Calcific tendinitis
Calcific tendinitis is a form of tendinitis, a disorder characterized by deposits of hydroxyapatite (a crystalline calcium phosphate) in any tendon of the body, but most commonly in the tendons of the rotator cuff (shoulder), causing pain and inflammation. The condition is related to and may cause adhesive capsulitis ("frozen shoulder").
| Calcific tendinitis | |
|---|---|
| Other names | calcific/calcifying/calcified/calcareous tendinitis/tendonitis/tendinopathy, tendinosis calcarea, hydroxyapatite deposition disease (HADD), calcific periarthritis |
 | |
| A plain X ray of the shoulder showing calcific tendinitis | |
| Specialty | Rheumatology |
| Symptoms | Pain of the shoulder exacerbated by overhead activities |
| Duration | Self-limiting, typically resolves in 6-9 months |
| Risk factors | Diabetes, hypothyroidism |
| Diagnostic method | X-ray |
| Treatment | Physiotherapy, sub-acromial injection with steroids, extracorporeal shockwave therapy, surgical excision |
| Medication | NSAIDs, analgesics |
It most often occurs in females aged 30 to 60 years.[1] Calcifications are usually located within the supraspinatus tendon (80% of cases), followed by the infraspinatus (15% of cases) and subscapularis (5% of cases) tendons; and are present in 5% or more of asymptomatic shoulders in healthy adults.[2]
Signs and symptoms
Around 50% of individuals with calcific tendinitis have symptoms. Symptoms include pain or weakness in the shoulder, and often leads to decreased active range of motion. If the condition is chronic, muscle atrophy and scapular dyskinesia can occur.[3]
Pain is often aggravated by elevation of the arm above shoulder level or by lying on the shoulder. Pain may awaken the patient from sleep. Other complaints may be stiffness, snapping, catching, or weakness of the shoulder.
Cause
Three main theories have emerged in an attempt to explain the mechanisms involved in tendon calcification.[4] The first theory is the theory of reactive calcification and involves an active cell-mediated process, usually followed by spontaneous resorption by phagocytosing multinucleated cells showing a typical osteoclast phenotype. The second theory suggests that calcium deposits are formed by a process resembling endochondral ossification. The mechanism involves regional hypoxia, which transforms tenocytes into chondrocytes. The third theory involves ectopic bone formation from metaplasia of mesenchymal stem cells normally present in tendon tissue into osteogenic cells. As no single theory is satisfactory to explain all cases, calcific tendinopathy is currently believed to be multifactorial.[4]
Risk factors that increase the chance of developing calcific tendinitis include; hormonal disorders, like diabetes and hypothyroidism, autoimmune disorders, like rheumatoid arthritis, and metabolic disorders that also cause kidney stones, gallstones, and gout. Occupations that consist of repetitive overhead lifting, such as athletes or construction workers, do not seem to significantly increase the likelihood of developing calcific tendinitis.[3]
Diagnosis
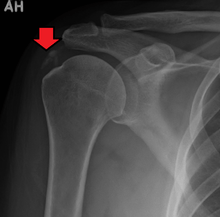
The calcific deposits are visible on X-ray as discrete lumps or cloudy areas. The deposits look cloudy on X-ray if they are in the process of reabsorption, and this is also when they cause the most pain. The deposits are crystalline when in their resting phase and like toothpaste in the reabsorptive phase. However, poor correlation exists between the appearance of a calcific deposit on plain X-rays and its consistency on needling. Ultrasound is also useful to depict calcific deposits and closely correlates with the stage of disease.[4]
Treatment
When treating calcific tendinitis, the goals are to decrease the amount of calcium deposits in the tissue, as well as to reduce the pain and improve function.[5] Usually it improves without specific treatment.[6] Treatments of calcific tendinitis may include physiotherapy, nonsteroidal anti-inflammatory drugs (NSAIDs), or corticosteroid injections.[6] If these do not work, extracorporeal shockwave therapy or surgery may be considered.[6]
Research has found conservative treatment consisting of Physical Therapy, NSAIDS, and steroid injections to be successful in managing 60-80% of cases, such that symptoms did not continue after 6 months. However, it is possible the high success rate is due to the natural progression of the disease.[3]
Medications
Analgesics and NSAIDs are useful to a limited extent. They can be used to relieve pain for 7-14 days, but can cause gastrointestinal, cardiovascular, and renal complications if NSAIDS are used long term.[3] Corticosteroid injections may be useful when the shoulder is acutely inflamed but otherwise are not generally useful except for the temporary relief of pain.
Physical therapy
Physical therapy combines stretching and strengthening of the area to reduce pain and work on range of motion and function. Physical therapy can further work to reduce symptoms with iontophoresis, deep transverse friction massage, laser therapy, or hyperthermia. [3]
Electroanalgesia, ice therapy, and heat offer symptomatic relief. The benefit of ultrasound in calcific tendinitis is debated; most studies are negative but a study by Ebenbichler et al. (1999)[7] showed resolution of deposits and clinical improvement. Improving the biomechanics of the shoulder will reduce the tension on the fault muscles allowing a decrease in symptoms. Improved biomechanics are thought to reduce the amount of calcification that occurs especially in the case of the supraspinatus where it can be caused from repetitive compression against the acromion.
