Fetal adenocarcinoma
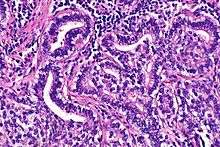
Fetal adenocarcinoma (FA) of the lung is a rare subtype of pulmonary adenocarcinoma that exhibits tissue architecture and cell characteristics that resemble fetal lung tissue upon microscopic examination. It is currently considered a variant of solid adenocarcinoma with mucin production.[1]
Symptoms
FA can produce repeated hemoptysis, possibly related to cavitation of the tumor.[2]
Other presenting symptoms described have included: flu-like syndrome with cough and fever,[3]
Genetics
Due to its rarity, little is known of the genetics of FA.[4]
One small series of 6 cases showed that MDM2 protein was expressed in 5 of them (83%), and p53 protein was overexpressed in 50%.[5] However, a larger series of 12 cases revealed no p53 gene mutations.[4]
Histogenesis
The details of the histogenesis of FA remain unknown and highly debated.[6] Adenocarcinomas are most often highly heterogeneous peripheral tumors,[7] and are thought to arise from malignant transformation of primitive cells that can exhibit differentiation characteristics of Club cells, Type II pneumocytes, bronchiolar surface cells, bronchial gland cells, or goblet cells.[8][9]
Most FA's are well or moderately differentiated tumors, although high-grade, poorly differentiated variants have been described.[1][10][11] Tissue resembling FA can also be found admixed with a component made up of primitive blastoma-like cells. In such cases, these biphasic tumors are classified as a form of pulmonary blastoma because the presence of the blastomatous cells dramatically worsens the prognosis.[11][12]
FA can occur in combination with other forms of lung cancer, particularly other variants of adenocarcinoma.[1] There also seems to be an association with clear cell lung cancer variants.[13] A case of combined small cell lung carcinoma featuring components of FA and cells resembling those from carcinoid tumor has been reported, illustrating the unique complexity and heterogeneity of divergent histogenesis and cell differentiation in lung cancer.[14]
Diagnosis
FA is an epithelial tumor whose cells and architecture resemble that of fetal lung tissues in the pseudoglandular stage of development (which occurs at about 10–16 weeks gestation in the human),[6] with complex glandular structures and morules with cell nuclei that appear clear due to the accumulation of biotin.[15]
While FA can be diagnosed via biopsy, bronchial brushings, and immunocytochemistry,[16] examination of the whole tumor is required to rule out biphasic pulmonary blastoma, a mixed tumor of higher aggressiveness, wherein FA occurs admixed with primitive blastoma cells.[6]
Although it is not normally considered a fast-growing malignant neoplasm, FA can exhibit high uptake on FDG-PET scanning.[17]
Identification of aberrant nuclear localization of a mutated protein product of the beta-catenin gene has been proposed as a diagnostic tool for FA.[18]
Although FA's usually occur as nodules or masses, they can sometimes present as a multifocal disease.[19]
Treatment
Because of its extreme rarity, there have been no controlled clinical trials of treatment regimens for FA and, as a result, there are no evidence-based treatment guidelines.[6] Complete surgical resection is the treatment of choice in FA, as it is in nearly all forms of lung cancer.[20]
Anecdotal reports suggest that FA is rarely highly sensitive to cytotoxic drugs[20] or radiation.[2] Case reports suggest that chemotherapy with UFT may be useful in FA.[13]
Prognosis
The prognosis of patients with FA as a whole is considered to be better than that of most other forms of non-small cell carcinoma, including biphasic pulmonary blastoma.[21][22]
Incidence
FA is a rare tumor, with a relative incidence estimated to be no more than 0.5% of all lung cancers.[2][23][24][6]
FA is exceptionally rare in children, with only a handful of cases reported to date,[25] However, several case reports have involved FA's in pregnant women or the early postnatal period.[2][24]
Synonyms
Synonyms for FA include well differentiated fetal adenocarcinoma, high-grade fetal adenocarcinoma, pulmonary adenocarcinoma of fetal type, and pulmonary endodermal tumour resembling fetal lung.[1]
References
- Travis, William D; Brambilla, Elisabeth; Muller-Hermelink, H Konrad; et al., eds. (2004). Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart (PDF). World Health Organization Classification of Tumours. Lyon: IARC Press. ISBN 92-832-2418-3. Archived from the original (PDF) on 23 August 2009. Retrieved 14 April 2012.
