Quality-adjusted life year
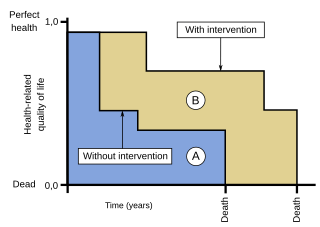
The quality-adjusted life year or quality-adjusted life-year (QALY) is a generic measure of disease burden, including both the quality and the quantity of life lived.[1][2] It is used in economic evaluation to assess the value of medical interventions.[1] One QALY equates to one year in perfect health.[2] QALY scores range from 1 (perfect health) to 0 (dead).[3] QALYs can be used to inform personal decisions, to evaluate programs, and to set priorities for future programs.[3]
Critics point out that the QALY figures oversimplify how actual patients would assess risks and outcomes. Proponents of the approach acknowledge its imperfections but consider the QALY better than alternative measures.
Calculation
The QALY is a measure of the value of health outcomes. It assumes that health is a function of length of life and quality of life, and combines these values into a single index number. To determine QALYs, one multiplies the utility value associated with a given state of health by the years lived in that state. A year of life lived in perfect health is worth 1 QALY (1 year of life × 1 Utility value). A year of life lived in a state of less than perfect health is worth less than 1 QALY; for example, 1 year of life lived in a situation with utility 0.5 (e.g. bedridden, 1 year × 0.5 Utility) is assigned 0.5 QALYs. Similarly, half a year lived in perfect health is equivalent to 0.5 QALYs (0.5 years × 1 Utility). Death is assigned a value of 0 QALYs, and in some circumstances it is possible to accrue negative QALYs to reflect health states deemed "worse than dead."[3]
Weighting
The "weight" (utility) values between 0 and 1 are usually determined by methods such as those proposed in the Journal of Health Economics:[4]
- Time-trade-off (TTO): Respondents are asked to choose between remaining in a state of ill health for a period of time, or being restored to perfect health but having a shorter life expectancy.
- Standard gamble (SG): Respondents are asked to choose between remaining in a state of ill health for a period of time, or choosing a medical intervention which has a chance of either restoring them to perfect health or killing them.
- Visual analogue scale (VAS): Respondents are asked to rate a state of ill health on a scale from 0 to 100, with 0 representing being dead and 100 representing perfect health. This method has the advantage of being the easiest to ask, but is the most subjective.
Another way of determining the weight associated with a particular health state is to use standard descriptive systems such as the EuroQol Group's EQ-5D questionnaire, which categorises health states according to five dimensions: mobility, self-care, usual activities (e.g. work, study, homework or leisure activities), pain/discomfort and anxiety/depression.[5]
Use
Data on medical costs are often combined with QALYs in cost-utility analysis to estimate the cost-per-QALY associated with a health care intervention. This parameter can be used to develop a cost-effectiveness analysis of any treatment. This incremental cost-effectiveness ratio (ICER) can then be used to allocate healthcare resources, often using a threshold approach.[6]
In the United Kingdom, the National Institute for Health and Care Excellence, which advises on the use of health technologies within the National Health Service, has since at least 2013 used "£ per QALY" to evaluate their utility.[1][7]
History
QALY is credited to work by Klarman et al. (1968)[8], Fanshel and Bush (1970)[9] and Torrance et al. (1972)[10] who suggested the idea of length of life adjusted by indices of functionality or health.[11] A 1976 article by Zeckhauser and Shepard[12] was the first appearance in print of the term.[13] QALYs were later promoted through medical technology assessments conducted by the US Congress Office of Technology Assessment.
In 1980, Pliskin et al. justified the QALY indicator using multiattribute utility theory: if a set of conditions pertaining to agent preferences on life years and quality of life are verified, then it is possible to express the agent's preferences about couples (number of life years/health state), by an interval (Neumannian) utility function.[14] This utility function would be equal to the product of an interval utility function on "life years", and an interval utility function on "health state".