Ultrasound guided percutaneous irrigation
Ultrasound guided percutaneous irrigation (US-PICT) uses sonographic guidance to aspirate and remove calcium deposits while also increasing the vascular supply by causing microtrauma in the area. The technique is followed by a steroid injection to control pain and inflammation. US-PICT removes much of the calcium deposit, and the newly increased vasculature helps to reabsorb whatever calcium is left over. For both short term and long term management, US-PICT has been shown to be 90% successful one year post treatment, and has shown to reduce pain by around 55%. Complications are rare, but most common is bursitis.[3]
Extracorporeal shock wave therapy
In those with calcific tendinitis of the shoulder, high energy extracorporeal shockwave therapy may be useful;[8] it is not useful in other types of tendinitis.[9]
Extra corporeal shockwave therapy (ESWT) can reduce the calcium deposits significantly, thus contributing to decreased pain and increased function. There are different kinds of ESWT. High-energy focused extra corporeal shockwave therapy has been shown to yield the most results when compared with other forms of electrotherapy. Low-energy extra corporeal shockwave therapy, ultrasound and transcutaneous electrical nerve stimulation (TENS) are less likely to break apart the calcium deposits. However, ESWT requires multiple sessions to treat calcific tendinitis and may be quite costly in some countries. [10]
Surgery
Surgery is only recommended once 6 months of conservative, non-operative treatment has failed to reduce symptoms. Additionally, debate remains over whether a complete removal of the deposits is necessary, or if equal pain relief can be obtained from a partial removal of calcium deposits.[3]
Removing the deposits either with open shoulder surgery or arthroscopic surgery are both difficult operations, but with high success rates (around 90%). About 10% require re-operation. If the deposit is large, then frequently the patient will require a rotator cuff repair to fix the defect left in the tendon when the deposit is removed or to reattach the tendon to the bone if the deposit was at the tendon insertion into the bone.
Other
In studies, acetic acid iontophoresis combined with ultrasound provided no better clinical results or shrinkage of the calcific deposits than did no treatment. Platelet-rich plasma (PRP) is blood plasma that has been enriched with platelets. It has not been well studied in calcific tendinitis.[6]
Under local anesthetic, the calcific deposits can be mechanically broken up by puncturing them repeatedly with a needle and then aspirating the calcific material with the help of a sluice of saline. Ultrasound can be used to help localize the deposit and to visualize the needle entering the deposit in real time. Available evidence does not suggest a benefit over usual treatments.[11]
References
- "Evaluation and Management of Calcific Tendinitis". Clinical Advisor. 20 December 2016. Retrieved 12 March 2018.
- Serafini, Giovanni; Sconfienza, Luca M.; Lacelli, Francesca; Silvestri, Enzo; Aliprandi, Alberto; Sardanelli, Francesco (July 2009). "Rotator Cuff Calcific Tendonitis: Short-term and 10-year Outcomes after Two-Needle US-guided Percutaneous Treatment— Nonrandomized Controlled Trial". Radiology. 252 (1): 157–164. doi:10.1148/radiol.2521081816. PMID 19561254.
- Bechay, Joseph; Lawrence, Cassandra; Namdari, Surena (2020-01-01). "Calcific tendinopathy of the rotator cuff: a review of operative versus nonoperative management". The Physician and Sportsmedicine. 0 (0): 1–6. doi:10.1080/00913847.2019.1710617. ISSN 0091-3847. PMID 31893972.
- Arend CF. Ultrasound of the Shoulder. Master Medical Books, 2013. Free chapter on US evaluation of calcific rotator cuff tendinopathy available at ShoulderUS.com
- Wu, Yi-Cheng; Tsai, Wen-Chung; Tu, Yu-Kung; Yu, Tung-Yang (2017-08-01). "Comparative Effectiveness of Nonoperative Treatments for Chronic Calcific Tendinitis of the Shoulder: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials". Archives of Physical Medicine and Rehabilitation. 98 (8): 1678–1692.e6. doi:10.1016/j.apmr.2017.02.030. ISSN 0003-9993. PMID 28400182.
- Carcia, CR; Scibek, JS (March 2013). "Causation and management of calcific tendonitis and periarthritis". Current Opinion in Rheumatology. 25 (2): 204–9. doi:10.1097/bor.0b013e32835d4e85. PMID 23370373.
- Ebenbichler GR, Erdogmus CB, Resch KL, et al. (May 1999). "Ultrasound therapy for calcific tendinitis of the shoulder". N. Engl. J. Med. 340 (20): 1533–8. doi:10.1056/NEJM199905203402002. PMID 10332014.
- Saithna, Adnan; Jenkinson, Emma; Boer, Ronald; Costa, Matt L; Drew, Steve (October 2009). "Is extracorporeal shockwave therapy for calcifying tendinitis of the rotator cuff associated with a significant improvement in the Constant-Murley score? A systematic review:". Current Orthopaedic Practice. 20 (5): 566–571. doi:10.1097/BCO.0b013e3181a5e53d. ISSN 1940-7041.
- Bannuru, RR; Flavin, NE; Vaysbrot, E; Harvey, W; McAlindon, T (Apr 15, 2014). "High-energy extracorporeal shock-wave therapy for treating chronic calcific tendinitis of the shoulder: a systematic review". Annals of Internal Medicine. 160 (8): 542–9. doi:10.7326/m13-1982. PMID 24733195.
- Wu, Yi-Cheng; Tsai, Wen-Chung; Tu, Yu-Kung; Yu, Tung-Yang (2017-08-01). "Comparative Effectiveness of Nonoperative Treatments for Chronic Calcific Tendinitis of the Shoulder: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials". Archives of Physical Medicine and Rehabilitation. 98 (8): 1678–1692.e6. doi:10.1016/j.apmr.2017.02.030. ISSN 0003-9993. PMID 28400182.
- Vignesh, KN; McDowall, A; Simunovic, N; Bhandari, M; Choudur, HN (January 2015). "Efficacy of ultrasound-guided percutaneous needle treatment of calcific tendinitis". AJR. American Journal of Roentgenology. 204 (1): 148–52. doi:10.2214/ajr.13.11935. PMID 25539250.
External links
| Classification |
|---|