscience, CRC Press/Taylor & Francis, ISBN 978-0-8493-3818-2, PMID 21204345, retrieved 2020-05-29
- de la Monte, Suzanne M.; Wands, Jack R. (November 2008). "Alzheimer's Disease Is Type 3 Diabetes–Evidence Reviewed". Journal of diabetes science and technology (Online). 2 (6): 1101–1113. ISSN 1932-2968. PMC 2769828. PMID 19885299.
- Srikanth, Velandai. "Why Alzheimer's Disease Is Called Type 3 Diabetes". Science Direct. Retrieved 2020-05-29.
- "Signing into eresources, The University of Sydney Library". login.ezproxy1.library.usyd.edu.au. doi:10.1016/j.jalz.2016.06.2359. PMC 5259552. PMID 27461490. Retrieved 2020-05-29.
- "Signing into eresources, The University of Sydney Library". login.ezproxy1.library.usyd.edu.au. doi:10.1177/2158244016631799. Retrieved 2020-05-29.
- Paillard, Thierry; Rolland, Yves; de Souto Barreto, Philipe (2015-07-01). "Protective Effects of Physical Exercise in Alzheimer's Disease and Parkinson's Disease: A Narrative Review". Journal of Clinical Neurology. 11 (3): 212–219. doi:10.3988/jcn.2015.11.3.212. ISSN 1738-6586. PMC 4507374. PMID 26174783.
- "Signing into eresources, The University of Sydney Library". login.ezproxy1.library.usyd.edu.au. Retrieved 2020-05-29.
- Cd, Ryff; Bh, Singer; G, Dienberg Love (2004-09-29). "Positive Health: Connecting Well-Being With Biology". Philosophical transactions of the Royal Society of London. Series B, Biological sciences. PMID 15347530. Retrieved 2020-05-29.
- McMullan, Ciaran J.; Schernhammer, Eva S.; Rimm, Eric B.; Hu, Frank B.; Forman, John P. (2013-04-03). "Melatonin Secretion and the Incidence of Type 2 Diabetes". JAMA. 309 (13): 1388–1396. doi:10.1001/jama.2013.2710. ISSN 0098-7484.
- Femminella, Grazia Daniela; Bencivenga, Leonardo; Petraglia, Laura; Visaggi, Lucia; Gioia, Lucia; Grieco, Fabrizio Vincenzo; de Lucia, Claudio; Komici, Klara; Corbi, Graziamaria (2017-06-01). "Antidiabetic Drugs in Alzheimer's Disease: Mechanisms of Action and Future Perspectives". Journal of Diabetes Research. doi:10.1155/2017/7420796. PMC 5471577. PMID 28656154. Retrieved 2020-05-29.