- Thompson RJ, Hasleton PS, Taylor PM, Woodhead M, Byrd LM (2010). "Haemoptysis in pregnancy caused by a well-differentiated fetal adenocarcinoma: a case report". J Med Case Rep. 4: 17. doi:10.1186/1752-1947-4-17. PMC 2823759. PMID 20205788.
- Longo M, Levra MG, Capelletto E, et al. (April 2008). "Fetal adenocarcinoma of the lung in a 25-year-old woman". J Thorac Oncol. 3 (4): 441–3. doi:10.1097/JTO.0b013e318169cd9a. hdl:2318/27869. PMID 18379367.
- Bodner SM, Koss MN (November 1996). "Mutations in the p53 gene in pulmonary blastomas: immunohistochemical and molecular studies". Hum. Pathol. 27 (11): 1117–23. doi:10.1016/S0046-8177(96)90302-0. PMID 8912818.
- Pacinda SJ, Ledet SC, Gondo MM, et al. (June 1996). "p53 and MDM2 immunostaining in pulmonary blastomas and bronchogenic carcinomas". Hum. Pathol. 27 (6): 542–6. doi:10.1016/S0046-8177(96)90159-8. PMID 8666362.
- Cutler CS, Michel RP, Yassa M, Langleben A (February 1998). "Pulmonary blastoma: case report of a patient with a 7-year remission and review of chemotherapy experience in the world literature". Cancer. 82 (3): 462–7. doi:10.1002/(sici)1097-0142(19980201)82:3<462::aid-cncr6>3.0.co;2-r. PMID 9452262.
- Roggli VL, Vollmer RT, Greenberg SD, McGavran MH, Spjut HJ, Yesner R (June 1985). "Lung cancer heterogeneity: a blinded and randomized study of 100 consecutive cases". Hum. Pathol. 16 (6): 569–79. doi:10.1016/S0046-8177(85)80106-4. PMID 2987102.
- Shimosato Y, Kodama T, Kameya T (1982). "Morphogenesis of peripheral type adenocarcinoma of the lung". In Shimosato Y, Melamed MR, Nettesheim P (eds.). Morphogenesis of lung cancer. Boca Raton FL: CRC Press. pp. 65–89.
- Gupta K, Joshi K, Jindal SK, Rayat CS (2008). "Spectrum of pulmonary adenocarcinoma with ultrastructural correlation: an autopsy study from northern India". Indian J Pathol Microbiol. 51 (3): 329–36. doi:10.4103/0377-4929.42505. PMID 18723952.
- Kadota K, Haba R, Katsuki N, et al. (October 2010). "Bronchial brushing cytology of a pulmonary fetal adenocarcinoma with a poorly differentiated component". Cytopathology. 21 (5): 349–51. doi:10.1111/j.1365-2303.2009.00724.x. PMID 20015256.
- Nakatani Y, Kitamura H, Inayama Y, et al. (April 1998). "Pulmonary adenocarcinomas of the fetal lung type: a clinicopathologic study indicating differences in histology, epidemiology, and natural history of low-grade and high-grade forms". Am. J. Surg. Pathol. 22 (4): 399–411. doi:10.1097/00000478-199804000-00003. PMID 9537466.
- Adluri RK, Boddu SR, Martin-Ucar A, Duffy JP, Beggs FD, Morgan WE (February 2006). "Pulmonary blastoma—a rare tumor with variable presentation". Eur J Cardiothorac Surg. 29 (2): 236–9. doi:10.1016/j.ejcts.2005.11.035. PMID 16387506.
- Matsuoka T, Sugi K, Matsuda E, et al. (August 2006). "[Clear cell adenocarcinoma with acomponent of well-differentiated fetal adenocareinoma; report of a case]". Kyobu Geka (in Japanese). 59 (9): 867–70. PMID 16922450.
