Do not resuscitate
A do-not-resuscitate order (DNR), also known as no code or allow natural death, is a legal order, written or oral depending on country, indicating that a person does not want to receive cardiopulmonary resuscitation (CPR) if that person's heart stops beating.[1] Sometimes it also prevents other medical interventions.[2] The legal status and processes surrounding DNR orders vary from country to country. Most commonly, the order is placed by a physician based on a combination of medical judgement and patient wishes and values.[3]
| Do not resuscitate | |
|---|---|
 DNR form used in Virginia | |
| Other names | Do not attempt resuscitation, allow natural death, no code |
Basis for choice
Interviews with 26 DNR patients and 16 full code patients in Toronto in 2006-9 suggest that the decision to choose do-not-resuscitate status was based on personal factors including health and lifestyle; relational factors (to family or to society as a whole); and philosophical factors.[4] Audio recordings of 19 discussions about DNR status between doctors and patients in 2 US hospitals (San Francisco and Durham) in 2008-9 found that patients "mentioned risks, benefits, and outcomes of CPR," and doctors "explored preferences for short- versus long-term use of life-sustaining therapy."[5]
Outcomes of CPR
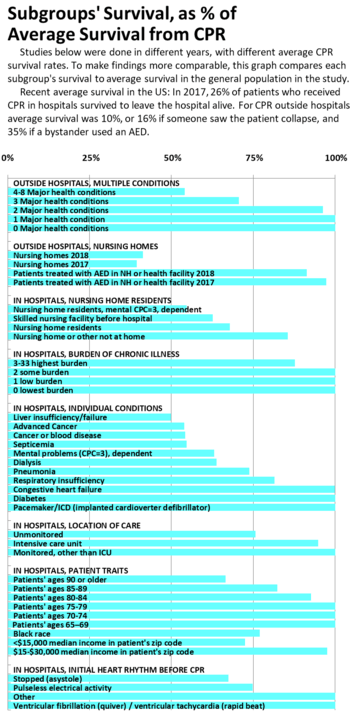
When medical institutions explain DNR, they describe survival from CPR, in order to address patients' concerns about outcomes. After CPR in hospitals in 2017, 7,000 patients survived to leave the hospital alive, out of 26,000 CPR attempts, or 26%.[6] After CPR outside hospitals in 2018, 8,000 patients survived to leave the hospital alive, out of 80,000 CPR attempts, or 10%. Success was 21% in a public setting, where someone was more likely to see the person collapse and give help than in a home.[7] Success was 35% when bystanders used an Automated external defibrillator (AED), outside health facilities and nursing homes.[7]
In information on DNR, medical institutions compare survival for patients with multiple chronic illnesses;[8][9] patients with heart, lung or kidney disease;[8][9] liver disease;[8] widespread cancer[8][9][10] or infection;[10] and residents of nursing homes.[8] Research shows that CPR survival is the same as the average CPR survival rate, or nearly so, for patients with multiple chronic illnesses,[11][12] or diabetes, heart or lung diseases.[13] Survival is about half as good as the average rate, for patients with kidney or liver disease,[13] or widespread cancer[13][14] or infection.[13]
For people who live in nursing homes, survival after CPR is about half to three quarters of the average rate.[7][11][13][15][16] In health facilities and nursing homes where AEDs are available and used, survival rates are twice as high as the average survival found in nursing homes overall.[7] Few nursing homes have AEDs.[17]
Research on 26,000 patients found similarities in the health situations of patients with and without DNRs. For each of 10 levels of illness, from healthiest to sickest, 7% to 36% of patients had DNR orders; the rest had full code.[18]
Risks
As noted above, patients considering DNR mention the risks of CPR. Physical injuries, such as broken bones, affect 13% of CPR patients,[19] and an unknown additional number have broken cartilage which can sound like breaking bones.[20][21]
Mental problems affect some patients, both before and after CPR. After CPR, up to 1 more person, among each 100 survivors, is in a coma than before CPR (and most people come out of comas[22][23]). 5 to 10 more people, of each 100 survivors, need more help with daily life than they did before CPR. 5 to 21 more people, of each 100 survivors, decline mentally, but stay independent.[24]
Organ donation
Organ donation is possible after CPR, but not usually after a death with a DNR. If CPR does not revive the patient, and continues until an operating room is available, kidneys and liver can be considered for donation. US Guidelines endorse organ donation, "Patients who do not have ROSC [return of spontaneous circulation] after resuscitation efforts and who would otherwise have termination of efforts may be considered candidates for kidney or liver donation in settings where programs exist."[25] European guidelines encourage donation, "After stopping CPR, the possibility of ongoing support of the circulation and transport to a dedicated centre in perspective of organ donation should be considered."[26] CPR revives 64% of patients in hospitals[27] and 43% outside[7] (ROSC), which gives families a chance to say goodbye,[28] and all organs can be considered for donation, "We recommend that all patients who are resuscitated from cardiac arrest but who subsequently progress to death or brain death be evaluated for organ donation."[25]
1,000 organs per year in the US are transplanted from patients who had CPR.[29] Donations can be taken from 40% of patients who have ROSC and later become brain dead,[30] and an average of 3 organs are taken from each patient who donates organs.[29] DNR does not usually allow organ donation.
