Renal cyst
A renal cyst is a fluid collection in or on the kidney. There are several types based on the Bosniak classification. The majority are benign, simple cysts that can be monitored and not intervened upon. However, some are cancerous or are suspicious for cancer and are commonly removed in a surgical procedure called nephrectomy.
| Renal cyst | |
|---|---|
| Other names | Kidney cysst |
 | |
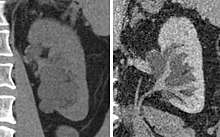
| Renal cyst of the left kidney (hyperintense area) as shown on MRI. | |
| Specialty | Urology |

Numerous renal cysts are seen in the cystic kidney diseases, which include polycystic kidney disease and medullary sponge kidney.
Classification
Renal cysts are classified by malignant risk using the Bosniak Classification System. The system was created by Dr. Morton Bosniak, a faculty member at the New York University Langone Medical Center in New York City.[1]
The Bosniak classification categorizes renal cysts into five groups.[2]
Category I
- Benign simple cyst with thin wall without septa, calcifications, or solid components, and has a density of 0–20 Hounsfield units (HU)[3] (about equal to that of water). In such cases, a CT scan without intravenous contrast is enough for classification.[4] Still, if a contrast CT is performed, a category I cyst should not show significant enhancement,[4] which can be regarded as an increase of less than 10HU.[5]
Category II
- Benign cyst with a few thin septa, which may contain fine calcifications or a small segment of mildly thickened calcification. This includes homogenous, high-attenuation (60–70 Hounsfield units[3]) lesions less than 3 cm with sharp margins but without enhancement. Hyperdense cysts must be exophytic with at least 75 percent of its wall outside the kidney to allow for appropriate assessment of margins, otherwise they are categorized as IIF.[6]

Category IIF
This category includes renal cysts with multiple thin septa, a septum thicker than hairline, slightly thick wall, or with calcification, which may be thick.
It also includes intrarenal cysts larger than 3 centimetres (1.2 inches) if:
- there is no contrast enhancement (otherwise category III).[7]
- there is high attenuation or there is a maximum 25% of their walls visible outside the kidney (otherwise category II).[3]
Category IIF cysts have a 5–10% risk of being kidney cancer, and therefore follow-up is recommended. However, there is no consensus recommendation on the appropriate interval of follow up.[7]
Category III
- Indeterminate cystic masses with thickened irregular septa with enhancement. 50 percent of these lesions are ultimately found to be malignant.
Category IV
- Malignant cystic masses with all the characteristics of category III lesions but also with enhancing soft tissue components independent of but adjacent to the septa. 100 percent of these lesions are malignant.
| Bosniak category | |||||
|---|---|---|---|---|---|
| I | II | IIF | III | IV | |
| Attenuation[3] | 0–20 HU | 60–70 Hounsfield units | |||
| Walls[3] | Thin and smooth | Small and fine calcifications | Nodular or irregular calcifications | Thick, heterogeneous. Gross calcifications with enhancement | |
| Solid components[3] | No | Yes | |||
Diagnosis
The complex cyst can be further evaluated with doppler ultrasonography, and for Bosniak classification and follow-up of complex cysts, either contrast-enhanced ultrasound (CEUS) or contrast CT is used.[8]
 Renal ultrasonography of a simple renal cyst with posterior enhancement.
