Cardiotocography
Cardiotocography (CTG) is a technical means of recording the fetal heartbeat and the uterine contractions during pregnancy. The machine used to perform the monitoring is called a cardiotocograph, more commonly known as an electronic fetal monitor (EFM).
| Cardiotocography | |
|---|---|
 A cardiotocograph recording fetal heart rate and uterine contractions | |
| ICD-9-CM | 75.32 |
| MeSH | D015148 |
Fetal monitoring was invented by Doctors Alan Bradfield, Orvan Hess and Edward Hon. A refined (antepartal, non-invasive, beat-to-beat) version (cardiotocograph) was later developed for Hewlett Packard by Konrad Hammacher.
CTG monitoring is widely used to assess fetal wellbeing.[1] A review found that in the antenatal period (before labour) there is no evidence to suggest that monitoring women with high-risk pregnancies benefits the mother or baby although research around this is old and should be interpreted with caution.[1] The same review found that computerised CTG machines resulted in lower numbers of baby deaths than the traditional CTG machines (as shown in picture). More up-to-date research is needed to provide more information around this practice.[1]
CTG monitoring can sometimes lead to medical interventions which are not necessarily needed.[1] Fetal vibroacoustic stimulation (sound played to the unborn baby through the mother's abdomen) has been used to provoke the baby into being more active.[2] This can improve their CTG monitoring so that the mother does not have to be monitored for as long.[2] However the safety of this technique has not been fully assessed; hearing impairment, stress reactions and other effects should be investigated before this technique is used widely.[2]
Method

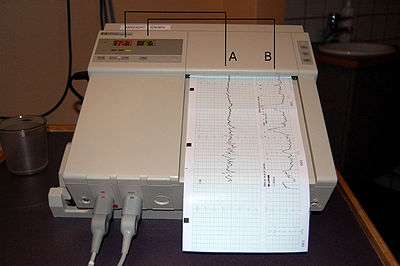
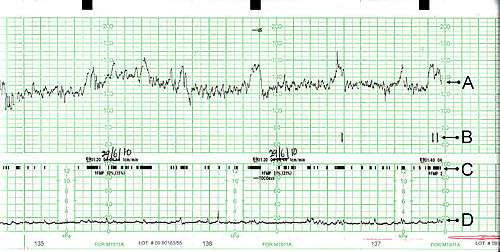
External Cardiotocography can be used for continuous or intermittent monitoring. The fetal heart rate and the activity of the uterine muscle are detected by two transducers placed on the mother's abdomen (one above the fetal heart, to monitor heart rate and the other at the fundus of the uterus to measure frequency of contractions). Doppler ultrasound provides the information which is recorded on a paper strip known as a cardiotocograph (CTG).[3] External tocometry is useful in showing the beginning and end of contractions, as well as frequency, but not the strength of contractions. The absolute values of pressure readings on an external tocometer are dependent on position, and are not sensitive in people who are obese.[4] In cases where information on the strength, or precise timing, of contractions is needed, an internal tocometer is more appropriate.[4]
Internal Cardiotocography uses an electronic transducer connected directly to the fetal scalp. A wire electrode is attached to the fetal scalp through the cervical opening and is connected to the monitor. This type of electrode is sometimes called a spiral or scalp electrode. Internal monitoring provides a more accurate and consistent transmission of the fetal heart rate than external monitoring because factors such as movement do not affect it. Internal monitoring may be used when external monitoring of the fetal heart rate is inadequate, or closer surveillance is needed.[5] Internal tocometry can only be used if membranes (fore-waters) have ruptured either spontaneously or artificially, and the cervix is open. To gauge the strength of contractions, a small catheter (Intrauterine pressure catheter or IUPC) is passed into the uterus, past the fetus. Combined with an internal fetal monitor, an IUPC may give a more precise reading of the baby's heart rate and the strength of contractions.