Less care for DNR patients
Reductions in other care are not supposed to result from DNR,[1] but they do. Some patients choose DNR because they prefer less care: Half of Oregon patients with DNR orders who filled out a POLST {known as a POST (Physician Orders and Scope of Treatment) in Tennessee} wanted only comfort care, and 7% wanted full care. The rest wanted various limits on care, so blanket assumptions are not reliable.[31] There are many doctors "misinterpreting DNR preferences and thus not providing other appropriate therapeutic interventions."[18]
Patients with DNR are less likely to get medically appropriate care for a wide range of issues such as blood transfusions, cardiac catheterizations, cardiac bypass, operations for surgical complication,[32] blood cultures, central line placement,[33] antibiotics and diagnostic tests.[34] "[P]roviders intentionally apply DNR orders broadly because they either assume that patients with DNR orders would also prefer to abstain from other life-sustaining treatments or believe that other treatments would not be medically beneficial."[34] 60% of surgeons do not offer operations with over 1% mortality to patients with DNRs.[35]
Patients with DNR therefore die sooner, even from causes unrelated to CPR. A study grouped 26,300 very sick hospital patients in 2006-10 from the sickest to the healthiest, using a detailed scale from 0 to 44. They compared survival for patients at the same level, with and without DNR orders. In the healthiest group, 69% of those without DNR survived to leave the hospital, while only 7% of equally healthy patients with DNR survived. In the next-healthiest group, 53% of those without DNR survived, and 6% of those with DNR. Among the sickest patients, 6% of those without DNR survived, and none with DNR.[18]
Two Dartmouth doctors note that "In the 1990s...'resuscitation' increasingly began to appear in the medical literature to describe strategies to treat people with reversible conditions, such as IV fluids for shock from bleeding or infection... the meaning of DNR became ever more confusing to health-care providers."[36] Other researchers confirm this pattern, using "resuscitative efforts" to cover a range of care, from treatment of allergic reaction to surgery for a broken hip.[37] Hospital doctors do not agree which treatments to withhold from DNR patients, and document decisions in the chart only half the time.[33] A survey with several scenarios found doctors "agreed or strongly agreed to initiate fewer interventions when a DNR order was present.[33]
After successful CPR, hospitals often discuss putting the patient on DNR, to avoid another resuscitation. Guidelines generally call for a 72-hour wait to see what the prognosis is,[38] but within 12 hours US hospitals put up to 58% of survivors on DNR, and at the median hospital 23% received DNR orders at this early stage, much earlier than the guideline. The hospitals putting fewest patients on DNR had more successful survival rates, which the researchers suggest shows their better care in general.[18] When CPR happened outside the hospital, hospitals put up to 80% of survivors on DNR within 24 hours, with an average of 32.5%. The patients who received DNR orders had less treatment, and almost all died in the hospital. The researchers say families need to expect death if they agree to DNR in the hospital.[2]
Patients' values
The philosophical factors and preferences mentioned by patients and doctors are treated in the medical literature as strong guidelines for care, including DNR or CPR. "Complex medical aspects of a patient with a critical illness must be integrated with considerations of the patient’s values and preferences"[39] and "the preeminent place of patient values in determining the benefit or burden imposed by medical interventions."[40] Patients' most common goals include talking, touch, prayer, helping others, addressing fears, laughing.[41][42] Being mentally aware was as important to patients as avoiding pain, and doctors underestimated its importance and overestimated the importance of pain.[41] Dying at home was less important to most patients.[41] Three quarters of patients prefer longer survival over better health.[43]
Advance directive, living will, POLST, medical jewelry, tattoos
Advance directives and living wills are documents written by individuals themselves, so as to state their wishes for care, if they are no longer able to speak for themselves. In contrast, it is a physician or hospital staff member who writes a DNR "physician's order," based upon the wishes previously expressed by the individual in his or her advance directive or living will. Similarly, at a time when the individual is unable to express his wishes, but has previously used an advance directive to appoint an agent, then a physician can write such a DNR "physician's order" at the request of that individual's agent. These various situations are clearly enumerated in the "sample" DNR order presented on this page.
It should be stressed that, in the United States, an advance directive or living will is not sufficient to ensure a patient is treated under the DNR protocol, even if it is their wish, as neither an advance directive nor a living will legally binds doctors.[44] They can be legally binding in appointing a medical representative, but not in treatment decisions.
Physician Orders for Life-Sustaining Treatment (POLST) documents are the usual place where a DNR is recorded outside hospitals. A disability rights group criticizes the process, saying doctors are trained to offer very limited scenarios with no alternative treatments, and steer patients toward DNR. They also criticize that DNR orders are absolute, without variations for context.[45] The Mayo Clinic found in 2013 that "Most patients with DNR/DNI [do not intubate] orders want CPR and/or intubation in hypothetical clinical scenarios," so the patients had not had enough explanation of the DNR/DNI or did not understand the explanation.[46]
Medical jewelry
Medical bracelets, medallions, and wallet cards from approved providers allow for identification of DNR patients outside in home or non-hospital settings. Each state has its own DNR policies, procedures, and accompanying paperwork for emergency medical service personnel to comply with such forms of DNR.[47]
DNR tattoos
There is a growing trend of using DNR tattoos, commonly placed on the chest, to replace other forms of DNR, but these often cause confusion and ethical dilemmas among healthcare providers.[48] Laws vary from state to state regarding what constitutes a valid DNR and currently do not include tattoos.[47] End of life (EOL) care preferences are dynamic and depend on factors such as health status, age, prognosis, healthcare access, and medical advancements. DNR orders can be rescinded while tattoos are far more difficult to remove if the individual changes their mind. Uncommonly, some individuals have decided to get their DNR tattoo based on a dare while under the influence.[49]
Ethics
DNR orders in certain situations have been subject to ethical debate. In many institutions it is customary for a patient going to surgery to have their DNR automatically rescinded. Though the rationale for this may be valid, as outcomes from CPR in the operating room are substantially better than general survival outcomes after CPR, the impact on patient autonomy has been debated. It is suggested that facilities engage patients or their decision makers in a 'reconsideration of DNR orders' instead of automatically making a forced decision.[50]
When a patient or family and doctors do not agree on a DNR status, it is common to ask the hospital ethics committee for help, but authors have pointed out that many members have little or no ethics training, some have little medical training, and they do have conflicts of interest by having the same employer and budget as the doctors.[51][52][53]
There is accumulating evidence of racial differences in rates of DNR adoption. A 2014 study of end stage cancer patients found that non-Latino white patients were significantly more likely to have a DNR order (45%) than black (25%) and Latino (20%) patients. The correlation between preferences against life-prolonging care and the increased likelihood of advance care planning is consistent across ethnic groups.[54]
Ethical dilemmas occur when a patient with a DNR attempts suicide and the necessary treatment involves ventilation or CPR. In these cases it has been argued that the principle of beneficence takes precedence over patient autonomy and the DNR can be revoked by the physician.[55] Another dilemma occurs when a medical error happens to a patient with a DNR. If the error is reversible only with CPR or ventilation there is no consensus if resuscitation should take place or not.[56]
There are also ethical concerns around how patients reach the decision to agree to a DNR order. One study found that patients wanted intubation in several scenarios, even when they had a Do Not Intubate (DNI) order, which raises a question whether patients with DNR orders may want CPR in some scenarios too.[57][46][58] It is possible that providers are having a "leading conversation" with patients or mistakenly leaving crucial information out when discussing DNR.[57][45]
One study reported that while 88% of young doctor trainees at two hospitals in California in 2013 believed they themselves would ask for a DNR order if they were terminally ill, they are flexible enough to give high intensity care to patients who have not chosen DNR.[59][60]
There is also the ethical issue of discontinuation of an implantable cardioverter defibrillator (ICD) in DNR patients in cases of medical futility. A large survey of Electrophysiology practitioners, the heart specialists who implant pacemakers and ICDs, noted that the practitioners felt that deactivating an ICD was not ethically distinct from withholding CPR thus consistent with DNR. Most felt that deactivating a pacemaker was a separate issue and could not be broadly ethically endorsed. Pacemakers were felt to be unique devices, or ethically taking a role of "keeping a patient alive" like dialysis.[61]
Terminology
DNR and Do Not Resuscitate are common terms in the United States, Canada, New Zealand and the United Kingdom. This may be expanded in some regions with the addition of DNI (Do Not Intubate). In some hospitals DNR alone will imply no intubation,[62] though 98% of intubations are unrelated to cardiac arrest; most intubations are for pneumonia or surgery.[63] Clinically, the vast majority of people requiring resuscitation will require intubation, making a DNI alone problematic. Hospitals sometimes use the expression no code, which refers to the jargon term code, short for Code Blue, an alert to a hospital's resuscitation team.
