Blount's disease
Blount's disease is a growth disorder of the tibia (shin bone) that causes the lower leg to angle inward, resembling a bowleg.It is also known as "tibia vara".[2]
| Blount's disease | |
|---|---|
| Other names | Tibia vara |
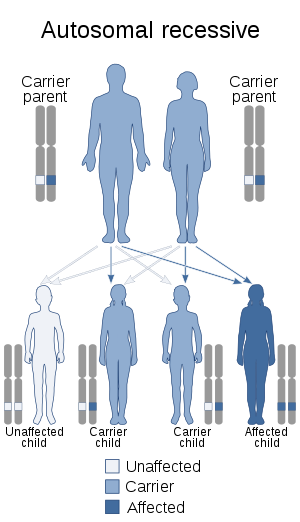 | |
| Blount's disease is inherited in an autosomal recessive manner (may be multifactorial as well).[1] | |
| Specialty | Rheumatology |
It is named after Walter Putnam Blount (1900–1992), an American pediatric orthopedic surgeon.[3][4] It has also been known as Mau-Nilsonne Syndrome, after C. Mau and H. Nilsonne, who published early case reports of the condition.[5][6]
Symptoms and signs
Bowing of one or both legs that may:
- Be rapidly progressive
- Appear asymmetric
- Primarily occur just below the knee
Complications
Failure to treat Blount's disease may lead to progressive deformity. Blount's disease may come back after surgery, especially in younger children. Because of the bowing, a leg-length discrepancy may result. This may result in disability if the discrepancy is significant (greater than 1 inch) and is not treated.
Causes
Blount's disease occurs in young children and adolescents. The cause is unknown but is thought to be due to the effects of weight on the growth plate. The inner part of the tibia, just below the knee, fails to develop normally, causing angulation of the bone.
Unlike bowlegs, which tend to straighten as the child develops, Blount's disease is progressive and the condition worsens. It can cause severe bowing of the legs and can affect one or both legs. This condition is more common among children of African ancestry. It is also associated with obesity, short stature, and early walking.
Diagnosis
Physical examination shows the lower legs to be angled inward. An x-ray of the knee and the lower leg confirms the diagnosis.
Differential Diagnosis
Lower extremity deformities in Rickets can closely mimic those produced by Blount's disease. To differentiate between Rickets and Blount's disease it is important to correlate the clinical picture with laboratory findings such as calcium, phosphorus and alkaline phosphatase. Besides the X-ray appearance. Bone deformities in Rickets have a reasonable likelihood to correct over time, while this is not the case with Blount's disease. Nevertheless both disorders may need surgical intervention in the form of bone osteotomy or more commonly guided growth surgery.[7] Osteochondrodysplasias or genetic bone diseases can cause lower extremity deformities similar to Blount's disease. The clinical appearance and the characteristic radiographic are important to confirm the diagnosis.[8]
Treatment
Children who develop severe bowing before the age of 3 may be treated with knee ankle foot orthoses.[9] However, bracing may fail, or bowing may not be detected until the child is older. In some cases, surgery may be performed.[10] Surgery may involve cutting the shin bone (tibia) to realign it, and sometimes lengthen it as well.Other times, the growth of just the outer half of the tibia can be surgically restricted to allow the child’s natural growth to reverse the bowing process. This second, much smaller surgery is most effective in children with less severe bowing and significant growth remaining.
Return to normal function and cosmetic appearance is expected if the knee can be properly aligned.
References
- "OMIM Entry 259200 - BLOUNT DISEASE, ADOLESCENT". omim.org. Retrieved 7 November 2017.
- Clarke SE, McCarthy JJ, Davidson RS (March 2009). "Treatment of Blount disease: a comparison between the multiaxial correction system and other external fixators". J Pediatr Orthop. 29 (2): 103–9. doi:10.1097/BPO.0b013e3181982a62. PMID 19352232. S2CID 31733527.
- synd/1470 at Who Named It?
- W. P. Blount. Tibia vara: osteochondrosis deformans tibiae. Journal of Bone and Joint Surgery, Boston, 1937, 19: 1-29.
- Mau, C. (1923/24) Genu varum bedingt durch Tihiaepiphysendefekt bei Kartilaginärer Exostose. Z. orthop. Chir. 44, 383.
- Nilsonne, H. (1929) Genu varum mit eigentümlichen Epiphysenveränderungen. Acta chir. scand. 44, 187.
- EL-Sobky, TA; Samir, S; Baraka, MM; Fayyad, TA; Mahran, MA; Aly, AS; Amen, J; Mahmoud, S (1 January 2020). "Growth modulation for knee coronal plane deformities in children with nutritional rickets: A prospective series with treatment algorithm". JAAOS: Global Research and Reviews. 4 (1). doi:10.5435/JAAOSGlobal-D-19-00009. PMID 32159063.
- EL-Sobky, TA; Shawky, RM; Sakr, HM; Elsayed, SM; Elsayed, NS; Ragheb, SG; Gamal, R (15 November 2017). "A systematized approach to radiographic assessment of commonly seen genetic bone diseases in children: A pictorial review". J Musculoskelet Surg Res. 1 (2): 25. doi:10.4103/jmsr.jmsr_28_17. S2CID 79825711.
- Alsancak, S; Guner, S; Kinik, H (2013). "Orthotic variations in the management of infantile tibia vara and the results of treatment". Prosthetics and Orthotics International. 37 (5): 375–83. doi:10.1177/0309364612471369. PMID 23344116. S2CID 24907234.
- McCarthy JJ, MacIntyre NR, Hooks B, Davidson RS (March 2009). "Double osteotomy for the treatment of severe Blount disease". J Pediatr Orthop. 29 (2): 115–9. doi:10.1097/BPO.0b013e3181982512. PMID 19352234. S2CID 21625248.
External links
| Classification | |
|---|---|
| External resources |