Debate
According to Pliskin et al., the QALY model requires utility independent, risk neutral, and constant proportional tradeoff behaviour.[14] Because of these theoretical assumptions, the meaning and usefulness of the QALY is debated.[15][16] Perfect health is difficult, if not impossible, to define. Some argue that there are health states worse than being dead, and that therefore there should be negative values possible on the health spectrum (indeed, some health economists have incorporated negative values into calculations). Determining the level of health depends on measures that some argue place disproportionate importance on physical pain or disability over mental health.[17]
The method of ranking interventions on grounds of their cost per QALY gained ratio (or ICER) is controversial because it implies a quasi-utilitarian calculus to determine who will or will not receive treatment.[18] However, its supporters argue that since health care resources are inevitably limited, this method enables them to be allocated in the way that is approximately optimal for society, including most patients. Another concern is that it does not take into account equity issues such as the overall distribution of health states – particularly since younger, healthier cohorts have many times more QALYs than older or sicker individuals. As a result, QALY analysis may undervalue treatments which benefit the elderly or others with a lower life expectancy. Also, many would argue that all else being equal, patients with more severe illness should be prioritised over patients with less severe illness if both would get the same absolute increase in utility.[19]
As early as 1989, Loomes and McKenzie recommended that research be conducted concerning the validity of QALYs.[20] In 2010, with funding from the European Commission, the European Consortium in Healthcare Outcomes and Cost-Benefit Research (ECHOUTCOME) began a major study on QALYs as used in health technology assessment.[21] Ariel Beresniak, the study's lead author, was quoted as saying that it was the "largest-ever study specifically dedicated to testing the assumptions of the QALY."[22] In January 2013, at its final conference, ECHOUTCOME released preliminary results of its study which surveyed 1361 people "from academia" in Belgium, France, Italy and the UK.[22][23][24] The researchers asked the subjects to respond to 14 questions concerning their preferences for various health states and durations of those states (e.g., 15 years limping versus 5 years in a wheelchair).[24] They concluded that "preferences expressed by the respondents were not consistent with the QALY theoretical assumptions" that quality of life can be measured in consistent intervals, that life-years and quality of life are independent of each other, that people are neutral about risk, and that willingness to gain or lose life-years is constant over time.[24] ECHOUTCOME also released "European Guidelines for Cost-Effectiveness Assessments of Health Technologies," which recommended not using QALYs in healthcare decision making.[25] Instead, the guidelines recommended that cost-effectiveness analyses focus on "costs per relevant clinical outcome."[22][25]
In response to the ECHOUTCOME study, representatives of the National Institute for Health and Care Excellence, the Scottish Medicines Consortium, and the Organisation for Economic Co-operation and Development made the following points. First, QALYs are better than alternative measures.[22][23] Second, the study was "limited."[22][23] Third, problems with QALYs were already widely acknowledged.[23] Fourth, the researchers did not take budgetary constraints into consideration.[23] Fifth, the UK's National Institute for Health and Care Excellence uses QALYs that are based on 3395 interviews with residents of the UK, as opposed to residents of several European countries.[22] Finally, according to Franco Sassi, a senior health economist at the Organisation for Economic Co-operation and Development, people who call for the elimination of QALYs may have "vested interests."[22]
Future development
The UK Medical Research Council and others are exploring improvements to or replacements for QALYs.[26] Among other possibilities are extending the data used to calculate QALYs (e.g., by using different survey instruments); "using well-being to value outcomes" (e.g., by developing a "well-being-adjusted life-year"; and by value outcomes in monetary terms.[26] In 2018 HM Treasury set a discount rate of 1.5% for QALYs which is lower than the discount rate for other costs and benefits, because the QALY is a direct utility measure.[27]
See also
- Case mix index
- Cost-Effectiveness Analysis Registry
- Cost-utility analysis
- Disability-adjusted life year (DALY)
- Incremental cost-effectiveness ratio
- Quality of life and measurements such as MANSA and Life Quality Index
References
- "Judging whether public health interventions offer value for money". National Institute for Health and Care Excellence. September 2013. Retrieved 2017-05-30.
- "Glossary". National Institute for Health and Care Excellence. Retrieved 2017-05-30.
- Weinstein, Milton C.; Torrance, George; McGuire, Alistair (2009). "QALYs: The Basics". Value in Health. 12: S5–S9. doi:10.1111/j.1524-4733.2009.00515.x. ISSN 1098-3015. PMID 19250132.
- Torrance, George E. (1986). "Measurement of health state utilities for economic appraisal: A review". Journal of Health Economics. 5 (1): 1–30. doi:10.1016/0167-6296(86)90020-2. PMID 10311607.
- EuroQol Group (1990-12-01). "EuroQol--a new facility for the measurement of health-related quality of life". Health Policy (Amsterdam, Netherlands). 16 (3): 199–208. doi:10.1016/0168-8510(90)90421-9. ISSN 0168-8510. PMID 10109801.
- Weinstein, Milton; Zeckhauser, Richard (1973-04-01). "Critical ratios and efficient allocation". Journal of Public Economics. 2 (2): 147–157. doi:10.1016/0047-2727(73)90002-9.
- "Guide to the methods of technology appraisal 2013". NICE. 2013. Archived from the original on 7 May 2015. Retrieved 15 Jun 2015.
- Klarman, Herbert E.; Francis, John O'S; Rosenthal, Gerald D. (1968). "Cost effectiveness analysis applied to the treatment of chronic renal disease". Medical Care. 6 (1): 48–54. doi:10.1097/00005650-196801000-00005.
