Food choice of older adults
Food preferences in older adults and seniors takes into consideration how people's experiences change with aging; that is, changes in taste, diet (nutrition) and food choice. Primarily, this occurs when most people approach the age of 70 or older. Influencing variables can include: social and cultural environment, male or female sex and personal habits as well as physical and mental health. Scientific studies attempting to explain why people like or dislike certain foods have been performed to further our understanding of these issues.
Science of food preferences
Research is continuously examining the variables that cause the elderly to change food preferences, one example being the Elderly Nutrition Program (ENP). To improve the quality of meal programs, the ENP explored how food preferences varied depending on biological sex and ethnic groups. A total of 2,024 participants in the ENP aged 60 years or older were interviewed. A majority of the participants were female, served by congregate meal programs, or meals served in community settings such as senior centers, churches or senior housing communities.
A general impression of the meals and preferences for 13 food groups (fresh fruit, chicken, soup, salad, vegetables, potatoes, meat, sandwiches, pasta, canned fruit, legumes, deli meats, and ethnic foods) were assessed. After adjusting for variables, older male subjects were found to be significantly more likely to prefer deli meats, meat, legumes, canned fruit, and ethnic foods compared to females. In addition, compared with African Americans, the study found that "... Caucasians demonstrated higher percentages of preference for 9 of 13 food groups including pasta, meat, and fresh fruit", and recommended that "... To improve the quality of the ENP, and to increase dietary compliance of the older adults to the programs, the nutritional services require a strategic meal plan that solicits and incorporates older adults' food preferences".[2]
Influences on food preference
There are multiple factors in an elderly person's life that can affect food preferences. Aspects like the environment, mental and physical health, and lifestyle choices can all contribute to the individual taste and/or habits of elderly persons.
An article about Influences On Cognitive Function In Older Adults (Neuropsychology, November 2014) states that "the nutritional status of older adults relates to their quality of life, ability to live independently, and their risk for developing costly chronic illnesses. An aging adult’s nutritional well-being can be affected by multiple socio-environmental factors, including access to healthy and affordable foods, congregate meal sites, and nutritious selections at restaurants. The Academy of Nutrition and Dietetics, American Society for Nutrition, and the Society for Nutrition Education have identified an older adult's access to a balanced diet to be critical for the prevention of disease and promotion of nutritional wellness so that quality of life and independence can be maintained throughout the aging process and excessive health care costs can be reduced".[3]
By age: younger and older adults
As people age, their bodies change. This can include their taste buds, their needs of certain vitamins and nutrients, and their desire for different types of food. In a study by the Monell Chemical Senses Center,[4] fifty young adults and forty-eight elderly adults participated in the study. "Young" subjects ranged from eighteen to thirty-five years of age and "elderly" subjects were defined as sixty-five years of age or older. There were more females than males in the study, but there were approximately equal proportions of males and females in the two age groups.
The study observed that younger females had stronger cravings for sweets than elderly females. Causation theories included accounting this difference in preference with the younger female test subject's menstrual cycles and the fact that elderly women no longer go through menopause. The study also postulated that "... Ninety-one percent of the cycle-associated cravings were said to occur in the second half of the cycle (between ovulation and the start of menstruation)".[4]
These physical changes can be considered when assessing why someone of an older age might not be getting the nutrition they need. As taste buds change with age, certain foods might not be seen as appetizing. For example, a study done by Dr. Phyllis B. Grzegorcyzk says that as we age, our sense for tasting salty foods goes away slowly. [5] Therefore, when elderly people in care homes eat (often frozen, mass produced) meals that contain large amounts of salt, they may not enjoy it. This could lead to depression, anxiety, or thoughts of suicide.
By biological sex: elderly male and female

Not only are there differences in food preferences between ages, but between biological sexes also. In a study conducted by the ENP, preferences of male and female subjects throughout 13 individual food groups (fresh fruit, chicken, soup, salad, vegetables, potatoes, meat, sandwiches, pasta, canned fruit, legumes, deli meats, and ethnic groups) were identified.