Renal ultrasonography of a simple renal cyst with posterior enhancement. Advanced polycystic kidney disease with multiple cysts.[8]
Advanced polycystic kidney disease with multiple cysts.[8] Renal cyst as seen on abdominal ultrasound
Renal cyst as seen on abdominal ultrasound Renal cyst as seen on abdominal ultrasound
Renal cyst as seen on abdominal ultrasound Renal cyst as seen on abdominal ultrasound
Renal cyst as seen on abdominal ultrasound
Treatment
This system is more directly focused on the most appropriate management. These alternatives are broadly to ignore the cyst, schedule follow-up or perform a surgical excision of it. When a cyst shows discrepancy in severity across categories, it is the most worrisome feature that is used in deciding about management. There is no established rule regarding the follow-up frequency, but one possibility is after 6 months, which can later be doubled if unchanged.[5]
| Recommended management[5] | |||
|---|---|---|---|
| Ignore | Follow | Excise | |
| Calcification |
|
Thick, nodular | |
| If radiodensity > 20 HU without radiocontrast |
|
|
|
| Septations | Thin and smooth | Slightly greater than hairline |
|
| Enhancement (increase with radiocontrast) | < 10 HU | 10–15 HU | > 15 HU |
| Multilocular | If infection | All others | |
| Nodularity[5] | Very small and nonenhancing | All others | |
| Wall thickening[5] | If infection | All others | |
Peripelvic versus parapelvic cysts
Parapelvic cysts originate from around the kidney at the adjacent renal parenchyma, and plunge into the renal sinus. Peripelvic cysts are contained entirely within the renal sinus, possibly related to dilated lymphatic channels. When viewed on CT in absence of contrast, they can mimic hydronephrosis.[9] If symptomatic, they can be laparoscopically decorticated - removal of the outer layer or cortex.[10]
Epidemiology
Up to 27 percent of individuals older than 50 years may have simple renal cysts that cause no symptoms.[11]
See also
- Renal tumor
References
- http://urology.med.nyu.edu/conditions-we-treat/renal-cysts
- Curry NS, Cochran ST, Bissada NK (August 2000). "Cystic renal masses: accurate Bosniak classification requires adequate renal CT". American Journal of Roentgenology. 175 (2): 339–42. doi:10.2214/ajr.175.2.1750339. PMID 10915671.
- Muglia, Valdair F.; Westphalen, Antonio Carlos (2014). "Classificação de Bosniak para cistos renais complexos: histórico e análise crítica". Radiologia Brasileira. 47 (6): 368–373. doi:10.1590/0100-3984.2013.1797. ISSN 0100-3984. PMC 4341374. PMID 25741120.
- Karen Garfield and Stephen W. Leslie (2019-03-14). Simple Renal Cyst. National Center for Biotechnology Information, StatPearls. StatPearls.
- David S. Hartman, MD and Ileana Chesaru, MD. "Kidney – Cystic masses". Radiology Assistant. Retrieved 2017-10-20.CS1 maint: multiple names: authors list (link)
- De Miranda, C. M.; Maranhão, C. P.; Dos Santos, C. J.; Padilha, I. G.; De Farias Lde, P; Da Rocha, M. S. (2014). "Bosniak classification of renal cystic lesions according to multidetector computed tomography findings". Radiologia Brasileira. 47 (2): 115–21. doi:10.1590/S0100-39842014000200015. PMC 4337166. PMID 25741060.
- "Bosniak classification of renal cystic disease". GPnotebook. Retrieved 2017-05-17.
- Hansen, Kristoffer; Nielsen, Michael; Ewertsen, Caroline (2015). "Ultrasonography of the Kidney: A Pictorial Review". Diagnostics. 6 (1): 2. doi:10.3390/diagnostics6010002. ISSN 2075-4418. PMC 4808817. PMID 26838799. (CC-BY 4.0)
- Zinn, H. L.; Becker, J. A. (1997). "Peripelvic cysts simulating hydronephrosis". Abdominal Imaging. 22 (3): 346–7. doi:10.1007/s002619900205. PMID 9107666.
- Shiraishi, K; Eguchi, S; Mohri, J; Kamiryo, Y (2006). "Laparoscopic decortication of symptomatic simple renal cysts: 10-year experience from one institution". BJU International. 98 (2): 405–8. doi:10.1111/j.1464-410X.2006.06249.x. PMID 16879687.
- Tada S, Yamagishi J, Kobayashi H, Hata Y, Kobari T (July 1983). "The incidence of simple renal cyst by computed tomography". Clinical Radiology. 34 (4): 437–9. doi:10.1016/S0009-9260(83)80238-4. PMID 6872451.