A typical CTG reading is printed on paper and/or stored on a computer for later reference. A variety of systems for centralized viewing of CTG have been installed in a large number of maternity hospitals in industrialised countries, allowing simultaneous monitoring of multiple tracings in one or more locations. Display of maternal vital signs, ST signals and an electronic Partogram are available in the majority of these systems. A few of them have incorporated computer analysis of cardiotocographic signals or combined cardiotocographic and ST data analysis.[6][7][8][3]
Interpretation
In the US, the Eunice Kennedy Shriver National Institute of Child Health and Human Development sponsored a workshop to develop a standardized nomenclature for use in interpreting Intrapartum fetal heart rate and uterine contraction patterns. This nomenclature has been adopted by the Association of Women's Health, Obstetric, and Neonatal Nurses (AWHONN), the American College of Obstetricians and Gynecologists (ACOG), and the Society for Maternal-Fetal Medicine.[9]
The Royal College of Obstetricians and Gynaecologists[10] and the Society of Obstetricians and Gynaecologists of Canada[11] have also published consensus statements on standardized nomenclature for fetal heart rate patterns.
Interpretation of a CTG tracing requires both qualitative and quantitative description of:
- Uterine activity (contractions)
- Baseline fetal heart rate (FHR)
- Baseline FHR variability
- Presence of accelerations
- Periodic or episodic decelerations
- Changes or trends of FHR patterns over time.
Uterine Activity
There are several factors used in assessing uterine activity.
- Frequency- the amount of time between the start of one contraction to the start of the next contraction.
- Duration- the amount of time from the start of a contraction to the end of the same contraction.
- Intensity- a measure of how strong a contraction is. With external monitoring, this necessitates the use of palpation to determine relative strength. With an IUPC, this is determined by assessing actual pressures as graphed on the paper.
- Resting Tone- a measure of how relaxed the uterus is between contractions. With external monitoring, this necessitates the use of palpation to determine relative strength. With an IUPC, this is determined by assessing actual pressures as graphed on the paper
- Interval- the amount of time between the end of one contraction to the beginning of the next contraction.
The NICHD nomenclature[9] defines uterine activity by quantifying the number of contractions present in a 10-minute window, averaged over 30 minutes. Uterine activity may be defined as:
- Normal- less than or equal to 5 contractions in 10 minutes, averaged over a 30-minute window
- Tachysystole- more than 5 contractions in 10 minutes, averaged over a 30-minute window
Baseline fetal heart rate
The NICHD nomenclature[9] defines baseline fetal heart rate as: The baseline FHR is determined by approximating the mean FHR rounded to increments of 5 beats per minute (bpm) during a 10-minute window, excluding accelerations and decelerations and periods of marked FHR variability (greater than 25 bpm). There must be at least 2 minutes of identifiable baseline segments (not necessarily contiguous) in any 10-minute window, or the baseline for that period is indeterminate. In such cases, it may be necessary to refer to the previous 10-minute window for determination of the baseline. Abnormal baseline is termed bradycardia when the baseline FHR is less than 110 bpm; it is termed tachycardia when the baseline FHR is greater than 160 bpm.
Baseline FHR variability
Moderate baseline fetal heart rate variability reflects the delivery of oxygen to the fetal central nervous system. Its presence is reassuring in predicting an absence of metabolic acidemia and hypoxic injury to the fetus at the time it is observed.[9] In contrast, the presence of mild baseline FHR variability, or an absence of FHR variability does not reliably predict fetal acidemia or hypoxia; lack of moderate baseline FHR variability may be a result of the fetal sleep cycle, or a result of medications, extreme prematurity, congenital anomalies, or pre-existing neurological injury.[9]
The NICHD nomenclature[9] defines baseline FHR variability as: Baseline FHR variability is determined in a 10-minute window, excluding accelerations and decelerations. Baseline FHR variability is defined as fluctuations in the baseline FHR that are irregular in amplitude and frequency. The fluctuations are visually quantitated as the amplitude of the peak-to-trough in beats per minute. Using this definition, the baseline FHR variability is categorized by the quantitated amplitude as:
- Absent- undetectable
- Minimal- greater than undetectable, but less than or equal to 5 beats per minute
- Moderate- 6-25 beats per minute
- Marked- greater than 25 beats per minute
Saltatory pattern of fetal heart rate
Saltatory pattern of fetal heart rate is defined in cardiotocography (CTG) guidelines by FIGO (The International Federation of Gynaecology and Obstetrics) and NICE (The National Institute for Health and Care Excellence) as fetal heart rate (FHR) baseline amplitude changes of more than 25 beats per minute (bpm).[12][13]
In a 1992 study, the saltatory pattern FHR was defined by O'Brien-Abel and Benedetti as:
Fetal heart baseline amplitude changes of greater than 25 bpm with an oscillatory frequency of greater the 6 per minutes for a minimum duration of 1 minute.[14]
The pathophysiology of saltatory pattern is not well-known.[12][13] It has been linked with rapidly progressing hypoxia[15] for example due to an umbilical cord compression, and it is presumed to be caused by an instability of fetal central nervous system.[12]
In a study by Nunes et al. (2014),[16] four saltatory patterns exceeding in CTG more than 20 minutes in the last 30 minutes before birth were associated with fetal metabolic acidosis. According to this study, saltatory pattern is relatively rare condition, thus only four cases were found from three large databases.