Some areas of the United States and the United Kingdom include the letter A, as in DNAR, to clarify "Do Not Attempt Resuscitation". This alteration is so that it is not presumed by the patient or family that an attempt at resuscitation will be successful.
As noted above in Less care for DNR patients, the word "resuscitation" has grown to include many treatments other than CPR, so DNR has become ambiguous, and authors recommend "No CPR" instead.[36]
Since the term DNR implies the omission of action, and therefore "giving up", a few authors have advocated for these orders to be retermed Allow Natural Death.[64][65] Others say AND is ambiguous whether it would allow morphine, antibiotics, hydration or other treatments as part of a natural death.[66][67] New Zealand and Australia, and some hospitals in the UK, use the term NFR or Not For Resuscitation. Typically these abbreviations are not punctuated, e.g., DNR rather than D.N.R.
Resuscitation orders, or lack thereof, can also be referred to in the United States as a part of Physician Orders for Life-Sustaining Treatment (POLST), Medical Orders for Life-Sustaining Treatment (MOLST), Physician's Orders on Scope of Treatment (POST) or Transportable Physician Orders for Patient Preferences (TPOPP) orders,[68] typically created with input from next of kin when the patient or client is not able to communicate their wishes.
Another synonymous term is "not to be resuscitated" (NTBR).[69]
Until recently in the UK it was common to write "Not for 222" or conversationally, "Not for twos". This was implicitly a hospital DNR order, where 222 (or similar) is the hospital telephone number for the emergency resuscitation or crash team.
Usage by country
DNR documents are widespread in some countries and unavailable in others. In countries where a DNR is unavailable the decision to end resuscitation is made solely by physicians.
A 2016 paper reports a survey of doctors in numerous countries, asking "how often do you discuss decisions about resuscitation with patients and/or their family?" and "How do you communicate these decisions to other doctors in your institution?"[70] Some countries had multiple respondents, who did not always act the same, as shown below. There was also a question "Does national guidance exist for making resuscitation decisions in your country?" but the concept of "guidance" had no consistent definition, For example, in the US, four respondents said Yes, and two said No.
| Country | Discuss with Patient or Family | Tell Other Doctors the Decision |
|---|---|---|
| Argentina | Rarely | Oral |
| Australia | Most, Half | Oral+Notes+Pre-printed (2), Notes |
| Austria | Half | Notes |
| Barbados | Half | Oral+Notes |
| Belgium | Half, Rarely | Notes+Electronic |
| Brazil | Most | Oral+Notes |
| Brunei | Rarely | Oral+Notes |
| Canada | Always, Most | Oral+Notes, Oral+Notes+Electronic, Notes+Pre-printed |
| Colombia | Half | Oral |
| Cuba | Always | Oral |
| Denmark | Most | Electronic |
| France | Most | Pre-printed, |
| Germany | Always | Oral+Notes+Electronic |
| Hong Kong | Always, Half | Notes+Pre-printed, Oral+Notes+Pre-printed |
| Hungary | Rarely | Oral |
| Iceland | Rarely | Notes+Electronic |
| India | Always | Notes, Oral, Oral+Notes |
| Ireland | Most, Rarely | Notes (2) |
| Israel | Most, Half | Oral+Notes (2) Notes |
| Japan | Most, Half | Oral, Notes, |
| Lebanon | Most | Oral+Notes+Electronic |
| Malaysia | Rarely | Notes |
| Malta | Most | Notes |
| New Zealand | Always | Pre-printed |
| Netherlands | Half | Electronic (3) |
| Norway | Always, Rarely | Oral, Notes+Electronic |
| Pakistan | Always | Notes+Electronic |
| Poland | Always, Most | Oral+Notes, Notes+Pre-printed |
| Puerto Rico | Always | Pre-printed |
| Saudi Arabia | Always, Most | Pre-printed, Notes+Electronic, Oral |
| Singapore | Always, Most, Half | Pre-printed (2), Oral+Notes+Pre-printed, Oral+Notes+Electronic, Oral+Pre-printed |
| South Africa | Rarely | Oral+Notes |
| South Korea | Always | Pre-printed |
| Spain | Always, Most | Pre-printed, Oral+Notes+Electronic, Oral+Notes+Pre-printed |
| Sri Lanka | Most | Notes |
| Sweden | Most | Oral+Notes+Pre-printed+Electronic |
| Switzerland | Most, Half | Oral+Notes+Pre-printed, Oral+Notes+Other |
| Taiwan | Half, Rarely | Notes+Pre-printed+Other, Oral |
| UAE | Half | Oral+Notes |
| Uganda | Always | Notes, |
| USA | Always, Most | Notes, Electronic, Oral+Electronic, Oral+Notes+Electronic, Oral+Notes+Pre-printed+Electronic |
Middle East
DNRs are not recognized by Jordan. Physicians attempt to resuscitate all patients regardless of individual or familial wishes.[71] The UAE have laws forcing healthcare staff to resuscitate a patient even if the patient has a DNR or does not wish to live. There are penalties for breaching the laws.[72] In Saudi Arabia patients cannot legally sign a DNR, but a DNR can be accepted by order of the primary physician in case of terminally ill patients. In Israel, it is possible to sign a DNR form as long as the patient is dying and aware of their actions.