Through this study, it was apparent that older males were "significantly more likely to prefer deli meats, meat, legumes, canned fruit, and ethnic foods compared to females".[2]
Another study by the Monell Chemical Senses Center concluded that females had significantly more cravings for sweets and for chocolate than males; and the study results suggested that males had more cravings or preferences for entrees than sweets.[4]
By personal health
Physical health
With age, some people tend to avoid food or are unwilling to modify their diets due to oral health problems. These issues, such as ill-fitting dentures (false teeth) or gum disease, are associated with significant differences in dietary quality, which is a measure of the quality of the diet using a total of eight recommendations regarding the consumption of foods and nutrients from the National Academy of Sciences (NAS). Approaches to minimize food avoidance and promote changes to the diets of people that have eating difficulties due to oral health conditions are needed desperately because without being able to chew or take in food properly, their health is effected drastically and their food preferences are limited greatly (to soft or liquids only).[6]
Due to varying factors of older adults' physical and mental wellbeing, eating choices can become more and more restricted. Many elderly people are forced into eating softer foods, foods that incorporate fiber and protein, drinking calcium-packed liquids, and so on. Six of the leading causes of death for older adults, including cardiovascular disease, cancer, chronic lower respiratory disease, stroke, Alzheimer's, and diabetes mellitus, have nutrition-related causes and/or respond favorably to nutrition interventions[7]. These six illnesses can implement certain restrictions and heavily influence the diet of elderly persons.
Declines in physical health can also cause deterioration in diet due to difficulties in preparing and eating food as a result of conditions like arthritis.[8]
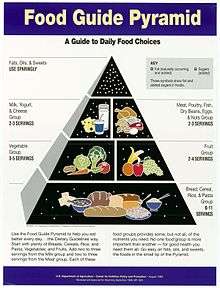
At the 2010 "Providing Healthy and Safe Foods As We Age" conference sponsored by the Institute of Medicine, Dr. Katherine Tucker noted that the elderly are less active and have lower metabolism with a consequent lower need to eat[9]. In addition, they tend to have existing diseases and/or take medications that interfere with nutrient absorption. Based on their research dietary requirements, one study developed a modified food pyramid for adults over 70.[10]
Mental health
The impact of certain diseases can also impact the quality of the food in the elderly population, especially those that are in care facilities. Certain risk factors include conditions that impair cognitive function, such as Dementia. When a person falls victim to a condition that limits mental capacity, mortality risk can rise if due care is not implemented.[11]
As a result of certain mental health conditions and/or diseases—like Alzheimer's—a person's food preferences might become affected. With certain diseases, individuals can develop specific preferences or distaste for various types of food that were not present before onset. For example, people with Alzheimer's may experience many big and small changes as a result of their symptoms.[12] One change identified by Suszynski in "How Dementia Tampers With Taste Buds" is within the taste buds of a patient with dementia, which contain the receptors for taste. Since the experience of flavor is significantly altered, people with dementia can often change their eating habits and take on entirely new food preferences. In this study, the researchers found that these dementia patients had trouble identifying flavors and appeared to have lost the ability to remember tastes, therefore leading to a theory that dementia caused the patients to lose their knowledge of flavors[12].
Psychological conditions can also affect elderly eating habits. For instance, length of widowhood may affect nutrition.[13] Depression in elderly people is also associated with a risk of malnutrition.[14]
By lifestyle choices
Elderly people, as all people, have different lifestyle choices involved in their eating habits. Dietary choices are often a result of personal beliefs and preferences.[8]
A survey based on self-reporting found that many rural community-dwelling elderly Iowans adopted eating habits that provided inadequate levels of some key nutrients and most did not take supplements to correct the deficiencies.[15] In contrast, a restaurant study found that the impact of a lifestyle of health and sustainability on healthy food choices is much stronger for senior diners than for non-senior diners.[16]
Other research has found that adults, regardless of age, will tend to increase fruit and vegetable consumption following a diagnosis of breast, prostate or colorectal cancer.[8]
By social environment and conditioning
The environment can greatly impact food preferences of older adults. Those around 75 years old and older are more likely to suffer with imited mobility due to health conditions[17] and often rely on others for food shopping and preparation.[18]
In some areas, homebound seniors receive one meal per day (several fresh and frozen meals may be included in a single delivery) by communities that offer congregate meals, or meals served in community settings such as senior centers, churches or senior housing communities.[19] These congregate meal programs are encouraged to offer these elderly people a meal at least five times per week.
