Dengue fever
Dengue fever (pronounced DEN-geh or DEN-ghee [The 'g' is the "hard g" as in "get", and the 'u' is silent]) is a viral tropical disease transmitted by mosquito bites. In 2016 over 50 million new cases were reported, about ten million were hospitalized, and over ten thousand died.
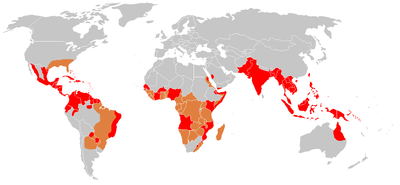
Red: has had recent dengue outbreaks as of 2006.
Orange: dengue outbreaks possible
Dengue is a major public health problem throughout South-East Asia and South Asia. It is also found in Queensland, Australia, the tropical South Pacific islands, Africa, tropical parts of North and South America, including the Caribbean and mainland Central America. According to the World Health Organization, dengue infections have been increasing in recent years and over half the world's population is now at risk.
Dengue is not infectious between humans. It is transmitted to humans mainly by the Aedes aegypti mosquito, which is found in tropical regions throughout the world. The Aedes albopictus mosquito can also carry it; that one tolerates cold better and has been involved in the spread of the disease to Europe and North America. These mosquitoes carry a flavivirus which causes Dengue fever. Other flaviviruses, also insect-borne, cause Yellow fever, Zika fever, Chikungunya, the West Nile disease, and several types of encephalitis.
There are four confirmed strains of the virus and perhaps a fifth. After recovering from an infection, a patient has long-term immunity to the strain they had but only a few months reststance to other strains.
The main preventive measures are to prevent the breeding of mosquitoes and to avoid mosquito bites. No vaccine was available until recently, but in 2016 the first vaccine came on the market; see below.
Signs and symptoms
About 80% of people infected with the virus have no symptoms, or only a mild fever and general malaise. Mild cases without rash may be easily misdiagnosed as flu. Dengue is also easily confused with Zika fever or Chikungunya which are caused by related viruses carried by the same genus of mosquito, are found in overlapping geographic regions, and have similar symptoms.
For the unlucky 20% or so who get full-blown dengue fever, the first symptoms are usually a sudden fever (often over 40°C, 104°F) accompanied by strong joint and muscle pains; in the 19th century it was known as breakbone fever due to these pains. This is usually soon followed by a bright red rash, most often starting on the legs but sometimes the arms and it may spread to torso and face. Splitting headaches, nausea, vomiting and abdominal pain are also common. This stage of the disease is quite unlikely to kill, but the patient may wish it would.
Symptoms usually appear 3-14 days (most commonly 4-7 days) after being bitten by an infected mosquito. The acute symptoms typically last a few days or a week, but milder flu-like symptoms often persist beyond that; many patients are miserable for weeks and for some it takes several months to fully recover. Fatality rates are around 1 in 1000, nearly all in cases that progress to dengue hemorrhagic fever.
A few cases become dengue hemorrhagic fever (DHF), in which blood vessels become more porous and start to leak fluids; fortunately this is fairly rare. The most common symptom is bleeding from the nose, mouth, and gums, but accumulation of fluids in the abdomen or lungs, bleeding in the intestinal tract, vaginal bleeding, or bleeding under the skin are also possible. There can be a fever of 42°C (107°F) or higher, which is an emergency in itself.
There are four strains of the dengue virus and DHF occurs more often in people who have recovered from an infection with one strain but then get re-infected with a different strain. The reason for this is not known for certain; one theory is that the immune system, instead of fighting the second strain, gets confused and just makes lots of antibodies against the first.
The fatality rate for DHF with proper treatment is only about 1%, but it is a life-threatening illness which usually requires hospitalization, and often some time in an intensive care ward. Treatment involves major interventions – transfusions, other intravenous fluids, sometimes oxygen to compensate for blood or lung problems, perhaps medication to reduce bleeding, and so on. The main goal is to prevent the patient from progressing to dengue shock syndrome, and this can usually be achieved.
The nastiest form of the disease is dengue shock syndrome (DSS) in which so much fluid is lost that pulse rate and blood pressure drop precipitously. This is a critical emergency; it is lethal in 90% of cases unless correctly and very promptly treated, and once the disease has progressed to this point there is risk of death even with good treatment.
Treatment
There is no treatment that can attack the virus or cure the disease, only ones to alleviate symptoms such as pain, fever or nausea, or to deal with dehydration and blood loss. For mild cases, rest and fluids may be enough, but check with a doctor about other treatment.
In areas with dengue, if you get some of the symptoms described above (especially after being bitten by a mosquito) see a doctor. The presence of dengue can be confirmed with a blood test, and much of the misery can be avoided with treatment. Not all cases need hospitalization, but most will be too ill for work or travel for anything from a few days to a few weeks.
| WARNING: If dengue fever is a possibility, do not self-medicate without medical advice. Some common over-the-counter medicines such as aspirin and ibuprofen, commonly sold as headache remedies, increase the risk of DHF. Any medication containing acetylsalicyclic acid or nonsteroidal anti-inflammatory agents should be avoided. Paracetamol (acetominophen) is often used instead to manage the fever and pain. | |
Dengue hemorrhagic fever is a life-threatening illness; if you show any DHF symptoms, see a doctor immediately. If a local hospital has a good emergency room, go directly there.
Treating dengue hemorrhagic fever requires the resources of a modern hospital. If you are out in the boondocks and come down with dengue fever, consider evacuating immediately to somewhere with such a hospital. If your case does develop into DHF, then you will urgently need treatment but might be in no shape to travel.
If you get dengue fever during a long trip, talk to your doctor about your prognosis. The disease leaves some people debilitated (about like flu) for anything up to several months, and if you are one of the unlucky ones you may need to alter your travel plans: postpone strenuous activities and go lie on a beach or take it easy in some other way until you recover fully. Some people may even need to cut a trip short and go home to recover.
Preventive measures
Preventive measures to control and avoid dengue fever focus on avoiding mosquito bites and include:
- Prevention or elimination of standing water sources, such as pools of water that collect in containers, flower pots, discarded tires or coconut shells, etc. Mosquitoes will breed in any standing water in a matter of days.
- Use of permethrin-treated fabrics which kill insects that land on them.
- Use of mosquito netting especially for the place you sleep in even if mosquitoes "can't enter" the house.
- Use of insect repellent (DEET or picardin are the main agents that have been shown to be most effective) as well as wearing clothing that covers exposed skin.
- Houses constructed in such a way as to reduce the entry of mosquitoes. (e.g. screens on the windows a/c instead of open windows/ventilators...)
Most electronic bug zappers are not effective against mosquitoes since mosquitoes are not attracted to light. There are some models which emit carbon dioxide or octenol (found in the breath of mammals) so they do attract mosquitoes.
See mosquitoes for more detailed discussion.
Vaccine
The first vaccine to prevent dengue fever reached the market in 2016; it is effective against all four strains of the virus. It needs three shots six months apart, and is recommended for the age range used in testing, 9-45.
Sanofi Pasteur, the French company who developed it, are seeking approval first in countries like Mexico, Thailand, Brazil and the Philippines – places that need it and have moderately high incomes – and leaving US and European approval for later, so travellers may need to get the shot at their destination.
The vaccine was approved in Brazil, Mexico and the Philippines in December 2015 and other approvals are expected to follow. However, there are complications; the Philippine government withdrew their approval in 2017 and Sanofi no longer recommend that the vaccine be used by people who have not previously been exposed to the virus.