United Kingdom
England and Wales
In England and Wales, CPR is presumed in the event of a cardiac arrest unless a do not resuscitate order is in place. If they have capacity as defined under the Mental Capacity Act 2005 the patient may decline resuscitation, however any discussion is not in reference to consent to resuscitation and instead should be an explanation.[73] Patients may also specify their wishes and/or devolve their decision-making to a proxy using an advance directive, which are commonly referred to as 'Living Wills'. Patients and relatives cannot demand treatment (including CPR) which the doctor believes is futile and in this situation, it is their doctor's duty to act in their 'best interest', whether that means continuing or discontinuing treatment, using their clinical judgment. If the patient lacks capacity, relatives will often be asked for their opinion out of respect.
Scotland
In Scotland, the terminology used is "Do Not Attempt Cardiopulmonary Resuscitation" or "DNACPR". There is a single policy used across all of NHS Scotland. The legal standing is similar to that in England and Wales, in that CPR is viewed as a treatment and, although there is a general presumption that CPR will be performed in the case of cardiac arrest, this is not the case if it is viewed by the treating clinician to be futile. Patients and families cannot demand CPR to be performed if it is felt to be futile (as with any medical treatment) and a DNACPR can be issued despite disagreement, although it is good practice to involve all parties in the discussion.[74]
United States
In the United States the documentation is especially complicated in that each state accepts different forms, and advance directives and living wills may not be accepted by EMS as legally valid forms. If a patient has a living will that specifies the patient requests DNR but does not have a properly filled out state-sponsored form that is co-signed by a physician, EMS may attempt resuscitation.
The DNR decision by patients was first litigated in 1976 in In re Quinlan. The New Jersey Supreme Court upheld the right of Karen Ann Quinlan's parents to order her removal from artificial ventilation. In 1991 Congress passed into law the Patient Self-Determination Act that mandated hospitals honor an individual's decision in their healthcare.[75] Forty-nine states currently permit the next of kin to make medical decisions of incapacitated relatives, the exception being Missouri. Missouri has a Living Will Statute that requires two witnesses to any signed advance directive that results in a DNR/DNI code status in the hospital.
In the United States, cardiopulmonary resuscitation (CPR) and advanced cardiac life support (ACLS) will not be performed if a valid written DNR order is present. Many states do not recognize living wills or health care proxies in the prehospital setting and prehospital personnel in those areas may be required to initiate resuscitation measures unless a specific state-sponsored form is properly filled out and cosigned by a physician.[76][77]
Canada
Do not resuscitate orders are similar to those used in the United States. In 1995, the Canadian Medical Association, Canadian Hospital Association, Canadian Nursing Association, and Catholic Health Association of Canada worked with the Canadian Bar Association to clarify and create a Joint Statement on Resuscitative Interventions guideline for use to determine when and how DNR orders are assigned.[78] DNR orders must be discussed by doctors with the patient or patient agents or patient's significant others. Unilateral DNR by medical professionals can only be used if the patient is in a vegetative state.[78]
Australia
In Australia, Do Not Resuscitate orders are covered by legislation on a state-by-state basis.
In Victoria, a Refusal of Medical Treatment certificate is a legal means to refuse medical treatments of current medical conditions. It does not apply to palliative care (reasonable pain relief; food and drink). An Advanced Care Directive legally defines the medical treatments that a person may choose to receive (or not to receive) in various defined circumstances. It can be used to refuse resuscitation, so as avoid needless suffering.[79]
In NSW, a Resuscitation Plan is a medically authorised order to use or withhold resuscitation measures, and which documents other aspects of treatment relevant at end of life. Such plans are only valid for patients of a doctor who is a NSW Health staff member. The plan allows for the refusal of any and all life-sustaining treatments, the advance refusal for a time of future incapacity, and the decision to move to purely palliative care.[80]
Italy
DNRs are not recognized by Italy. Physicians must attempt to resuscitate all patients regardless of individual or familial wishes. Italian laws force healthcare staff to resuscitate a patient even if the patient has a DNR or does not wish to live. There are jail penalties (from 6 to 15 years) for healthcare staff breaching this law, e.g. "omicidio del consenziente".[81] Therefore, in Italy a signed DNR has no legal value.[82]
Taiwan
In Taiwan, patients sign their own DNR orders, and are required to do so to receive hospice care.[83] However, one study looking at insights into Chinese perspectives on DNR showed that the majority of DNR orders in Taiwan were signed by surrogates.[84] Typically doctors discuss the issue of DNR with the patients family rather than the patient themselves.[85] In Taiwan, there are two separate types of DNR forms: DNR-P which the patient themselves sign and DNR-S in which a designated surrogate can sign. Typically, the time period between signing the DNR and death is very short, showing that signing a DNR in Taiwan is typically delayed. Two witnesses must also be present in order for a DNR to be signed.[85]
DNR orders have been legal in Taiwan since May 2000 and were enacted by the Hospice and Palliative Regulation. Also included in the Hospice and Palliative Regulation is the requirement to inform a patient of their terminal condition, however, the requirement is not explicitly defined leading to interpretation of exact truth telling.[85]
Japan
In Japan, DNR orders are known as Do Not Attempt Resuscitation (DNAR). Currently, there are no laws or guidelines in place regarding DNAR orders but they are still routinely used.[86] A request to withdraw from life support can be completed by the patient or a surrogate.[82] In addition, it is common for Japanese doctors and nurses to be involved in the decision making process for the DNAR form.[87]
France
In 2005, France implemented its "Patients' Rights and End of Life Care" act. This act allows the withholding/withdrawal of life support treatment and as well as the intensified usage of certain medications that can quicken the action of death. This act also specifies the requirements of the act.[88]
The "Patients' Rights and End of Life Care" Act includes three main measures. First, it prohibits the continuation of futile medical treatments. Secondly, it empowers the right to palliative care that may also include the intensification of the doses of certain medications that can result in the shortening the patient's life span. Lastly, it strengthens the principle of patient autonomy. If the patient is unable to make a decision, the discussion, thus, goes to a trusted third party.[89]
See also
- Advance Health Care Directive
- Cardiac arrest
- Power of attorney
- Letting die
- Passive euthanasia
- Uniform Rights of the Terminally Ill Act
- Patient Self-Determination Act
- Slow code
- Medical ethics
- Right to die
References
- "Do-not-resuscitate order: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2019-05-29.
