Kegel exercise
Kegel exercise, also known as pelvic-floor exercise, involves repeatedly contracting and relaxing the muscles that form part of the pelvic floor, now sometimes colloquially referred to as the "Kegel muscles". The exercise can be performed multiple times each day, for several minutes at a time, but take one to three months to begin to have an effect.
| Kegel exercise | |
|---|---|
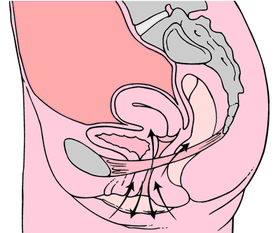 Kegel exercises diagram | |
| Pronunciation | Kegel /ˈkeɪɡəl/ |
| Other names | Pelvic floor exercise, pelvic muscle exercise |
Kegel exercises aim to strengthen the pelvic floor muscles.[1] These muscles have many functions within the human body. In women, they are responsible for: holding up the human bladder, preventing urinary stress incontinence (especially after childbirth), vaginal and uterine prolapse.[2][3] In men, these muscles are responsible for: urinary continence, fecal continence, and ejaculation.[4][3] Several tools exist to help with these exercises, although various studies debate the relative effectiveness of different tools versus traditional exercises.[5]
The American gynecologist Arnold Kegel first published a description of such exercises in 1948.
Mechanism of action
The aim of Kegel exercises is to improve muscle tone by strengthening the pubococcygeus muscles of the pelvic floor. Kegel is a popular prescribed exercise for pregnant women to prepare the pelvic floor for physiological stresses of the later stages of pregnancy and childbirth. Kegel exercises are said to be good for treating vaginal prolapse[6] and preventing uterine prolapse[7] in women and for treating prostate pain and swelling resulting from benign prostatic hyperplasia (BPH) and prostatitis in men. Kegel exercises may be beneficial in treating urinary incontinence in both men and women.[8] Kegel exercises may also increase sexual gratification, allowing women to complete pompoir and aid in reducing premature ejaculation[4] in men. The many actions performed by Kegel muscles include holding in urine and avoiding defecation. Reproducing this type of muscle action can strengthen the Kegel muscles. The action of slowing or stopping the flow of urine may be used as a test of correct pelvic floor exercise technique.[9][10]
It is now known that the components of levator ani (the pelvic diaphragm), namely pubococcygeus, puborectalis and ileococcygeus, contract and relax as one muscle. Hence, pelvic floor exercises involve the entire levator ani rather than pubococcygeus alone. Pelvic floor exercises may be of benefit in cases of fecal incontinence and pelvic organ prolapse conditions e.g. rectal prolapse.[11]
Health effects
Women
Factors such as pregnancy, childbirth, aging, and being overweight often result in the weakening of the pelvic muscles.[12] This can be assessed by either digital examination of vaginal pressure or using a Kegel perineometer. Kegel exercises are useful in regaining pelvic floor muscle strength in such cases.
The symptoms of prolapse and its severity can be decreased with pelvic floor exercises.[13][10] Effectiveness can be improved with feedback on how to do the exercises.[14]
Men
The muscles involved in men's Kegels are called the perineal muscles which can contract both voluntarily and involuntarily. Kegel exercises can train the perineal muscles by increasing oxygen supply to the muscle and increasing the strength of those muscles.[15] The names of the perineal muscles are: Ischiocavernosus (erection), bulbocavernosus (ejaculation), external sphincter of the anus, striated urethral sphincter, transverse perineal, levator of the prostate, and puborectalis.[16]
Premature ejaculation is when male ejaculation occurs after less than one minute of penetration.[17] The perineal muscles are involved in ejaculation when they are involuntarily contracted.[15] The ischiocavernosus are responsible for the male erection and the bulbocavernosus is responsible for ejaculation. By actively contracting the perineal muscles with kegels regularly, strength and control of these muscles will increase, which can aid in reducing premature ejaculation.[15][18]
Urinary incontinence
Pelvic floor exercises (muscle training) can be included in conservative treatment approaches for women with urinary incontinence.[19] There is tentative evidence that biofeedback may give added benefit when used with pelvic floor muscle training.[20] There is no clear evidence that teaching pelvic floor exercises alters the risk of stress urinary incontinence in men that develop this condition post prostatectomy.[21]
In pregnant women, antenatal PFMT probably helps prevent urinary continence during pregnancy and up to six months after giving birth but for pregnant women who already have incontinence, it is not clear if antenatal PFMT helps to reduce symptoms.[16]
Faecal incontinence
In pregnancy, it is not yet clear if antenatal PFMT helps to prevent or treat faecal incontinence.[16]
Pelvic toning devices
Some devices, marketed to women, are for exercising the pelvic floor muscles and to improve the muscle tone of the pubococcygeal or vaginal muscle.


As of 2013 there was no evidence that doing pelvic floor exercise with weights worked better than doing Kegel exercises without weights; there is greater risk with weights, because a foreign object is introduced into the vagina.[22][5]
Inserting foreign objects into the vagina increases the risk of infections and can lead to vaginosis or toxic shock syndrome.[23]
Marketing
During the latter part of the 20th century, a number of medical and pseudo-medical devices were marketed to consumers as improving sexual performance or orgasms, increasing "energy", "balancing hormones", and as having other health or lifestyle benefits. There is no evidence for any of these claims, and many of them are pseudoscience.[23][24][25]
References
- "Pelvic floor muscle training exercises: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2019-02-26.