Impeded access to transportation may also be an issue for elderly persons, especially in rural areas where there is less public transportation. This can vary greatly due to geographic location; for instance, a study based in Iowa study failed to find problems in purchasing food among elderly in rural open country and towns, as those without their own transportation relied on family, friends and senior services.[20] A separate study found a slight difference in urban areas with elderly who did not own a car.[21] Aside from transportation, the kind and quality of available food can also shape food choice if a person lives in a so-called "food desert".
Social network type can also affect individuals food choices in our elderly population. For example, one study showed that a person that has a larger social network and lower economic status is more likely to have proper nutrition that someone who has a smaller social network and higher economic status. [22] Health and social aid can be instrumental into introducing positive change for those at risk.
See also
- Assisted living
- Centenarian
- Elderly care
- Food choice
- Food studies
- Illnesses related to poor nutrition
- List of nutrition guides
- Meals on Wheels
- Nutrition
- Portion size
- Research into centenarians
References
- "Center for Nutrition Policy and Promotion (CNPP) | USDA-FNS" (PDF). Archived from the original (PDF) on August 24, 2014. Retrieved August 14, 2014.
- Song, Hee-Jung; Simon, Judy R.; Patel, Dhruti U (March 21, 2014). "Food Preferences of Older Adults in Senior Nutrition Programs". Journal of Nutrition in Gerontology & Geriatrics. 33 (1): 55–67. doi:10.1080/21551197.2013.875502. PMID 24597997.
- Brewster, Paul W.H.; Melrose, Rebecca J.; Marquine, Maria J.; Johnson, Julene K.; Napoles, Anna; Mac-Kay-Brant, Anna; Farias, Sarah; Reed, Bruce; Mungas, Dan (2014). "Life Experience And Demographic Influences On Cognitive Function In Older Adults". Neuropsychology. 28 (6): 846–858. CiteSeerX 10.1.1.456.6629. doi:10.1037/neu0000098. PMC 4227962. PMID 24933483.
- Pelchat, Marcia Levin (1997). "Food Cravings In Young and Elderly Adults". Appetite. 28 (2): 103–113. doi:10.1006/appe.1996.0063. PMID 9158846.
- Grzegorczyk, P. B.; Jones, S. W.; Mistretta, C. M. (1979-11-01). "Age-Related Differences in Salt Taste Acuity". Journal of Gerontology. 34 (6): 834–840. doi:10.1093/geronj/34.6.834. ISSN 0022-1422. PMID 512303.
- Savoca, MR; Arcury, TA; Leng, X; Chen, H; Bell, RA; Anderson, AM; Kohrman, T; Gilbert, GH; Quandt, SA (2010). "Association Between Dietary Quality of Rural Older Adults and Self-Reported Food Avoidance and Food Modification Due to Oral Health Problems". Journal of the American Geriatrics Society. 58 (7): 1225–1232. doi:10.1111/j.1532-5415.2010.02909.x. PMC 3098620. PMID 20533966.
- Jung, Seung Eun; Lawrence, Jeannine; Hermann, Janice; McMahon, Amy (2020). "Application of the Theory of Planned Behavior to Predict Nutrition Students' Intention to Work with Older Adults". Journal of Nutrition in Gerontology and Geriatrics. 39 (1): 44–55. doi:10.1080/21551197.2019.1664967. PMID 31517572.