- Richardson DK, Zive D, Daya M, Newgard CD (April 2013). "The impact of early do not resuscitate (DNR) orders on patient care and outcomes following resuscitation from out of hospital cardiac arrest". Resuscitation. 84 (4): 483–7. doi:10.1016/j.resuscitation.2012.08.327. PMID 22940596.
- Santonocito C, Ristagno G, Gullo A, Weil MH (February 2013). "Do-not-resuscitate order: a view throughout the world". Journal of Critical Care. 28 (1): 14–21. doi:10.1016/j.jcrc.2012.07.005. PMID 22981534.
- Downar J, Luk T, Sibbald RW, Santini T, Mikhael J, Berman H, Hawryluck L (June 2011). "Why do patients agree to a "Do not resuscitate" or "Full code" order? Perspectives of medical inpatients". Journal of General Internal Medicine. 26 (6): 582–7. doi:10.1007/s11606-010-1616-2. PMC 3101966. PMID 21222172.
- Anderson WG, Chase R, Pantilat SZ, Tulsky JA, Auerbach AD (April 2011). "Code status discussions between attending hospitalist physicians and medical patients at hospital admission". Journal of General Internal Medicine. 26 (4): 359–66. doi:10.1007/s11606-010-1568-6. PMC 3055965. PMID 21104036.
- Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. (March 2019). "Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association". Circulation. 139 (10): e56–e528. doi:10.1161/cir.0000000000000659. PMID 30700139.
- "National Reports by Year". MyCares.net. Retrieved 2018-12-12.
- COALITION for COMPASSIONATE CARE of CALIFORNIA (2010). "CPR/DNR" (PDF). UCLA. Retrieved 2019-05-03.
- WV Center for End of Life Care; WV Department of Health and Human Services (2016). "DNR Card (Do Not Resuscitate)" (PDF). Retrieved 2019-05-03.
- "Understanding Do Not Resuscitate (DNR) Orders - Brigham and Women's Faulkner Hospital". www.brighamandwomensfaulkner.org. Retrieved 2019-05-03.
- Ehlenbach WJ, Barnato AE, Curtis JR, Kreuter W, Koepsell TD, Deyo RA, Stapleton RD (July 2009). "Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly". The New England Journal of Medicine. 361 (1): 22–31. doi:10.1056/NEJMoa0810245. PMC 2917337. PMID 19571280.
- Carew HT, Zhang W, Rea TD (June 2007). "Chronic health conditions and survival after out-of-hospital ventricular fibrillation cardiac arrest". Heart. 93 (6): 728–31. doi:10.1136/hrt.2006.103895. PMC 1955210. PMID 17309904.
- Merchant RM, Berg RA, Yang L, Becker LB, Groeneveld PW, Chan PS (January 2014). "Hospital variation in survival after in-hospital cardiac arrest". Journal of the American Heart Association. 3 (1): e000400. doi:10.1161/JAHA.113.000400. PMC 3959682. PMID 24487717.
- Bruckel JT, Wong SL, Chan PS, Bradley SM, Nallamothu BK (October 2017). "Patterns of Resuscitation Care and Survival After In-Hospital Cardiac Arrest in Patients With Advanced Cancer". Journal of Oncology Practice. 13 (10): e821–e830. doi:10.1200/JOP.2016.020404. PMC 5640412. PMID 28763260.
- Abbo ED, Yuen TC, Buhrmester L, Geocadin R, Volandes AE, Siddique J, Edelson DP (January 2013). "Cardiopulmonary resuscitation outcomes in hospitalized community-dwelling individuals and nursing home residents based on activities of daily living". Journal of the American Geriatrics Society. 61 (1): 34–9. doi:10.1111/jgs.12068. PMID 23311551.
- Søholm H, Bro-Jeppesen J, Lippert FK, Køber L, Wanscher M, Kjaergaard J, Hassager C (March 2014). "Resuscitation of patients suffering from sudden cardiac arrests in nursing homes is not futile". Resuscitation. 85 (3): 369–75. doi:10.1016/j.resuscitation.2013.10.033. PMID 24269866.
- Ullman, Edward A.; Sylvia, Brett; McGhee, Jonathan; Anzalone, Brendan; Fisher, Jonathan (2007-07-01). "Lack of Early Defibrillation Capability and Automated External Defibrillators in Nursing Homes". Journal of the American Medical Directors Association. Berlin/Heidelberg: Springer-Verlag. 8 (6): 413–415. doi:10.1016/j.jamda.2007.04.001. ISSN 1525-8610. PMID 17619041.
- Fendler TJ, Spertus JA, Kennedy KF, Chen LM, Perman SM, Chan PS (2015-09-22). "Alignment of Do-Not-Resuscitate Status With Patients' Likelihood of Favorable Neurological Survival After In-Hospital Cardiac Arrest". JAMA. 314 (12): 1264–71. doi:10.1001/jama.2015.11069. PMC 4701196. PMID 26393849.
- Boland LL, Satterlee PA, Hokanson JS, Strauss CE, Yost D (January–March 2015). "Chest Compression Injuries Detected via Routine Post-arrest Care in Patients Who Survive to Admission after Out-of-hospital Cardiac Arrest". Prehospital Emergency Care. 19 (1): 23–30. doi:10.3109/10903127.2014.936636. PMID 25076024.
- "CPR Review - Keeping It Real". HEARTSAVER (BLS Training Site) CPR/AED & First Aid (Bellevue, NE). Retrieved 2018-12-12.
- "CPR Breaking Bones". EMTLIFE. Retrieved 2018-12-12.
- Katz, Douglas I.; Polyak, Meg; Coughlan, Daniel; Nichols, Meliné; Roche, Alexis (2009-01-01). Laureys, Steven; Schiff, Nicholas D.; Owen, Adrian M. (eds.). "Natural history of recovery from brain injury after prolonged disorders of consciousness: outcome of patients admitted to inpatient rehabilitation with 1–4 year follow-up". Coma Science: Clinical and Ethical Implications. 177. Elsevier: 73–88. Cite journal requires
|journal=(help) - Giacino, Joseph T.; Katz, Douglas I.; Schiff, Nicholas D.; Whyte, John; Ashman, Eric J.; Ashwal, Stephen; Barbano, Richard; Hammond, Flora M.; Laureys, Steven (2018-08-08). "Practice guideline update recommendations summary: Disorders of consciousness". Neurology. 91 (10): 450–460. doi:10.1212/WNL.0000000000005926. ISSN 0028-3878. PMC 6139814. PMID 30089618.