- Mardini G, Pai U, Chavez AM, Tomashefski JF (March 1994). "Endobronchial adenocarcinoma with endometrioid features and prominent neuroendocrine differentiation. A variant of fetal adenocarcinoma". Cancer. 73 (5): 1383–9. doi:10.1002/1097-0142(19940301)73:5<1383::aid-cncr2820730512>3.0.co;2-v. PMID 8111705.
- Nakatani Y, Masudo K, Miyagi Y, et al. (June 2002). "Aberrant nuclear localization and gene mutation of beta-catenin in low-grade adenocarcinoma of fetal lung type: up-regulation of the Wnt signaling pathway may be a common denominator for the development of tumors that form morules". Mod. Pathol. 15 (6): 617–24. doi:10.1038/modpathol.3880575. PMID 12065775.
- Odashiro DN, Nguyen GK (April 2006). "Pulmonary well-differentiated fetal adenocarcinoma diagnosed by bronchial brush and immunocytochemistry". Diagn. Cytopathol. 34 (4): 308–10. doi:10.1002/dc.20409. PMID 16544342.
- Paull DE, Moezzi J, Katz N, Little AG, Adebonojo SA (April 2006). "Positron emission tomography in well differentiated fetal adenocarcinoma of the lung". Clin Nucl Med. 31 (4): 213–4. doi:10.1097/01.rlu.0000204131.93846.39. PMID 16550018.
- Proctor L, Folpe AL, Esper A, Wolfenden LL, Force S, Logani S (January 2007). "Well-differentiated fetal adenocarcinoma of the lung: cytomorphologic features on fine-needle aspiration with emphasis on use of beta-catenin as a useful diagnostic marker". Diagn. Cytopathol. 35 (1): 39–42. doi:10.1002/dc.20583. PMID 17173289.
- Furuya K, Yasumori K, Takeo S, et al. (2008). "Well-differentiated fetal adenocarcinoma of the lung: early-phase sequential high-resolution computed tomographic findings". J Comput Assist Tomogr. 32 (5): 806–9. doi:10.1097/RCT.0b013e3181573e98. PMID 18830116.
- Fujino S, Asada Y, Konishi T, Asakura S, Kato H, Mori A (December 1995). "Well-differentiated fetal adenocarcinoma of lung". Lung Cancer. 13 (3): 311–6. doi:10.1016/0169-5002(95)00489-0. PMID 8719071.
- Sato S, Koike T, Yamato Y, Yoshiya K, Honma K, Tsukada H (December 2006). "Resected well-differentiated fetal pulmonary adenocarcinoma and summary of 25 cases reported in Japan". Jpn. J. Thorac. Cardiovasc. Surg. 54 (12): 539–42. doi:10.1007/s11748-006-0048-8. PMID 17236658.
- Rossi G, Marchioni A, Sartori G, Longo L, Piccinini S, Cavazza A (2007). "Histotype in non-small cell lung cancer therapy and staging: The emerging role of an old and underrated factor". Curr Resp Med Rev. 3: 69–77. doi:10.2174/157339807779941820.
- Luo DL, Liu YH, Zhuang HG, et al. (November 2008). "[Clinicopathologic study of pulmonary adenocarcinoma with features of bronchioloalveolar carcinoma]". Zhonghua Bing Li Xue Za Zhi (in Chinese). 37 (11): 737–42. PMID 19094707.
- Esper A, Force S, Gal A, Wolfenden LL (November 2006). "A 36-year-old woman with hemoptysis and a lung mass 3 months after delivery". Chest. 130 (5): 1620–3. doi:10.1378/chest.130.5.1620. PMID 17099047.
- DiFurio MJ, Auerbach A, Kaplan KJ (2003). "Well-differentiated fetal adenocarcinoma: rare tumor in the pediatric population". Pediatr. Dev. Pathol. 6 (6): 564–7. doi:10.1007/s10024-003-4046-x. PMID 15018457.
External links
- "Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart". World Health Organization Classification of Tumours. (Download Page).