Formylglycine-generating enzyme
Formylglycine-generating enzyme (FGE), located at 3p26.1 in humans, is the name for an enzyme present in the endoplasmic reticulum that catalyzes the conversion of cysteine to formylglycine (fGly).[1] There are two main classes of FGE, aerobic and anaerobic. FGE activates sulfatases, which are essential for the degradation of sulfate esters. The catalytic activity of sulfatases is dependent upon a formylglycine (sometimes called oxoalanine) residue in the active site.[2]
| Formylglycine-generating enzyme | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Identifiers | |||||||||
| EC number | 1.8.99 | ||||||||
| Databases | |||||||||
| IntEnz | IntEnz view | ||||||||
| BRENDA | BRENDA entry | ||||||||
| ExPASy | NiceZyme view | ||||||||
| KEGG | KEGG entry | ||||||||
| MetaCyc | metabolic pathway | ||||||||
| PRIAM | profile | ||||||||
| PDB structures | RCSB PDB PDBe PDBsum | ||||||||
| |||||||||
| Formylglycine-generating enzyme | |||||||||
|---|---|---|---|---|---|---|---|---|---|
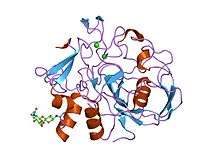 formylglycine generating enzyme c336s mutant covalently bound to substrate peptide lctpsra | |||||||||
| Identifiers | |||||||||
| Symbol | FGE-sulfatase | ||||||||
| Pfam | PF03781 | ||||||||
| InterPro | IPR005532 | ||||||||
| |||||||||
Aerobic
The aerobic enzyme has a structure homologous to the complex alpha/beta topology found in the gene product of human sulfatase-modifying factor 1 (SUMF1). Aerobic FGE converts a cysteine residue in the highly conserved consensus sequence CXPXR to fGly. To do so, FGE “activates” its target by utilizing mononuclear copper. The substrate first binds to copper, increasing reactivity of the substrate-copper complex with oxygen. Activation is then accomplished through oxidation of a cysteine residue in the substrate-copper complex. Due to the nature of this reaction, FGE is termed a “copper-dependent metalloenzyme.[3]

Anaerobic
The most well-studied anaerobic FGE is the bacterial AtsB, an iron-sulfur cluster containing enzyme present in Klebsiella pneumoniae, that is able to convert either cysteine or serine to fGly with a distinctly different mechanism than the aerobic form. While AtsB can convert either, its activity increases four fold when in the presence of cysteine over serine[4]. AtsB is 48% similar to an enzyme present in Clostridium perfringens.[5] Both enzymes possess the Cx3Cx2C motif unique to the radical S-adenosyl methionine superfamily and are able to use a reduction reaction to cleave S-adenosyl methionine. These two enzymes fall into a larger group called the anaerobic Sulfatase Maturing Enzymes, which are able to convert cysteine into fGly without the use of oxygen.
Protein domain
In molecular biology, "formylglycine-generating enzyme" (sometimes annotated as formylglycine-generating sulfatase enzyme) is the name of the FGE protein domain, whether or not the protein is catalytically active. Both prokaryotic and eukaryotic homologs of FGE possess highly conserved active sites — including the catalytic cysteine residues required for enzymatic function.[6] Activation of molecular oxygen is thought to be carried out by conserved residues close to the FGE catalytic site in aerobic organisms. The catalytic cysteine residues are involved in a thiol-cysteine exchange leading to the ultimate production of fGly[7].
Disease states
In humans, mutations in SUMF1 result in defects in FGE, which in turn causes the impairment of sulfatases. The result is a disease called multiple sulfatase deficiency (MSD), in which the accumulation of glycosaminoglycans or sulfolipids can cause early infant death.[8][9][10] This disease can be further differentiated into neonatal, late infantile, and juvenile, with neonatal being the most severe.[11] Common symptoms include ichthyosis, hypotonia, skeletal abnormalities, and overall cognitive decline.[12][13] In 2017 Weidner et. al., found an association with SUMF1 expression and chronic obstructive pulmonary disease (COPD) development.[14] As of January 2020, there were more than 100 reported cases worldwide cases of MSD.[15] Known substrates for SUMF1 are: N-acetylgalactosamine-6-sulfate sulfatase (GALNS), arylsulfatase A (ARSA), steroid sulfatase (STS) and arylsulfatase E (ARSE); all molecules that contain cysteine. FGE converts this cysteine group into C-𝛼-formylglycine.[16] SUMF1 occurs in the endoplasmic reticulum or its lumen.
References
- Reference, Genetics Home. "SUMF1 gene". Genetics Home Reference. Retrieved 2020-03-27.
- Roeser D, Dickmanns A, Gasow K, Rudolph MG (August 2005). "De novo calcium/sulfur SAD phasing of the human formylglycine-generating enzyme using in-house data". Acta Crystallogr. D. 61 (Pt 8): 1057–66. doi:10.1107/S0907444905013831. PMID 16041070.
- Appel, Mason J.; Meier, Katlyn K.; Lafrance-Vanasse, Julien; Lim, Hyeongtaek; Tsai, Chi-Lin; Hedman, Britt; Hodgson, Keith O.; Tainer, John A.; Solomon, Edward I.; Bertozzi, Carolyn R. (2019-03-19). "Formylglycine-generating enzyme binds substrate directly at a mononuclear Cu(I) center to initiate O2 activation". Proceedings of the National Academy of Sciences. 116 (12): 5370–5375. doi:10.1073/pnas.1818274116. ISSN 0027-8424. PMC 6431200. PMID 30824597.
