Phlegmasia cerulea dolens
Phlegmasia cerulea dolens (literally: painful blue inflammation) is an uncommon severe form of deep venous thrombosis which results from extensive thrombotic occlusion (blockage by a thrombus) of the major and the collateral veins of an extremity.[1][2] It is characterized by sudden severe pain, swelling, cyanosis and edema of the affected limb. There is a high risk of massive pulmonary embolism, even under anticoagulation. Foot gangrene may also occur. An underlying malignancy is found in 50% of cases. Usually, it occurs in those afflicted by a life-threatening illness.[1]
| Phlegmasia cerulea dolens | |
|---|---|
 | |
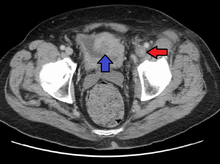
| A person with a two hour history of phlegmasia cerulea dolens (left leg, right side of image) |
This phenomenon was discovered by Jonathan Towne, a vascular surgeon in Milwaukee, who was also the first to report the "white clot syndrome" (now called heparin induced thrombocytopenia [HIT]). Two of their HIT patients developed phlegmasia cerulea dolens that went on to become gangrenous.[3]
Treatment is by catheter-directed thrombolytic therapy, a type of thrombolysis.[4]
Additional images
See also
References
- John T. Owings (December 2005). "Management of Venous Thromboembolism". ACS Surgery. American College of Surgeons. Archived from the original on January 27, 2012. Retrieved January 16, 2012.
- Barham, Kalleen; Tina Shah (2007-01-18). "Images in Clinical Medicine: Phlegmasia Cerulea Dolens". The New England Journal of Medicine. 356 (3): e3. doi:10.1056/NEJMicm054730. PMID 17229945.
- Heparin-Induced Thrombocytopenia By Theodore E. Warkentin, Andreas Greinacher, Published 2004, ISBN 0-8247-5625-8
- Tran HA, Gibbs H, Merriman E, Curnow JL, Young L, Bennett A, Tan C, Chunilal SD, Ward CM, Baker R, Nandurkar H (March 2019). "New guidelines from the Thrombosis and Haemostasis Society of Australia and New Zealand for the diagnosis and management of venous thromboembolism". The Medical Journal of Australia. 210 (5): 227–235. doi:10.5694/mja2.50004. PMID 30739331.
External links
| Classification | |
|---|---|
| External resources |