- The ranges given in the text above represent outcomes inside and outside of hospitals:
- In US hospitals a study of 12,500 survivors after CPR, 2000-2009, found: 1% more survivors of CPR were in comas than before CPR (3% before, 4% after), 5% more survivors were dependent on other people, and 5% more had moderate mental problems but were still independent. [Chan PS, Spertus JA, Krumholz HM, Berg RA, Li Y, Sasson C, Nallamothu BK (June 2012). "Supplement of A validated prediction tool for initial survivors of in-hospital cardiac arrest". Archives of Internal Medicine. 172 (12): 947–53. doi:10.1001/archinternmed.2012.2050. PMC 3517176. PMID 22641228.]
- Outside hospitals, half a percent more survivors were in comas after CPR (0.5% before, 1% after), 10% more survivors were dependent on other people because of mental problems, and 21% more had moderate mental problems which still let them stay independent. This study covered 419 survivors of CPR in Copenhagen in 2007-2011. [Søholm op.cit]
- "Part 8: Post-Cardiac Arrest Care – ECC Guidelines, section 11". Resuscitation Science, Section 11. 2015.
- Bossaert; et al. (2015). "European Resuscitation Council Guidelines for Resuscitation 2015: Section 11. The ethics of resuscitation and end-of-life decisions". Resuscitation. 95: 302–11. doi:10.1016/j.resuscitation.2015.07.033. PMID 26477419. Retrieved 2019-01-24.
- Joseph L, Chan PS, Bradley SM, Zhou Y, Graham G, Jones PG, Vaughan-Sarrazin M, Girotra S (September 2017). "Temporal Changes in the Racial Gap in Survival After In-Hospital Cardiac Arrest". JAMA Cardiology. 2 (9): 976–984. doi:10.1001/jamacardio.2017.2403. PMC 5710174. PMID 28793138.
- Breu AC (October 2018). "Clinician-Patient Discussions of Successful CPR-The Vegetable Clause". JAMA Internal Medicine. 178 (10): 1299–1300. doi:10.1001/jamainternmed.2018.4066. PMID 30128558.
- Orioles A, Morrison WE, Rossano JW, Shore PM, Hasz RD, Martiner AC, Berg RA, Nadkarni VM (December 2013). "An under-recognized benefit of cardiopulmonary resuscitation: organ transplantation". Critical Care Medicine. 41 (12): 2794–9. doi:10.1097/CCM.0b013e31829a7202. PMID 23949474.
- Sandroni C, D'Arrigo S, Callaway CW, Cariou A, Dragancea I, Taccone FS, Antonelli M (November 2016). "The rate of brain death and organ donation in patients resuscitated from cardiac arrest: a systematic review and meta-analysis". Intensive Care Medicine. 42 (11): 1661–1671. doi:10.1007/s00134-016-4549-3. PMC 5069310. PMID 27699457.
- Tolle, Susan W.; Olszewski, Elizabeth; Schmidt, Terri A.; Zive, Dana; Fromme, Erik K. (2012-01-04). "POLST Registry Do-Not-Resuscitate Orders and Other Patient Treatment Preferences". JAMA. 307 (1): 34–35. doi:10.1001/jama.2011.1956. ISSN 0098-7484. PMID 22215159.
- Horwitz LI (January 2016). "Implications of Including Do-Not-Resuscitate Status in Hospital Mortality Measures". JAMA Internal Medicine. 176 (1): 105–6. doi:10.1001/jamainternmed.2015.6845. PMID 26662729.
- Smith CB, Bunch O'Neill L (October 2008). "Do not resuscitate does not mean do not treat: how palliative care and other modalities can help facilitate communication about goals of care in advanced illness". The Mount Sinai Journal of Medicine, New York. 75 (5): 460–5. doi:10.1002/msj.20076. PMID 18828169.
- Yuen JK, Reid MC, Fetters MD (July 2011). "Hospital do-not-resuscitate orders: why they have failed and how to fix them". Journal of General Internal Medicine. 26 (7): 791–7. doi:10.1007/s11606-011-1632-x. PMC 3138592. PMID 21286839.
- Schwarze ML, Redmann AJ, Alexander GC, Brasel KJ (January 2013). "Surgeons expect patients to buy-in to postoperative life support preoperatively: results of a national survey". Critical Care Medicine. 41 (1): 1–8. doi:10.1097/CCM.0b013e31826a4650. PMC 3624612. PMID 23222269.
- Malhi S (2019-05-05). "The term 'do not resuscitate' should be laid to rest". Retrieved 2019-05-29.
- Marco CA, Mozeleski E, Mann D, Holbrook MB, Serpico MR, Holyoke A, Ginting K, Ahmed A (March 2018). "Advance directives in emergency medicine: Patient perspectives and application to clinical scenarios". The American Journal of Emergency Medicine. 36 (3): 516–518. doi:10.1016/j.ajem.2017.08.002. PMID 28784259.
- "Resuscitation, Item 7.1, Prognostication". CPR & ECC Guidelines. The American Heart Association.
Part 3: Ethical Issues – ECC Guidelines, Timing of Prognostication in Post–Cardiac Arrest Adults
- Burns JP, Truog RD (December 2007). "Futility: a concept in evolution". Chest. 132 (6): 1987–93. doi:10.1378/chest.07-1441. PMID 18079232.
- Armstrong (2014). "MEDICAL FUTILITY AND NONBENEFICIAL INTERVENTIONS: AN ALGORITHM TO AID CLINICIANS". Mayo Clinic Proceedings. 89 (12): 1599–607. doi:10.1016/j.mayocp.2014.08.017. PMID 25441398.
- Steinhauser (2000). "FACTORS CONSIDERED IMPORTANT AT THE END OF LIFE BY PATIENTS, FAMILY, PHYSICIANS, AND OTHER CARE PROVIDERS" (PDF). JAMA. 284 (19): 2476–82. doi:10.1001/jama.284.19.2476. PMID 11074777.
- Reinke LF, Uman J, Udris EM, Moss BR, Au DH (December 2013). "Preferences for death and dying among veterans with chronic obstructive pulmonary disease". The American Journal of Hospice & Palliative Care. 30 (8): 768–72. doi:10.1177/1049909112471579. PMID 23298873.
- Brunner-La Rocca HP, Rickenbacher P, Muzzarelli S, Schindler R, Maeder MT, Jeker U, et al. (March 2012). "End-of-life preferences of elderly patients with chronic heart failure". European Heart Journal. 33 (6): 752–9. doi:10.1093/eurheartj/ehr404. PMID 22067089.