In a recent study by Tarvonen et al. (2019),[17] it was demonstrated that the occurrence of saltatory pattern, already with minimum duration of 2 minutes, in CTG tracings during labor was associated with fetal hypoxia indicated by high umbilical vein (UV) blood erythropoietin (EPO) levels and umbilical artery (UA) blood acidosis at birth in human fetuses. As saltatory patterns preceded late decelerations of fetal heart rate (FHR) in the majority of cases, saltatory pattern seems to be an early sign of fetal hypoxia.[18] According to the authors, awareness on this gives obstetricians and midwives time to intensify electronic fetal monitoring and to plan possible interventions before fetal asphyxia occurs.[19]
Accelerations
The NICHD nomenclature[9] defines an acceleration as a visually apparent abrupt increase in fetal heart rate. An abrupt increase is defined as an increase from the onset of acceleration to the peak in less than or equal to 30 seconds. To be called an acceleration, the peak must be greater than or equal to 15 bpm, and the acceleration must last greater than or equal to 15 seconds from the onset to return to baseline.[20] A prolonged acceleration is greater than or equal to 2 minutes but less than 10 minutes in duration. An acceleration lasting greater than or equal to 10 minutes is defined as a baseline change. Before 32 weeks of gestation, accelerations are defined as having a peak greater than or equal to 10 bpm and a duration of greater than or equal to 10 seconds.
Periodic or episodic decelerations
Periodic refers to decelerations that are associated with contractions; episodic refers to those not associated with contractions. There are four types of decelerations as defined by the NICHD nomenclature, all of which are visually assessed.[9]
- Early Decelerations are a result of increased vagal tone due to compression of the fetal head during contractions. Monitoring usually shows a symmetrical, gradual decrease and return to baseline of FHR which is associated with a uterine contraction. A 'gradual' deceleration has a time from onset to nadir of 30 seconds or more. Early decelerations begin and end at approximately the same time as contractions, and the low point of the fetal heart rate occurs at the peak of the contraction.[4]
- Late Decelerations are a result of placental insufficiency, which can result in fetal distress. Monitoring usually shows symmetrical gradual decrease and return to baseline of the fetal heart rate in association with a uterine contraction. A 'gradual' deceleration has onset to nadir of 30 seconds or more. In contrast to early deceleration, the low point of fetal heart rate occurs after the peak of the contraction, and returns to baseline after the contraction is complete.[4]
- Variable Decelerations are generally a result of umbilical cord compression, and contractions may further compress a cord when it is trapped around the neck or under the shoulder of the fetus. They are defined as abrupt decreases in fetal heart rate, with less than 30 seconds from the beginning of the decrease to the nadir of heart rate. The decrease in FHR is greater than or equal to 15 beats per minute, lasting greater than or equal to 15 seconds, and less than 2 minutes in duration.[4] When variable decelerations are associated with uterine contractions, their onset, depth, and duration commonly vary with successive uterine contractions.
