Juvenile hyaline fibromatosis
Juvenile hyaline fibromatosis (also known as "Fibromatosis hyalinica multiplex juvenilis,"[2] "Murray–Puretic–Drescher syndrome"[2]) is a very rare, autosomal recessive disease due to mutations in capillary morphogenesis protein-2 (CMG-2 gene). It occurs from early childhood to adulthood, and presents as slow-growing, pearly white or skin-colored dermal or subcutaneous papules or nodules on the face, scalp, and back, which may be confused clinically with neurofibromatosis.[3]
| Juvenile hyaline fibromatosis | |
|---|---|
| Other names | Puretic syndrome[1] |
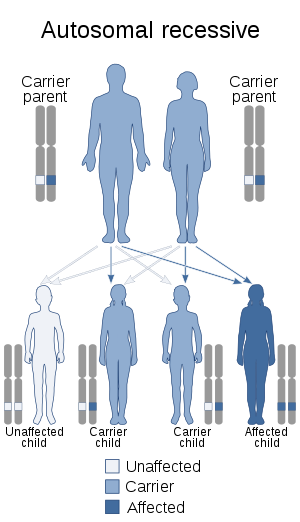 | |
| Autosomal recessive pattern is the inheritance manner of this condition | |
| Specialty | Dermatology |
Presentation
This condition is characterised by abnormal growth of hyalinized fibrous tissue with cutaneous, mucosal, osteoarticular and systemic involvement.
Clinical features include extreme pain at minimal handling in a newborn, gingival hypertrophy, subcutaneous nodules, painful joint stiffness and contractures, muscle weakness and hypotonia.
Genetics
This condition is due to mutations in the anthrax toxin receptor-2 (ANTXR2) gene. This gene is also known as capillary morphogenesis protein-2.
This gene is located on the long arm of chromosome 4 (4q21.21).
Management
There is no presently known curative treatment for this condition.
Management is supportive
Prognosis
This is very poor with a median age at death of 15 months.
Epidemiology
84 cases have been reported as of 2018.[4]
See also
- List of cutaneous conditions
References
- RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Juvenile hyaline fibromatosis". www.orpha.net. Retrieved 28 April 2019.
- Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). Page 989. McGraw-Hill. ISBN 0-07-138076-0.
- Casas-Alba D, Martínez-Monseny A, Pino-Ramírez RM, Alsina L, Castejón E, Navarro-Vilarrubí S, Pérez-Dueñas B, Serrano M, Palau F, García-Alix A (2018) Hyaline fibromatosis syndrome: Clinical update and phenotype-genotype correlations. Hum Mutat doi: 10.1002/humu.23638