Pelvic floor muscle training exercises are a series of exercises designed to strengthen the muscles of the pelvic floor.
- "Kegel Exercises | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved 2017-12-02.

- "Pelvic floor muscle training exercises: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2017-12-02.
- La Pera, G; Nicastro, A (1996). "A new treatment for premature ejaculation: the rehabilitation of the pelvic floor". Journal of Sex & Marital Therapy. 22 (1): 22–6. doi:10.1080/00926239608405302. PMID 8699493.
- "A randomised controlled trial of the PelvicToner Device in female stress urinary incontinence". BJUI.org. Retrieved 2011-09-02.
- September 2, 2011 (2011-02-09). "Vaginal Prolapse". eMedicineHealth. Retrieved 2011-09-02.
- "MedlinePlus Medical Encyclopedia: Uterine prolapse". Nlm.nih.gov. 2011-08-29. Retrieved 2011-09-02.
- "MedlinePlus Medical Encyclopedia: Kegel exercises". Nlm.nih.gov. 2011-08-29. Retrieved 2011-09-02.
- Kenway, M., and Goh, J. (2009). Inside Out: The Essential Women's Guide to Pelvic Support.
- "Cystocele (Prolapsed Bladder) | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved 2017-12-02.
- Bø, K (2006). "Can pelvic floor muscle training prevent and treat pelvic organ prolapse?". Acta Obstet Gynecol Scand. 85 (3): 263–8. doi:10.1080/00016340500486800. PMID 16553172.
- Services, Department of Health & Human. "Pelvic floor". Retrieved 2018-02-21.
- Hagen S, Stark D (2011). "Conservative prevention and management of pelvic organ prolapse in women". Cochrane Database Syst Rev. 12 (12): CD003882. doi:10.1002/14651858.CD003882.pub4. PMID 22161382.
- Herderschee, R; Hay-Smith, EJ; Herbison, GP; Roovers, JP; Heineman, MJ (6 July 2011). "Feedback or biofeedback to augment pelvic floor muscle training for urinary incontinence in women". The Cochrane Database of Systematic Reviews (7): CD009252. doi:10.1002/14651858.CD009252. PMID 21735442.
- Puppo, Vincenzo; Puppo, Giulia (January 2016). "Comprehensive review of the anatomy and physiology of male ejaculation: Premature ejaculation is not a disease: Anatomy and Physiology of Ejaculation". Clinical Anatomy. 29 (1): 111–119. doi:10.1002/ca.22655. PMID 26457680.
- Woodley, SJ; Lawrenson, P; Boyle, R; Cody, JD; Mørkved, S; Kernohan, A; Hay-Smith, EJC (6 May 2020). "Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women". The Cochrane Database of Systematic Reviews. 5: CD007471. doi:10.1002/14651858.CD007471.pub4. PMC 7203602. PMID 32378735.
- Encyclopedia of child behavior and development. Goldstein, Sam, 1952-, Naglieri, Jack A. [New York]: Springer. 2011. ISBN 9780387790619. OCLC 704395400.CS1 maint: others (link)
- Puppo, V.; Abdulcadir, J.; Mannucci, A.; Catania, L.; Abdulcadir, D. (April 2008). "T09-P-13 The importance of the Kegel exercises for the erection of the male and female erectile organs (male and female penis)". Sexologies. 17: S136. doi:10.1016/s1158-1360(08)72894-9. ISSN 1158-1360.
- Dumoulin, Chantale; Cacciari, Licia P.; Hay-Smith, E. Jean C. (2018-10-04). "Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women". The Cochrane Database of Systematic Reviews. 10: CD005654. doi:10.1002/14651858.CD005654.pub4. ISSN 1469-493X. PMC 6516955. PMID 30288727.
- Herderschee R, Hay-Smith EJ, Herbison GP, Roovers JP, Heineman MJ (6 July 2011). "Feedback or biofeedback to augment pelvic floor muscle training for urinary incontinence in women". The Cochrane Database of Systematic Reviews (7): CD009252. doi:10.1002/14651858.CD009252. PMID 21735442.
- Anderson, Coral A.; Omar, Muhammad Imran; Campbell, Susan E.; Hunter, Kathleen F.; Cody, June D.; Glazener, Cathryn M. A. (2015-01-20). "Conservative management for postprostatectomy urinary incontinence". The Cochrane Database of Systematic Reviews. 1: CD001843. doi:10.1002/14651858.CD001843.pub5. hdl:2164/6141. ISSN 1469-493X. PMC 7025637. PMID 25602133.
- Herbison, GP; Dean, N (8 July 2013). "Weighted vaginal cones for urinary incontinence". The Cochrane Database of Systematic Reviews (7): CD002114. doi:10.1002/14651858.CD002114.pub2. PMC 7086390. PMID 23836411.
- Gunter, Jen (2017-01-17). "Dear Gwyneth Paltrow, I'm a GYN and your vaginal jade eggs are a bad idea". Dr. Jen Gunter. Retrieved 2017-03-12.
- Tuteur, Amy (18 December 2008). "Vaginal weight lifting". The Skeptical OB.
- "No, Gwyneth Paltrow, women should not put jade eggs in their vaginas, gynecologist says". Washington Post. Retrieved 6 February 2017.