- Prolonged Deceleration: Decrease in FHR from baseline greater than or equal to 15 bpm, lasting greater than or equal to 2 minutes, but less than 10 minutes. A deceleration greater than or equal to 10 minutes is a baseline change.
Additionally, decelerations can be recurrent or intermittent based on their frequency (more or less than 50% of the time) within a 20 min window.[9]
FHR pattern classification
Before 2008, fetal heart rate was classified as either "reassuring" or "nonreassuring". The NICHD workgroup proposed terminology of a three-tiered system to replace the older, undefined terms.[9]
- Category I (Normal): Tracings with all these findings present are strongly predictive of normal fetal acid-base status at the time of observation and the fetus can be followed in a standard manner:
- Baseline rate 110-160 bpm,
- Moderate variability,
- Absence of late, or variable decelerations,
- Early decelerations and accelerations may or may not be present.
- Category II (Indeterminate): Tracing is not predictive of abnormal fetal acid-base status, but evaluation and continued surveillance and reevaluations are indicated.
- Bradycardia with normal baseline variability
- Tachycardia
- Minimal or Marked baseline variability of FHR
- Accelerations: Absence of induced accelerations after fetal stimulation
- Periodic or Episodic decelerations: Longer than 2min but shorter than 10min; Recurrent late decelerations with moderate baseline variability
- Variable decelerations with other characteristics such as slow return to baseline, overshoots of "shoulders" seen (humps on either side of deceleration)
- Category III (Abnormal): Tracing is predictive of abnormal fetal acid-base status at the time of observation; this requires prompt evaluation and management:
- Absence of baseline variability, with recurrent late or variable decelerations, or bradycardia; or
- Sinusoidal fetal heart rate
Updated 2015 FIGO Intrapartum Fetal Monitoring Guidelines
FIGO has recently modified the guidelines on intrapartum fetal monitoring, proposing following interpretation:[21]
- Normal: No hypoxia/acidosis, no intervention necessary to improve fetal oxygenation state:
- Baseline 110-160 bpm
- Variability 5-25 bpm
- No repetitive decelerations (decelerations are defined as repetitive when associated with > 50% contractions)
- Suspicious: Low probability of hypoxia/acidosis, warrants action to correct reversible causes if identified, close monitoring or adjunctive methods:
- Lacking at least one characteristic of normality, but with no pathological features.
- Pathological: High probability of hypoxia/acidosis, requires immediate action to correct reversible causes, adjunctive methods, or if this is not possible expedite delivery. In acute situations immediate delivery should be accomplished
- Baseline <100 bpm
- Reduced or increased variability or sinusoidal pattern
- Repetitive late or prolonged decelerations for > 30 min, or > 20 min if reduced variability (decelerations are defined as repetitive when associated with > 50% contractions)
- Deceleration > 5 min
Benefits
According to the Cochrane review from the February 2017, CTG was associated with fewer neonatal seizures but it is unclear if it had any impact on long-term neurodevelopmental outcomes. No clear differences in cerebral palsy, infant mortality or other standard measures of neonatal wellbeing, neither on any meaningful long-term outcomes could be shown. Continuous CTG was associated with the higher rates of caesarean sections and instrumental vaginal births. The authors see the challenge in how to discuss these results with women to enable them to make an informed decision without compromising the normality of labour. Future research should focus on events that happen in pregnancy and labour that could be the cause of long-term problems for the baby.[3]
References
- Grivell, Rosalie M; Alfirevic, Zarko; Gyte, Gillian ML; Devane, Declan; Grivell, Rosalie M (2015). "Antenatal cardiotocography for fetal assessment". The Cochrane Database of Systematic Reviews (9): CD007863. doi:10.1002/14651858.CD007863.pub4. PMC 6510058. PMID 26363287.
- Tan, Kelvin H; Smyth, Rebecca MD; Wei, Xing; Tan, Kelvin H (2013). "Fetal vibroacoustic stimulation for facilitation of tests of fetal wellbeing". The Cochrane Database of Systematic Reviews (12): CD002963. doi:10.1002/14651858.CD002963.pub2. PMID 24318543.