- Nicklett, Emily J.; Kadell, Andria R. (2013). "Fruit and vegetable intake among older adults: A scoping review". Maturitas. 75 (4): 305–12. doi:10.1016/j.maturitas.2013.05.005. PMC 3713183. PMID 23769545.
- "Chapter 5: Diet Quality Issues for Aging Populations". Institute of Medicine (US) Food Forum. Providing Healthy and Safe Foods As We Age: Workshop Summary. Washington, D.C.: National Academies Press (US). 2010. ISBN 978-0-309-15883-1.
- Russell, Robert M.; Rasmussen, Helen; Lichtenstein, Alice H. (1999). "Modified Food Guide Pyramid for people over seventy years of age". The Journal of Nutrition. 129 (3): 751–753. doi:10.1093/jn/129.3.751. PMID 10082784.
- Field, Katherine; Duizer, Lisa M. (2016-08-01). "Food Sensory Properties and the Older Adult". Journal of Texture Studies. 47 (4): 266–276. doi:10.1111/jtxs.12197. ISSN 1745-4603.
- Suszynski, Marie. "How Dementia Tampers With Taste Buds". EverydayHealth.com. Retrieved November 4, 2014.
- Quandt, S. A.; McDonald, J; Arcury, T. A.; Bell, R. A.; Vitolins, M. Z. (2000). "Nutritional self-management of elderly widows in rural communities". The Gerontologist. 40 (1): 86–96. doi:10.1093/geront/40.1.86. PMID 10750316.
- Vafaei, Z; Mokhtari, H; Sadooghi, Z; Meamar, R; Chitsaz, A; Moeini, M (2013). "Malnutrition is associated with depression in rural elderly population". Journal of Research in Medical Sciences. 18 (Suppl 1): S15–9. PMC 3743311. PMID 23961277.
- Marshall, T. A.; Stumbo, P. J.; Warren, J. J.; Xie, X. J. (2001). "Inadequate nutrient intakes are common and are associated with low diet variety in rural, community-dwelling elderly". The Journal of Nutrition. 131 (8): 2192–6. doi:10.1093/jn/131.8.2192. PMID 11481416.
- Kim, Myung-Ja; Lee, Choong-Ki; Kim, Woo Gon; Kim, Jong-Man (2013). "Relationships Between Lifestyle Of Health And Sustainability And Healthy Food Choices For Seniors". International Journal of Contemporary Hospitality Management. 25 (4): 558–576. doi:10.1108/09596111311322925.
- "Summary Health Statistics: National Health Interview Survey 2014" (PDF). Center for Disease Control and Prevention. National Center for Health Statistics. 2014. Retrieved Nov 11, 2016.
- Bitto, Ella Annette; Morton, Lois Wright; Oakland, Mary Jan; Sand, Mary (2003). "Grocery Store Access Patterns in Rural Food Deserts". Journal for the Study of Food and Society. 6 (2): 35–48. doi:10.2752/152897903786769616.
- "Congregate Meals". mhcc.maryland.gov/. Maryland Health Care Commission. Retrieved November 6, 2014.
- Bitto, Ella Annette; Morton, Lois Wright; Oakland, Mary Jan; Sand, Mary (2003). "Grocery Store Access Patterns in Rural Food Deserts". Journal for the Study of Food and Society. 6 (2): 35–48. doi:10.2752/152897903786769616.
- Fitzpatrick, Katie; Greenhalgh-Stanley, Nadia; Ver Ploeg, Michele (2016). "The Impact of Food Deserts on Food Insufficiency and SNAP Participation among the Elderly". American Journal of Agricultural Economics. 98: 19–40. doi:10.1093/ajae/aav044.
- Kim, Chang-O (2016). "Food choice patterns among frail older adults: The associations between social network, food choice values, and diet quality". Appetite. 96: 116–121. doi:10.1016/j.appet.2015.09.015. PMID 26385288.