- Philpot, J (2011). "MYTHS AND FACTS ABOUT HEALTH CARE ADVANCE DIRECTIVES" (PDF). American Bar Association.
- Coleman D (2013-07-23). "Full Written Public Comment: Disability Related Concerns About POLST". Not Dead Yet. Retrieved 2018-12-12.
- Jesus JE, Allen MB, Michael GE, Donnino MW, Grossman SA, Hale CP, Breu AC, Bracey A, O'Connor JL, Fisher J (July 2013). "Preferences for resuscitation and intubation among patients with do-not-resuscitate/do-not-intubate orders". Mayo Clinic Proceedings. 88 (7): 658–65. doi:10.1016/j.mayocp.2013.04.010. PMID 23809316.
- "DNR Guidelines for Medical ID Wearers". www.americanmedical-id.com. Retrieved 2019-08-02.
- Holt, Gregory E.; Sarmento, Bianca; Kett, Daniel; Goodman, Kenneth W. (2017-11-30). "An Unconscious Patient with a DNR Tattoo". New England Journal of Medicine. 377 (22): 2192–2193. doi:10.1056/NEJMc1713344. ISSN 0028-4793.
- Cooper, Lori; Aronowitz, Paul (October 2012). "DNR Tattoos: A Cautionary Tale". Journal of General Internal Medicine. 27 (10): 1383–1383. doi:10.1007/s11606-012-2059-8. ISSN 0884-8734.
- Dugan D, Riseman J (July 2015). "Do-Not-Resuscitate Orders in an Operating Room Setting #292". Journal of Palliative Medicine. 18 (7): 638–9. doi:10.1089/jpm.2015.0163. PMID 26091418.
- Rubin E, Courtwright A (November 2013). "Medical futility procedures: what more do we need to know?". Chest. 144 (5): 1707–1711. doi:10.1378/chest.13-1240. PMID 24189864.
- Swetz KM, Burkle CM, Berge KH, Lanier WL (July 2014). "Ten common questions (and their answers) on medical futility". Mayo Clinic Proceedings. 89 (7): 943–59. doi:10.1016/j.mayocp.2014.02.005. PMID 24726213.
- Burns JP, Truog RD (December 2007). "Futility: a concept in evolution". Chest. 132 (6): 1987–93. doi:10.1378/chest.07-1441. PMID 18079232.
- Garrido MM, Harrington ST, Prigerson HG (December 2014). "End-of-life treatment preferences: a key to reducing ethnic/racial disparities in advance care planning?". Cancer. 120 (24): 3981–6. doi:10.1002/cncr.28970. PMC 4257859. PMID 25145489.
- Humble MB (November 2014). "Do-Not-Resuscitate Orders and Suicide Attempts: What Is the Moral Duty of the Physician?". The National Catholic Bioethics Quarterly. 14 (4): 661–71. doi:10.5840/ncbq201414469.
- Hébert PC, Selby D (April 2014). "Should a reversible, but lethal, incident not be treated when a patient has a do-not-resuscitate order?". CMAJ. 186 (7): 528–30. doi:10.1503/cmaj.111772. PMC 3986316. PMID 23630240.
- Capone's paper, and the original by Jesus et al. say the patients were asked about CPR, but the questionnaire shows they were only asked whether they wanted intubation in various scenarios. This is an example of doctors using the term resuscitation to cover other treatments than CPR. {{title Capone RA (March 2014). "Problems with DNR and DNI orders". Ethics & Medics. 39 (3): 1–3.
- Jesus (2013). "Supplemental Appendix of Preferences for Resuscitation and Intubation..." (PDF). Cite journal requires
|journal=(help) - Periyakoil VS, Neri E, Fong A, Kraemer H (2014-05-28). "Do unto others: doctors' personal end-of-life resuscitation preferences and their attitudes toward advance directives". PLOS ONE. 9 (5): e98246. Bibcode:2014PLoSO...998246P. doi:10.1371/journal.pone.0098246. PMC 4037207. PMID 24869673.
- Pfeifer M, Quill TE, Periyakoil VJ (2014). "Physicians provide high-intensity end-of-life care for patients, but "no code" for themselves". Medical Ethics Advisor. 30 (10).
- Daeschler M, Verdino RJ, Caplan AL, Kirkpatrick JN (August 2015). "Defibrillator Deactivation against a Patient's Wishes: Perspectives of Electrophysiology Practitioners". Pacing and Clinical Electrophysiology. 38 (8): 917–24. doi:10.1111/pace.12614. PMID 25683098.
- Breu, Anthony C.; Herzig, Shoshana J. (October 2014). "Differentiating DNI from DNR: Combating code status conflation: Differentiating DNI From DNR". Journal of Hospital Medicine. 9 (10): 669–670. doi:10.1002/jhm.2234. PMC 5240781. PMID 24978058.
- Esteban (2002). "CHARACTERISTICS AND OUTCOMES IN ADULT PATIENTS RECEIVING MECHANICAL VENTILATION" (PDF). JAMA. doi:10.1001/jama.287.3.345.
- Mockford C, Fritz Z, George R, Court R, Grove A, Clarke B, Field R, Perkins GD (March 2015). "Do not attempt cardiopulmonary resuscitation (DNACPR) orders: a systematic review of the barriers and facilitators of decision-making and implementation". Resuscitation. 88: 99–113. doi:10.1016/j.resuscitation.2014.11.016. PMID 25433293.
- Meyer C. "Allow Natural Death — An Alternative To DNR?". Rockford, Michigan: Hospice Patients Alliance.
- Sinclair, Christian (2009-03-05). "Do Not (Attempt) Resuscitation vs. Allow Natural Death". Pallimed.org.
- Youngner, S. J.; Chen, Y.-Y. (2008-12-01). ""Allow natural death" is not equivalent to "do not resuscitate": a response". Journal of Medical Ethics. 34 (12): 887–888. doi:10.1136/jme.2008.024570. ISSN 0306-6800. PMID 19065754.
- Pollak AN, Edgerly D, McKenna K, Vitberg DA, et al. (American Academy of Orthopaedic Surgeons) (2017). Emergency Care and Transportation of the Sick and Injured. Jones & Bartlett Learning. p. 540. ISBN 978-1-284-10690-9.