- Fanshel, Sol; Bush, J.W. (1970). "A health-status index and its application to health-services outcomes" (PDF). Operations Research. 18 (6): 1021–66. doi:10.1287/opre.18.6.1021. Retrieved 2014-05-06.
- Torrance, G W; Thomas, W.H.; Sackett, D.L. (1972). "A utility maximization model for evaluation of health care programs". Health Services Research. 7 (2): 118–133. ISSN 0017-9124. PMC 1067402. PMID 5044699.
- Kaplan, Robert M. (1995). "Utility assessment for estimating quality-adjusted life years" (PDF). Valuing health care: Costs, benefits, and effectiveness of pharmaceuticals and other medical technologies. pp. 31–60. Retrieved 2014-05-06.
- Zeckhauser, Richard; Shepard, Donald (1976). "Where Now for Saving Lives?". Law and Contemporary Problems. 40 (4): 5–45. doi:10.2307/1191310. ISSN 0023-9186. JSTOR 1191310.
- Sassi, Franco (2006). "Calculating QALYs, comparing QALY and DALY calculations". Health Policy and Planning. 21 (5): 402–408. doi:10.1093/heapol/czl018. ISSN 0268-1080. PMID 16877455.
- Pliskin, J. S.; Shepard, D. S.; Weinstein, M. C. (1980). "Utility Functions for Life Years and Health Status". Operations Research. 28 (1): 206–24. doi:10.1287/opre.28.1.206. JSTOR 172147.
- Prieto, Luis; Sacristán, José A (2003). "Problems and solutions in calculating quality-adjusted life years (QALYs)". Health and Quality of Life Outcomes. 1: 80. doi:10.1186/1477-7525-1-80. PMC 317370. PMID 14687421.

- Mortimer, D.; Segal, L. (2007). "Comparing the Incomparable? A Systematic Review of Competing Techniques for Converting Descriptive Measures of Health Status into QALY-Weights". Medical Decision Making. 28 (1): 66–89. doi:10.1177/0272989X07309642. PMID 18263562.
- Dolan, P (January 2008). "Developing methods that really do value the 'Q' in the QALY" (PDF). Health Economics, Policy and Law. 3 (1): 69–77. doi:10.1017/S1744133107004355. PMID 18634633.
- Schlander, Michael (2010-05-23), Measures of efficiency in healthcare: QALMs about QALYs?, Institute for Innovation & Valuation in Health Care, archived from the original (PDF) on 2016-10-25, retrieved 2010-05-23
- Nord, Erik; Pinto, Jose Luis; Richardson, Jeff; Menzel, Paul; Ubel, Peter (1999). "Incorporating societal concerns for fairness in numerical valuations of health programmes". Health Economics. 8 (1): 25–39. doi:10.1002/(SICI)1099-1050(199902)8:1<25::AID-HEC398>3.0.CO;2-H. PMID 10082141.
- Loomes, Graham; McKenzie, Lynda (1989). "The use of QALYs in health care decision making". Social Science & Medicine. 28 (4): 299–308. doi:10.1016/0277-9536(89)90030-0. ISSN 0277-9536. PMID 2649989.
- "ECHOUTCOME: European Consortium in Healthcare Outcomes and Cost-Benefit Research". Archived from the original on 2016-10-08.
- Holmes, David (March 2013). "Report triggers quibbles over QALYs, a staple of health metrics". Nature Medicine. 19 (3): 248. doi:10.1038/nm0313-248. PMID 23467219.
- Dreaper, Jane (24 January 2013). "Researchers claim NHS drug decisions 'are flawed'". BBC News. Retrieved 2017-05-30.
- Beresniak, Ariel; Medina-Lara, Antonieta; Auray, Jean Paul; De Wever, Alain; Praet, Jean-Claude; Tarricone, Rosanna; Torbica, Aleksandra; Dupont, Danielle; Lamure, Michel; Duru, Gerard (2015). "Validation of the Underlying Assumptions of the Quality-Adjusted Life-Years Outcome: Results from the ECHOUTCOME European Project". PharmacoEconomics. 33 (1): 61–69. doi:10.1007/s40273-014-0216-0. ISSN 1170-7690. PMID 25230587.
- European Consortium in Healthcare Outcomes and Cost-Benefit Research (ECHOUTCOME). "European Guidelines for Cost-Effectiveness Assessments of Health Technologies" (PDF). Archived from the original (PDF) on 2015-08-14.
- Brazier, John; Tsuchiya, Aki (2015). "Improving Cross-Sector Comparisons: Going Beyond the Health-Related QALY". Applied Health Economics and Health Policy. 13 (6): 557–565. doi:10.1007/s40258-015-0194-1. ISSN 1175-5652. PMC 4661222. PMID 26324402.
- "HMT Green Book". p. 28.