Propofol infusion syndrome
Propofol infusion syndrome (PRIS) is a rare syndrome which affects patients undergoing long-term treatment with high doses of the anaesthetic and sedative drug propofol. It can lead to cardiac failure, rhabdomyolysis, metabolic acidosis, and kidney failure, and is often fatal.[1][2][3] High blood potassium, high blood triglycerides, and liver enlargement, proposed to be caused by either "a direct mitochondrial respiratory chain inhibition or impaired mitochondrial fatty acid metabolism"[4] are also key features. It is associated with high doses and long-term use of propofol (> 4 mg/kg/h for more than 24 hours). It occurs more commonly in children, and critically ill patients receiving catecholamines and glucocorticoids are at high risk. Treatment is supportive. Early recognition of the syndrome and discontinuation of the Propofol infusion reduces morbidity and mortality.
| Propofol infusion syndrome | |
|---|---|
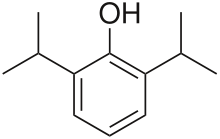 | |
| Propofol |
Presentation
The syndrome clinically presents as acute refractory bradycardia that leads to asystole, in the presence of one or more of the following conditions; metabolic acidosis, rhabdomyolysis, hyperlipidemia, and enlarged liver. The association between PRIS and Propofol infusions is generally noted at infusions higher than 4 mg.kg for greater than 48 hours.[4]
Mechanism of Action
The mechanism of action is poorly understood but may involve the impairment of mitochondrial fatty acid metabolism by Propofol.[4]
Risk Factors
Predisposing factors seem to include young age, severe critical illness of central nervous system or respiratory origin, exogenous catecholamine or glucocorticoid administration, inadequate carbohydrate intake and subclinical mitochondrial disease.[4]
Treatment
Treatment options are limited and are usually supportive, including Hemodialysis with cardiorespiratory support.[4]
References
- Vasile, Vasile B; Rasulo F; Candiani A; Latronico N. (September 2003). "The pathophysiology of propofol infusion syndrome: a simple name for a complex syndrome". Intensive Care Medicine. 29 (9): 1417–25. doi:10.1007/s00134-003-1905-x. PMID 12904852.
- Zaccheo, Melissa M; Bucher, Donald H. (June 2008). "Propofol Infusion Syndrome: A Rare Complication With Potentially Fatal Results". Critical Care Nurse. 28 (3): 18–25. PMID 18515605.
- Sharshar, T. (2008). "[ICU-acquired neuromyopathy, delirium and sedation in intensive care unit]". Ann Fr Anesth Reanim. 27 (7–8): 617–22. doi:10.1016/j.annfar.2008.05.010. PMID 18584998.
- Kam, PC; Cardone D. (July 2007). "Propofol infusion syndrome". Anaesthesia. 62 (7): 690–701. doi:10.1111/j.1365-2044.2007.05055.x. PMID 17567345.