- Vincent JL, Van Vooren JP (December 2002). "[NTBR (Not to Be Resuscitated) in 10 questions]". Revue Medicale de Bruxelles. 23 (6): 497–9. PMID 12584945.
- Gibbs AJ, Malyon AC, Fritz ZB (June 2016). "Themes and variations: An exploratory international investigation into resuscitation decision-making". Resuscitation. 103: 75–81. doi:10.1016/j.resuscitation.2016.01.020. PMC 4879149. PMID 26976676.
- "Mideast med-school camp: divided by conflict, united by profession". The Globe and Mail. August 2009. Retrieved 2009-08-22.
In hospitals in Jordan and Palestine, neither families nor social workers are allowed in the operating room to observe resuscitation, says Mohamad Yousef, a sixth-year medical student from Jordan. There are also no DNRs. “If it was within the law, I would always work to save a patient, even if they didn't want me to,” he says.
- Al Amir S (25 September 2011). "Nurses deny knowledge of 'do not resuscitate' order in patient's death". The National. United Arab Emirates. Retrieved 12 April 2018.
- "Decisions relating to cardiopulmonary resuscitation: A joint statement from the British Medical Association, the Resuscitation Council (UK) and the Royal College of Nursing" (PDF). Resus.org.uk. Resuscitation Council (UK). Retrieved 17 June 2014.
- Scottish Government (May 2010). "Do Not Attempt Cardiopulmonary Resuscitation (DNACPR): Integrated Adult Policy" (PDF). NHS Scotland.
- Eckberg E (April 1998). "The continuing ethical dilemma of the do-not-resuscitate order". AORN Journal. Retrieved 2009-08-23.
The right to refuse or terminate medical treatment began evolving in 1976 with the case of Karen Ann Quinlan v New Jersey (70NJ10, 355 A2d, 647 [NJ 1976]). This spawned subsequent cases leading to the use of the DNR order.(4) In 1991, the Patient Self-Determination Act mandated hospitals ensure that a patient's right to make personal health care decisions is upheld. According to the act, a patient has the right to refuse treatment, as well as the right to refuse resuscitative measures.(5) This right usually is accomplished by the use of the DNR order.
- "DO NOT RESUSCITATE – ADVANCE DIRECTIVES FOR EMS Frequently Asked Questions and Answers". State of California Emergency Medical Services Authority. 2007. Archived from the original on 2009-08-23. Retrieved 2009-08-23.
# What if the EMT cannot find the DNR form or evidence of a MedicAlert medallion? Will they withhold resuscitative measures if my family asks them to? No. EMS personnel are taught to proceed with CPR when needed, unless they are absolutely certain that a qualified DNR advance directive exists for that patient. If, after spending a reasonable (very short) amount of time looking for the form or medallion, they do not see it, they will proceed with lifesaving measures.
- "Frequently Asked Questions re: DNR's". New York State Department of Health. 1999-12-30. Retrieved 2009-08-23.
May EMS providers accept living wills or health care proxies? A living will or health care proxy is NOT valid in the prehospital setting
- "Do Not Resuscitate Orders". Princess Margaret Hospital d. Archived from the original on 2014-07-15. Retrieved 2012-12-05.
- "Respect for the right to choose - Resources". Dying with dignity, Victoria. 2017. Retrieved 2017-06-14.
- "Using resuscitation plans in end of life decisions" (PDF). Government of New South Wales Health Department. 2014-09-08. Retrieved 2017-06-14.
- it:Omicidio del consenziente (ordinamento penale italiano)
- Rubulotta, F.; Rubulotta, G.; Santonocito, C.; Ferla, L.; Celestre, C.; Occhipinti, G.; Ramsay, G. (March 2010). "End-of-life care is still a challenge for Italy". Minerva Anestesiologica. 76 (3): 203–208. ISSN 1827-1596. PMID 20203548.
- Fan SY, Wang YW, Lin IM (October 2018). "Allow natural death versus do-not-resuscitate: titles, information contents, outcomes, and the considerations related to do-not-resuscitate decision". BMC Palliative Care. 17 (1): 114. doi:10.1186/s12904-018-0367-4. PMC 6180419. PMID 30305068.
- Blank, Robert H. (May 2011). "End-of-Life Decision Making across Cultures". The Journal of Law, Medicine & Ethics. 39 (2): 201–214. doi:10.1111/j.1748-720X.2011.00589.x. ISSN 1073-1105.
- Wen, Kuei-Yen; Lin, Ya-Chin; Cheng, Ju-Feng; Chou, Pei-Chun; Wei, Chih-Hsin; Chen, Yun-Fang; Sun, Jia-Ling (September 2013). "Insights into Chinese perspectives on do-not-resuscitate (DNR) orders from an examination of DNR order form completeness for cancer patients". Supportive Care in Cancer. 21 (9): 2593–2598. doi:10.1007/s00520-013-1827-2. ISSN 0941-4355. PMC 3728434. PMID 23653012.
- Nakagawa, Yoshihide; Inokuchi, Sadaki; Kobayashi, Nobuo; Ohkubo, Yoshinobu (April 2017). "Do not attempt resuscitation order in Japan". Acute Medicine & Surgery. 4 (3): 286–292. doi:10.1002/ams2.271. PMC 5674456. PMID 29123876.
- Cherniack, E P (2002-10-01). "Increasing use of DNR orders in the elderly worldwide: whose choice is it?". Journal of Medical Ethics. 28 (5): 303–307. doi:10.1136/jme.28.5.303. PMC 1733661. PMID 12356958.
- Pennec, Sophie; Monnier, Alain; Pontone, Silvia; Aubry, Régis (2012-12-03). "End-of-life medical decisions in France: a death certificate follow-up survey 5 years after the 2005 act of parliament on patients' rights and end of life". BMC Palliative Care. 11: 25. doi:10.1186/1472-684X-11-25. ISSN 1472-684X. PMC 3543844. PMID 23206428.
- Pennec, Sophie; Monnier, Alain; Pontone, Silvia; Aubry, Régis (2012-12-03). "End-of-life medical decisions in France: a death certificate follow-up survey 5 years after the 2005 act of parliament on patients' rights and end of life". BMC Palliative Care. 11: 25. doi:10.1186/1472-684X-11-25. ISSN 1472-684X. PMC 3543844. PMID 23206428.
External links
- "Do Not Resuscitate Orders". MedlinePlus. U.S. National Library of Medicine.
- "Decisions Relating to Cardiopulmonary Resuscitation". Resuscitation Council (UK).