- Appel, Mason J.; Bertozzi, Carolyn R. (2015-01-16). "Formylglycine, a Post-Translationally Generated Residue with Unique Catalytic Capabilities and Biotechnology Applications". ACS Chemical Biology. 10 (1): 72–84. doi:10.1021/cb500897w. ISSN 1554-8929. PMC 4492166. PMID 25514000.
- Benjdia, Alhosna; Leprince, Jérôme; Guillot, Alain; Vaudry, Hubert; Rabot, Sylvie; Berteau, Olivier (2007-03-01). "Anaerobic Sulfatase-Maturating Enzymes: Radical SAM Enzymes Able To Catalyze in Vitro Sulfatase Post-translational Modification". Journal of the American Chemical Society. 129 (12): 3462–3463. doi:10.1021/ja067175e. ISSN 0002-7863. PMID 17335281.
- Carlson, Brian L.; Ballister, Edward R.; Skordalakes, Emmanuel; King, David S.; Breidenbach, Mark A.; Gilmore, Sarah A.; Berger, James M.; Bertozzi, Carolyn R. (2008-07-18). "Function and Structure of a Prokaryotic Formylglycine-generating Enzyme". The Journal of Biological Chemistry. 283 (29): 20117–20125. doi:10.1074/jbc.M800217200. ISSN 0021-9258. PMC 2459300. PMID 18390551.
- Appel, Mason J.; Bertozzi, Carolyn R. (2015-01-16). "Formylglycine, a Post-Translationally Generated Residue with Unique Catalytic Capabilities and Biotechnology Applications". ACS Chemical Biology. 10 (1): 72–84. doi:10.1021/cb500897w. ISSN 1554-8929. PMC 4492166. PMID 25514000.
- Fraldi A, Biffi A, Lombardi A, Visigalli I, Pepe S, Settembre C, Nusco E, Auricchio A, Naldini L, Ballabio A, Cosma MP (April 2007). "SUMF1 enhances sulfatase activities in vivo in five sulfatase deficiencies". Biochem. J. 403 (2): 305–12. doi:10.1042/BJ20061783. PMC 1874239. PMID 17206939.
- Diez-Roux G, Ballabio A (2005). "Sulfatases and human disease". Annu Rev Genom Hum Genet. 6: 355–79. doi:10.1146/annurev.genom.6.080604.162334. PMID 16124866.
- Sardiello M, Annunziata I, Roma G, Ballabio A (November 2005). "Sulfatases and sulfatase modifying factors: an exclusive and promiscuous relationship". Hum. Mol. Genet. 14 (21): 3203–17. doi:10.1093/hmg/ddi351. PMID 16174644.
- Schlotawa, Lars; Ennemann, Eva Charlotte; Radhakrishnan, Karthikeyan; Schmidt, Bernhard; Chakrapani, Anupam; Christen, Hans-Jürgen; Moser, Hugo; Steinmann, Beat; Dierks, Thomas; Gärtner, Jutta (March 2011). "SUMF1 mutations affecting stability and activity of formylglycine generating enzyme predict clinical outcome in multiple sulfatase deficiency". European Journal of Human Genetics. 19 (3): 253–261. doi:10.1038/ejhg.2010.219. ISSN 1476-5438. PMC 3062010. PMID 21224894.
- Reference, Genetics Home. "SUMF1 gene". Genetics Home Reference. Retrieved 2020-03-27.
- Staretz‐Chacham, Orna; Schlotawa, Lars; Wormser, Ohad; Golan‐Tripto, Inbal; Birk, Ohad S.; Ferreira, Carlos R.; Dierks, Thomas; Radhakrishnan, Karthikeyan (2020). "A homozygous missense variant of SUMF1 in the Bedouin population extends the clinical spectrum in ultrarare neonatal multiple sulfatase deficiency". Molecular Genetics & Genomic Medicine. n/a (n/a): e1167. doi:10.1002/mgg3.1167. ISSN 2324-9269. PMID 32048457.
- Weidner, Julie; Jarenbäck, Linnea; de Jong, Kim; Vonk, Judith M.; van den Berge, Maarten; Brandsma, Corry-Anke; Boezen, H. Marike; Sin, Don; Bossé, Yohan; Nickle, David; Ankerst, Jaro (2017-05-02). "Sulfatase modifying factor 1 (SUMF1) is associated with Chronic Obstructive Pulmonary Disease". Respiratory Research. 18 (1): 77. doi:10.1186/s12931-017-0562-5. ISSN 1465-993X. PMC 5414362. PMID 28464818.
- Staretz‐Chacham, Orna; Schlotawa, Lars; Wormser, Ohad; Golan‐Tripto, Inbal; Birk, Ohad S.; Ferreira, Carlos R.; Dierks, Thomas; Radhakrishnan, Karthikeyan (2020). "A homozygous missense variant of SUMF1 in the Bedouin population extends the clinical spectrum in ultrarare neonatal multiple sulfatase deficiency". Molecular Genetics & Genomic Medicine. n/a (n/a): e1167. doi:10.1002/mgg3.1167. ISSN 2324-9269. PMID 32048457.
- Reference, Genetics Home. "SUMF1 gene". Genetics Home Reference. Retrieved 2020-03-27.