Male accessory gland infection
Male accessory gland infection (MAGI) is a condition with signs of inflammation involving one or more sites in the male genital tract. Diagnosis is made according to parameters defined by the World Health Organization, and it is particularly made in relation to infectious or inflammatory causes of male infertility.
| Male accessory gland infection | |
|---|---|
| Other names | Male accessory gland inflammation[1] |
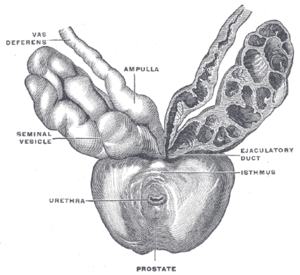 | |
| Prostate with seminal vesicles and seminal ducts, viewed from in front and above | |
| Specialty | Urology |
Although it is usually caused by infection spreading from the urethra, non-infectious causes also exist.
Definition
MAGI includes infections (bacterial, viral, fungal etc.) involving one or more of the following male genital organs or tracts:[2]
- seminal vesicles (seminal vesiculitis)
- prostate gland (prostatitis)
- vas deferens
- epididymis (epididymitis)
- testicles (orchitis)
- urethra (urethritis)
- Cowper's glands
Diagnosis
As infection has a negative impact on the secretory function of the accessory glands, findings that could indicate the presence of MAGI include:[3]
- signs of inflammation in a semen analysis (leukocytes ≥ 1x106/mL and/or elastase ≥ 230 ng/mL)
- low semen volume
- elevated semen pH
- low levels of alpha-glucosidase, fructose and zinc
WHO criteria
MAGI can be diagnosed when there are two or more factors present that meet criteria defined by the World Health Organization (WHO):[1][4]
| Factors | Description | For positive diagnosis |
|---|---|---|
| A | History of:
Physical signs:
|
(i) Any one Factor A feature plus (ii) one feature from either Factor B or Factor C |
| B | Prostatic fluid:
|
(i) Either one of the Factor B features plus (ii) one feature from either Factor A or Factor C |
| C | Semen:
|
Any two Factor C features or (i) any one Factor C featureplus (ii) one feature from either Factor A or Factor B |
Biomarkers
One study has proposed that elevated levels of soluble urokinase-type plasminogen activator receptor (SuPAR) in seminal plasma might be useful as a marker for MAGI.[5]
Causes
The main infectious agents are Enterobacteriaceae (such as Escherichia coli and Klebsiella), Neisseria gonorrhoeae, and Chlamydia trachomatis.[2]
One study has shown that men with MAGI who have lower serum levels of total testosterone tend to have a more complicated form of MAGI, such as involving more than one site, than those with normal levels.[6]
Complications
Potential complications include:[2][3][7]
- obstruction of the epididymis
- impairment of spermatogenesis
- impairmentment of sperm function
- induction of sperm auto-antibodies
- dysfunctions of the male accessory glands
These complications can result in sexual dysfunction[7] and male subfertility.[4][8]
References
- Rosita A Condorelli; Enzo Vicari; Aldo E Calogero; Sandro La Vignera (25 April 2014). "Male accessory gland inflammation prevalence in type 2 diabetic patients with symptoms possibly reflecting autonomic neuropathy". Asian Journal of Andrology. 16 (5): 761–766. doi:10.4103/1008-682X.125911. PMC 4215658. PMID 24799635.
- Walter K.H. Krause (April 2008). "Male accessory gland infection". Andrologia. 40 (2): 113–116. doi:10.1111/j.1439-0272.2007.00822.x. PMID 18336461.
- Marcelo Marconi; Adrian Pilatz; Florian Wagenlehner; Thorsten Diemer; Wolfgang Weidner (May–June 2009). "Impact of infection on the secretory capacity of the male accessory glands". International Brazilian Journal of Urology. 35 (3): 299–308. doi:10.1016/S0022-5347(09)60344-X. PMID 19538765.
- Sandro La Vignera; Enzo Vicari; Rosita A Condorelli; R D'Agata; Aldo E Calogero (November 2011). "Hypertrophic-congestive and fibro-sclerotic ultrasound variants of male accessory gland infection have different sperm output". Journal of Endocrinological Investigation. 34 (10): e330–e335. doi:10.1007/bf03346729. PMID 22234181.
- C. Autilio; R. Morelli; D. Milardi; G. Grande; R. Marana; A. Pontecorvi; C. Zuppi; S. Baroni (September 2015). "Soluble urokinase-type plasminogen activator receptor as a putative marker of male accessory gland inflammation". Andrology. 3 (6): 1054–61. doi:10.1111/andr.12084. PMID 26384478.
- R. A. Condorelli; A. E. Calogero; E. Vicari; V. Favilla; S. Cimino; G. I. Russo; G. Morgia; S. La Vignera (8 September 2014). "Male Accessory Gland Infection: Relevance of Serum Total Testosterone Levels". International Journal of Endocrinology. 2014 (915752): 915752. doi:10.1155/2014/915752. PMC 4172872. PMID 25276133.
- Sandro La Vignera; Rosita A Condorelli; Enzo Vicari; R D'Agata; Aldo E Calogero (May 2012). "High frequency of sexual dysfunction in patients with male accessory gland infections". Andrologia. 44 (Supplement s1): 438–446. doi:10.1111/j.1439-0272.2011.01202.x. PMID 21793867.
- Sandro La Vignera; Rosita A Condorelli; R D'Agata; Enzo Vicari; Aldo E Calogero (February 2012). "Semen alterations and flow-citometry evaluation in patients with male accessory gland infections". Journal of Endocrinological Investigation. 35 (2): 219–223. doi:10.3275/7924. PMID 21946047.