Trophoblast
Trophoblasts (from Greek 'trephein': to feed; and 'blastos': germinator) are cells that form the outer layer of a blastocyst and are present four days post fertilization in humans. They provide nutrients to the embryo and develop into a large part of the placenta. They form during the first stage of pregnancy and are the first cells to differentiate from the fertilized egg to become extraembryonic structures and do not directly contribute to the embryo. After gastrulation, the trophoblast is contiguous with the ectoderm of the embryo, and is referred to as the trophectoderm. After the first differentiation, the cells in the human embryo lose their totipotency and are no longer totipotent stem cells because they cannot form a trophoblast. They are now pluripotent stem cells.
| Trophoblast | |
|---|---|
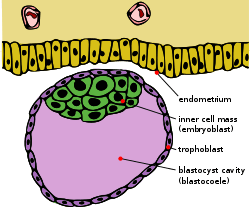 Blastocyst with an inner cell mass and trophoblast. | |
| Details | |
| Days | 6 |
| Gives rise to | caul |
| Identifiers | |
| Latin | trophoblastus; massa cellularis externa |
| MeSH | D014327 |
| TE | E6.0.1.1.2.0.2 |
| FMA | 83029 |
| Anatomical terminology | |
Structure
The trophoblast proliferates and differentiates into two cell layers at approximately six days after fertilization for humans.
| Layer | Location | Description |
| Cytotrophoblast | The inner layer | A single-celled inner layer of the trophoblast. |
| Syncytiotrophoblast | The outer layer | A thick layer that lacks cell boundaries and grows into the endometrial stroma. It secretes hCG in order to maintain progesterone secretion and sustain a pregnancy. |
| Intermediate trophoblast (IT) | The implantation site, chorion, villi (dependent on subtype) | An anchor placenta (implantation site IT). |
Function
Trophoblasts are specialized cells of the placenta that play an important role in embryo implantation and interaction with the decidualized maternal uterus. The core of placental villi contain mesenchymal cells and placental blood vessels that are directly connected to the fetus’ circulation via the umbilical cord. This core is surrounded by two layers of trophoblasts, the cytotrophoblast and the syncytiotrophoblast. The cytotrophoblast is a layer of mono-nucleated cells that resides underneath the syncytiotrophoblast.[1] The syncytiotrophoblast is composed of fused cytotrophoblasts which forms a layer that covers the placental surface.[1] The syncytiotrophoblast is in direct contact with the maternal blood that reaches the placental surface. It then facilitates the exchange of nutrients, wastes and gases between the maternal and fetal systems.
In addition, cytotrophoblasts in the tips of villi can differentiate into another type of trophoblast called the extravillous trophoblast. Extravillous trophoblasts grow out from the placenta and penetrate into the decidualized uterus. This process is essential not only for physically attaching the placenta to the mother, but also for altering the vasculature in the uterus. This alteration allows an adequate blood supply to the growing fetus as pregnancy progresses. Some of these trophoblasts even replace the endothelial cells in the uterine spiral arteries as they remodel these vessels into wide bore conduits that are independent of maternal vasoconstriction. This ensures that the fetus receives a steady supply of blood, and the placenta is not subjected to fluctuations in oxygen that could cause it damage.[2]
Clinical significance
The invasion of a specific type of trophoblast (extravillous trophoblast) into the maternal uterus is a vital stage in the establishment of pregnancy. Failure of the trophoblast to invade sufficiently is important in the development of some cases of pre-eclampsia. Invasion of the trophoblast too deeply may cause conditions such as placenta accreta, placenta increta, or placenta percreta.
Gestational trophoblastic disease is a pregnancy-associated concept, forming from the villous and extravillous trophoblast cells in the placenta.[3]
Choriocarcinoma are trophoblastic tumors that form in the uterus from villous cells.[3]
Trophoblast stem cells (TSCs) are cells that can regenerate and they are similar to embryonic stem cells (ESCs) in the fact that they come from early on in the trophoblast lifetime.[4] In the placenta, these stem cells are able to differentiate into any trophoblast cell because they are pluripotent.[4]
Additional images
 Blastodermic vesicle of Vespertilio murinus.
Blastodermic vesicle of Vespertilio murinus. Section through embryonic disk of Vespertilio murinus.
Section through embryonic disk of Vespertilio murinus.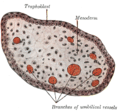 Transverse section of a chorionic villus.
Transverse section of a chorionic villus.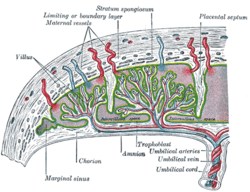 Scheme of placental circulation.
Scheme of placental circulation.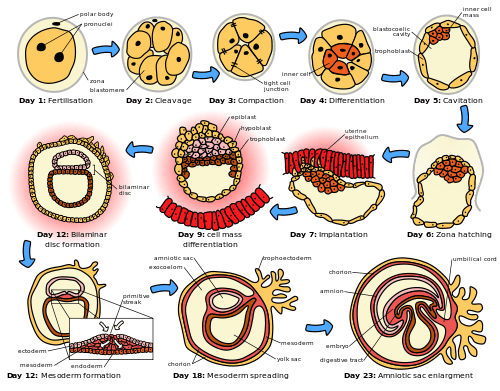 The initial stages of human embryogenesis
The initial stages of human embryogenesis
See also
- Syncytiotrophoblast
- Hydatidiform mole
References
- "The trophoblast". www.embryology.ch. Retrieved 2020-04-16.
- Lunghi, Laura; Ferretti, Maria E.; Medici, Silvia; Biondi, Carla; Vesce, Fortunato (2007-02-08). "Control of human trophoblast function". Reproductive Biology and Endocrinology. 5 (1): 6. doi:10.1186/1477-7827-5-6. ISSN 1477-7827. PMC 1800852. PMID 17288592.
- Ning, Fen; Hou, Houmei; Morse, Abraham N.; Lash, Gendie E. (2019-04-10). "Understanding and management of gestational trophoblastic disease". F1000Research. 8: 428. doi:10.12688/f1000research.14953.1. ISSN 2046-1402. PMC 6464061. PMID 31001418.
- Latos, P. A.; Hemberger, M. (2014-02-01). "Review: The transcriptional and signalling networks of mouse trophoblast stem cells". Placenta. Models for Molecular Understanding of Placental Development and Associated Disorders. 35: S81–S85. doi:10.1016/j.placenta.2013.10.013. ISSN 0143-4004. PMID 24220516.
External links
- Swiss embryology (from UL, UB, and UF) iperiodembry/carnegie02