- Alfirevic, Zarko; Devane, Declan; Gyte, Gillian Ml; Cuthbert, Anna (3 February 2017). "Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour". The Cochrane Database of Systematic Reviews. 2: CD006066. doi:10.1002/14651858.CD006066.pub3. ISSN 1469-493X. PMC 6464257. PMID 28157275.
- Callahan, Tamara (2013). Blueprints obstetrics & gynecology. Baltimore, MD: Lippincott Williams & Wilkins. pp. 43–47. ISBN 978-1-4511-1702-8.
- "Types of Fetal Heart Monitoring". www.hopkinsmedicine.org. Retrieved 21 March 2018.
- Nunes, Inês; Ayres-de-Campos, Diogo; Figueiredo, Catarina; Bernardes, João (2013). "An overview of central fetal monitoring systems in labour". Journal of Perinatal Medicine. 41 (1): 93–9. doi:10.1515/jpm-2012-0067. PMID 23093259.
- "Procedures That May Take Place During Labor and Delivery".
- Neilson, J (1993). "Cardiotocography during labour". BMJ. 306 (6874): 347–8. doi:10.1136/bmj.306.6874.347. PMC 1676479. PMID 8461676.
- Macones, George A.; Hankins, Gary D.V.; Spong, Catherine Y.; Hauth, John; Moore, Thomas (2008). "The 2008 National Institute of Child Health and Human Development Workshop Report on Electronic Fetal Monitoring". Obstetrics & Gynecology. 112 (3): 661–6. doi:10.1097/AOG.0b013e3181841395. PMID 18757666. S2CID 1884812.
- NICE Guideline Intrapartum care: management and delivery of care to women in labour Archived July 27, 2011, at the Wayback Machine
- SOGC Fetal health Surveillance: antepartum and intrapartum Consensus Guideline Archived November 29, 2010, at the Wayback Machine
- Ayres-de-Campos, Diogo; Spong, Catherine Y.; Chandraharan, Edwin; FIGO Intrapartum Fetal Monitoring Expert Consensus Panel (October 2015). "FIGO consensus guidelines on intrapartum fetal monitoring: Cardiotocography". International Journal of Gynaecology and Obstetrics. 131 (1): 13–24. doi:10.1016/j.ijgo.2015.06.020. ISSN 1879-3479. PMID 26433401.
- "NICE/RCOG CTG Guidelines 2017".
- O'Brien-Abel, N. E.; Benedetti, T. J. (March 1992). "Saltatory Fetal Heart Rate Pattern". Journal of Perinatology. 12 (1): 13–17. ISSN 0743-8346. PMID 1560284.
- Chandraharan, Niraj Yanamandra and Edwin (2013-07-31). "Saltatory and Sinusoidal Fetal Heart Rate (FHR) Patterns and significance of FHR 'Overshoots'". Current Women`s Health Reviews. Retrieved 2019-12-31.
- Nunes, I.; Ayres-de-Campos, D.; Kwee, A.; Rosén, K. G. (2014). "Prolonged saltatory fetal heart rate pattern leading to newborn metabolic acidosis". Clinical and Experimental Obstetrics & Gynecology. 41 (5): 507–511. ISSN 0390-6663. PMID 25864248.
- Tarvonen, Mikko; Sainio, Susanna; Hämäläinen, Esa; Hiilesmaa, Vilho; Andersson, Sture; Teramo, Kari (2019-12-17). "Saltatory Pattern of Fetal Heart Rate during Labor Is a Sign of Fetal Hypoxia". Neonatology. 117 (1): 111–117. doi:10.1159/000504941. ISSN 1661-7819. PMID 31846958.
- https://www.karger.com/Article/Abstract/504941
- https://www.researchgate.net/publication/337992988_Saltatory_Pattern_of_Fetal_Heart_Rate_during_Labor_Is_a_Sign_of_Fetal_Hypoxia/stats
- Bailey, RE (2009). "Intrapartum fetal monitoring". American Family Physician. 80 (12): 1388–96. PMID 20000301.
- "Available to view: FIGO Intrapartum Fetal Monitoring Guidelines | FIGO". www.figo.org. Retrieved 2017-06-26.