Parsonage–Turner syndrome
Parsonage–Turner syndrome, also known as acute brachial neuropathy and neuralgic amyotrophy, is a syndrome of unknown cause; although many specific risk factors have been identified (such as; post-operatively, post-infectious, post-traumatic or post-vaccination),[4] the cause is still unknown. The condition manifests as a rare set of symptoms most likely resulting from autoimmune inflammation of unknown cause of the brachial plexus.[5] (The brachial plexus is a complex network of nerves through which impulses reach the arms, shoulders and chest.)
| Parsonage–Turner syndrome | |
|---|---|
| Other names | acute brachial radiculitis,[1] Parsonage–Aldren–Turner syndrome', neuralgic amyotrophy,[2] brachial neuritis, brachial plexus neuropathy,[3] brachial plexitis, acute brachial neuropathy |
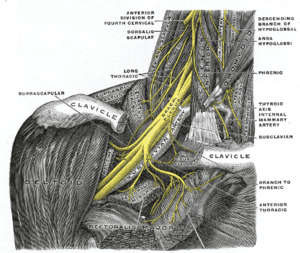 | |
| The right brachial plexus with its short branches, viewed from in front. | |
| Specialty | Neurology |
Parsonage–Turner syndrome occurs in about 1.6 people per 100,000 per year.[6]
Signs and symptoms
This syndrome can begin with severe shoulder or arm pain followed by weakness and numbness.[5] Those who suffer from Parsonage–Turner experience acute, sudden-onset pain radiating from the shoulder to the upper arm. Affected muscles become weak and atrophied, and in advanced cases, paralyzed. Occasionally, there will be no pain and just paralysis, and sometimes just pain, not ending in paralysis. MRI may assist in diagnosis.[7] Scapular winging is commonly seen.
Mechanism
Parsonage-Turner involves neuropathy of the suprascapular nerve in 97% of cases, and variably involves the axillary and subscapular nerves. As such, the muscles usually involved are the supraspinatus and infraspinatus, which are both innervated by the suprascapular nerve. Involvement of the deltoid is more variable, as it is innervated by the axillary nerve.[8]
Diagnosis
Differential diagnosis
The differential focuses on distinguishing it from similar entities such as quadrilateral space syndrome, which involves the teres minor and variably the deltoid, and suprascapular nerve impingement at the spinoglenoid notch, which predominantly involves the infraspinatus.[8]
Prognosis
Despite its wasting and at times long-lasting effects, most cases are resolved by the body's healing system, and recovery is usually good in 18–24 months, depending on how old the person in question is. For instance, a six-year-old could have brachial neuritis for only around 6 months, but a person in their early fifties could have it for over 3 years.
Eponym
It is named after Maurice Parsonage and John Turner.[9][10]
See also
References
- Wheeless, Clifford R. (30 August 2009). "Parsonage-Turner Syndrome". Wheeless' Textbook of Orthopedics @ wheelessonline.com. Retrieved 2009-10-11.
- Cary D. Alberstone; Michael Steinmetz; Edward C. Benzel (28 January 2009). Anatomic Basis of Neurologic Diagnosis. Thieme. pp. 105–. ISBN 978-0-86577-976-1. Retrieved 4 November 2010.
- Charles A. Rockwood (14 January 2009). The Shoulder. Elsevier Health Sciences. pp. 1376–. ISBN 978-1-4160-3427-8. Retrieved 4 November 2010.
- Feinberg JH, Radecki J (2010). "Parsonage-turner syndrome". HSS J. 6 (2): 199–205. doi:10.1007/s11420-010-9176-x. PMC 2926354. PMID 21886536.
- "NINDS Brachial Plexus Injuries: Information Page". National Institute of Neurological Disorders and Stroke. September 29, 2008. Retrieved 2009-10-11.
- Beghi E, Kurland LT, Mulder DW, Nicolosi A (1985). "Brachial plexus neuropathy in the population of Rochester, Minnesota, 1970-1981". Ann. Neurol. 18 (3): 320–3. doi:10.1002/ana.410180308. PMID 2996415.
- William E. Brant; Clyde A. Helms (2007). Fundamentals of diagnostic radiology. Lippincott Williams & Wilkins. pp. 1–. ISBN 978-0-7817-6135-2. Retrieved 4 November 2010.
- Frank Gaillard MD. "Parsonage-Turner syndrome". Radiopaedia.
- synd/1910 at Who Named It?
- Parsonage MJ, Turner JW (June 1948). "Neuralgic amyotrophy; the shoulder-girdle syndrome". Lancet. 1 (6513): 973–8. doi:10.1016/S0140-6736(48)90611-4. PMID 18866299.